The Cardiovascular System
Objectives
1. Describe the normal anatomy and physiology of the cardiovascular system.
2. Discuss the risk factors and incidence of cardiovascular disease.
3. Explain ways to modify risk factors for the development of cardiovascular disease.
4. State ways in which nurses can contribute to the prevention of cardiovascular disease.
Key Terms
arteriosclerosis (ăr-tē-rē-ō-sklĕ-RŌ-sĭs, p. 375)
atherosclerosis (ăth-ĕr-ō-sklĕ-RŌ-sĭs, p. 374)
cardiac output (p. 373)
cardiomyopathy (kăr-dē-ō-mī-ŎP-ăth-ē, p. 385)
cellulitis (sĕl-ū-LĬ-tĭs, p. 388)
coarctation (kō-ărk-TĀ-shŭn, p. 375)
dysrhythmia (dĭs-RĬTH-mē-ă, p. 375)
ejection fraction (p. 373)
endocarditis (ĔN-dō-kăhr-DĪ-tĭs, p. 376)
hypertension (hī-pĕr-TĔN-shŭn, p. 375)
infarct (p. 375)
intermittent claudication (ĭn-tĕr-MĬT-ĕnt klăw-dĭ-KĀ-shŭn, p. 385)
ischemia (ĭs-KĒ-mē-ă, p. 375)
palpitations (păl-pĭ-TĀ-shŭnz, p. 394)
pericarditis (pĕr-ē-kăhr-DĪ-tĭs, p. 376)
rubor (rū-bŏr, p. 388)
stroke volume (p. 373)
syncope (SĬN-kō-pē, p. 387)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Overview of Anatomy and Physiology of the Cardiovascular System
What are the Structures of the Heart and their Functions?
• A membranous sac, the pericardium, surrounds the heart.
• The pericardial space contains a thin layer of fluid (5 to 20 mL).
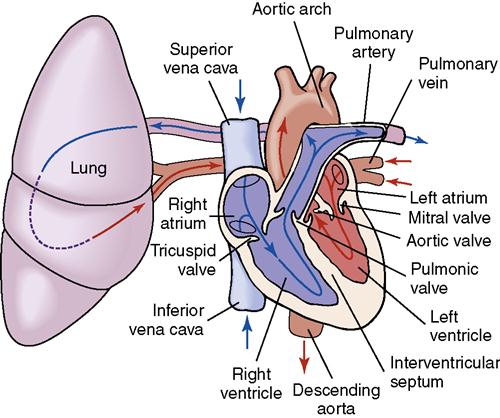
• The left atrium and left ventricle receive oxygenated blood from the lungs and pump it through the systemic circulation (Figure 18-1).
• A septum separates the right and left sides of the heart.
• The cardiac valves direct the flow of blood through the heart chambers.
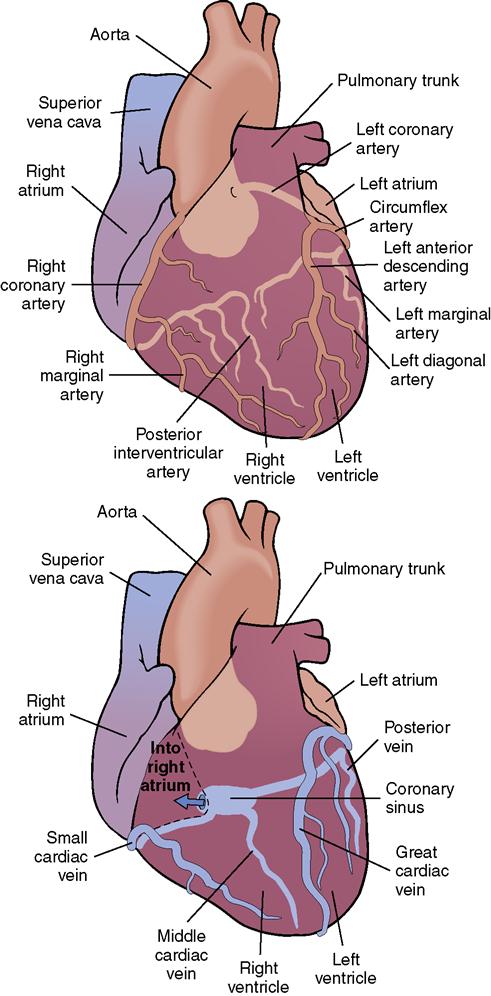
• The coronary arteries branch from the aorta and supply the cardiac muscle with blood (Figure 18-2).
• The right coronary artery supplies the right atrium, right ventricle, and part of the posterior wall of the left ventricle, as well as the atrioventricular node of the cardiac conduction system (see Figure 18-2).
• The heart is located within the mediastinum and is tilted forward and to the left side of the chest.
What Causes the Heart to Contract and Pump Blood?
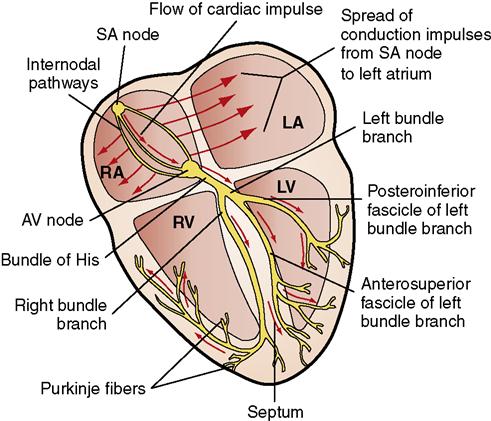
• The atrioventricular (AV) node is located in the lower part of the right atrium. It relays the impulse from the SA node to the bundle of His and throughout the ventricles via the Purkinje fibers (Figure 18-3).
What is the Cardiac Cycle?
What is the Ejection Fraction?
• The ejection fraction is the percentage of blood that is ejected from the heart during systole.
• A normal ejection fraction is 50% to 70%.
• As ejection fraction decreases with heart failure, tissue perfusion diminishes.
• A decreased ejection fraction causes backup of blood into the pulmonary vessels.
• Too much blood and the increased pressure in the pulmonary vessels can cause pulmonary edema.
• Stroke volume equals the amount of blood ejected by a ventricle during contraction.
• Cardiac output equals stroke volume multiplied by the heart rate.
How does the Vascular System Function to Carry Blood Throughout the Body?
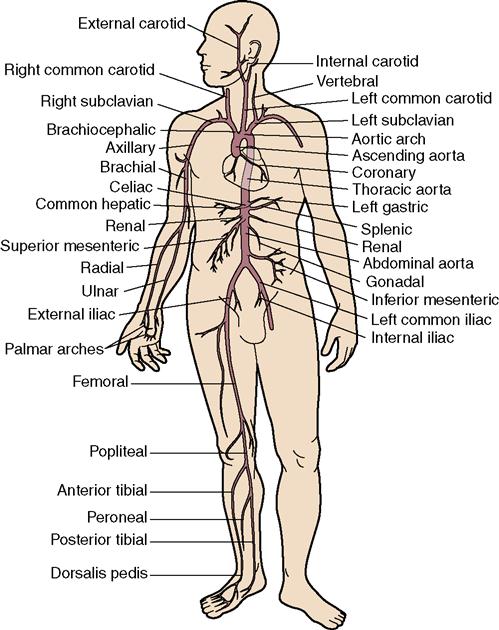
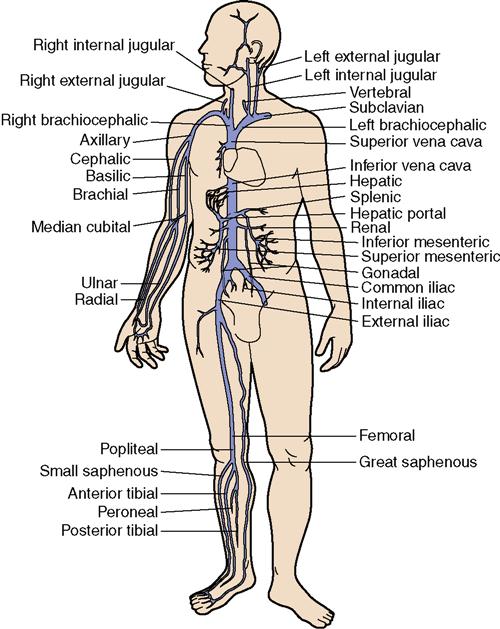
• Arteries carry oxygenated blood away from the heart (Figure 18-4). Veins carry oxygen-depleted blood back to the heart for reoxygenation by the lungs (Figure 18-5).
• Small veins, venules, and small arteries, arterioles, are connected by the capillaries.
• The aorta is the largest artery in the body, and it receives blood from the left ventricle.
• Arteries are elastic and accommodate changes in blood flow by constricting or dilating.
• Sets of valves in the medium and large veins open and close, keeping blood flowing toward the heart.
What is the Blood Pressure and what Affects it?
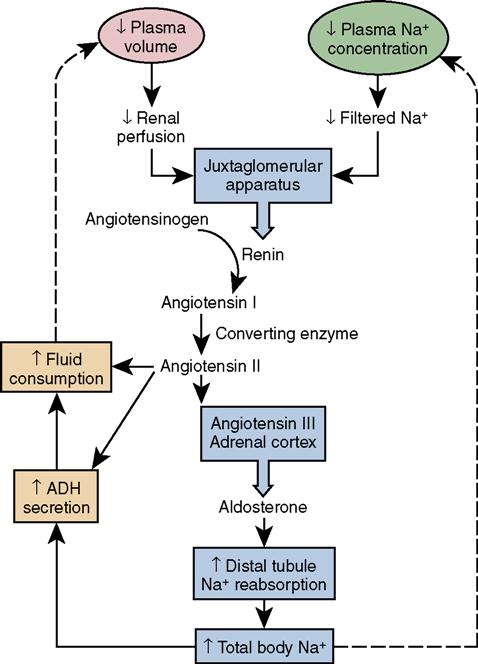
• If blood volume decreases, the kidneys secrete the enzyme renin in the blood (Figure 18-6).
• Renin acts on certain blood proteins to produce angiotensin I.
• Angiotensin I is converted to angiotensin II by the angiotensin-converting enzyme from the lungs.
• Blood flow is affected by the amount of resistance in the vessels and by the viscosity of the blood.
What Changes Occur in the Cardiovascular System with Aging?
Cardiovascular Disease
Cardiovascular disease (CVD) affects one in three people in the United States, and more than 800,000 people die in the United States as a result of cardiovascular problems each year. Cardiovascular disease is responsible for the largest portion of Medicare funds spent each year. Together with the heart, the vascular system provides the body with nutrients and oxygen needed for life. The vascular system also transports metabolic wastes that are excreted by the lungs and the kidneys. When a disorder of the cardiovascular system occurs, homeostasis is upset. Many of the disorders that afflict the cardiovascular system can be prevented or controlled.
Women and Heart Disease
Heart disease in women has been increasing. Nearly 42 million women live with heart disease. It is the number one killer of women. Low blood levels of “good” cholesterol (high-density lipoprotein [HDL]) appear to be a stronger predictor of heart disease in women than in men, particularly in the over-65 age group. High blood levels of triglycerides are another particular risk factor in women. Although it was once thought that postmenopausal hormone replacement therapy (HRT) was heart protective, it was discovered that there were more cardiovascular events in women who were on HRT (Hlatky et al., 2002). Women with CVD may experience subtle symptoms such as shortness of breath, fatigue, or changes in sleep patterns.
Causes of cardiovascular disorders
Causes of cardiovascular disorders can be congenital or acquired. Narrowing of the aorta (coarctation), holes in the septum, or abnormal formation of a cardiac valve can occur congenitally. Acquired defects include narrowing or hardening of the blood vessels from arteriosclerosis (thickening and loss of elasticity) or atherosclerosis and aneurysms of the large vessels. Inflammation of the valve structure may cause narrowing (stenosis) or incomplete closure (insufficiency) of the valve. Alteration of the myocardial muscle tissue by extra growth with thickening (hypertrophy) or fibrosis may occur as a result of systemic hypertension (persistently elevated blood pressure), pulmonary hypertension, or valve problems. Lack of adequate blood supply (ischemia) or infarct (area of tissue that has died from lack of blood supply) may occur from coronary artery stenosis. Deterioration of the pacemaker cells and conduction fibers related to hypertrophy or inflammation of tissues may cause conduction disorders.
Several disorders involving either the heart or the vessels through which it pumps blood can eventually weaken and damage the heart muscle and lead to pump failure. This condition, called heart failure, is a complication of many cardiovascular diseases, as discussed in the following chapters.
Disturbances in any part of the heart’s conduction system can result in an increase in heart rate (tachycardia), a slowing down of the heart rate (bradycardia), and disturbances in the rhythm of the heartbeat (dysrhythmias).
Infection and inflammation also can take their toll on the structure and function of the heart. Endocarditis, inflammation within the lining and valves of the heart, and pericarditis, an inflammation of the sac surrounding the heart, can occur as primary diseases, but they are more often secondary to infection and inflammation elsewhere in the body. An example is rheumatic heart disease, which occurs after a streptococcal infection.
Substances in the blood, such as excess carbon dioxide and certain drugs, can affect the rate and rhythm of the heart through their effect on the autonomic nervous system. The heart also responds to physiologic changes that indicate a need for more or less oxygen.
The arterial walls can be injured by several factors. Hypertension causes a mechanical injury by applying increased pressure continuously on the arterial walls. For each increment of 20/10 mm Hg above a pressure of 115/75, the risk of CVD doubles (National Heart, Lung, and Blood Institute, 2003). Elevated levels of LDLs and decreased levels of HDLs predispose to the deposition of fatty deposits in the arterial walls, causing a narrowing of the vessels. Chemical toxins such as carbon monoxide (present in the blood) when a person smokes, and the toxins caused by renal failure, cause injury to the arterial walls. Substance abuse with alcohol, stimulants, and nicotine are damaging to the cardiovascular system (see Chapter 47).
Physiologic disorders such as diabetes mellitus and metabolic syndrome directly cause physical changes in the vessel walls, leading to more rapid arteriosclerosis, possibly from elevated blood glucose levels, an increased rate of atherosclerosis, and an earlier onset of hypertension. Some inherited disorders, such as hyperlipidemia, contribute to atherosclerosis.
Obesity, a sedentary lifestyle, and stress are all directly related to the increased incidence of atherosclerosis and hypertension. Smoking, and the changes it causes in the vessel walls, is directly related to arteriosclerosis of the peripheral vessels and decreased circulation in the lower extremities. Long-term hypertension causes arteriosclerosis and is a direct factor in the development of aortic aneurysm in many patients. Hypertension cannot be prevented, but it can be managed with diligent therapy and cooperation of the patient.
Prevention of Cardiovascular Disease
Cardiovascular diseases claimed 864,480 lives in 2005 in the United States (American Heart Association, 2009). Heart disease remains the major cause of death in the United States. Cardiovascular diseases also account for a large percentage of the chronic illnesses that disable, to some degree, a large portion of the U.S. population.
There are many kinds and degrees of heart disease. Advances in medical science have made it possible either to cure or successfully manage a large number of cardiovascular problems. Reasons for the decline in deaths from heart disease since the mid-1980s include improved emergency treatment of persons experiencing a coronary occlusion or “heart attack,” improved education of the public regarding ways to prevent heart disease, and teaching about the warning signs of a heart attack. Every nurse has a responsibility to assist with public education about heart disease.
Nonmodifiable risk factors are those that cannot be prevented by an individual. However, control of diseases such as hypertension and diabetes mellitus and the reduction of high cholesterol are possible. Since hypertension and diabetes are factors in the development of atherosclerosis, controlling them can help prevent the early onset of heart disease. If a person with diabetes can keep the hemoglobin A1c below 6% the risk of atherosclerosis is lessened (Matsushita, et al., 2010). Management of hypertension is one of the major tools for heart disease prevention.
Table 18-1 presents the risk factors for cardiovascular disease. Metabolic syndrome is particularly an indicator of cardiovascular risk and is diagnosed when three or more of the components in Box 18-1 are present (Gami et al., 2007). More than 50 million Americans have it. Modifiable risk factors are the major focus for education to prevent heart disease.
Table 18-1
Risk Factors for Cardiovascular Disease
| Unmodifiable Risk Factors | Significance |
| Heredity | Children of parents with cardiovascular disease are more likely to develop the same problem. |
| Race | African Americans experience high blood pressure two to three times more frequently than whites. Consequently the risk of heart disease in this group is higher. |
| Sex | Males experience more heart attacks than females earlier in life. After age 65, the death rate from heart disease increases in women. |
| Age | Four out of five people who die of a heart attack are age 65 or older. Increasing age increases risk. |
| Modifiable Risk Factors | Means of Modification |
| Obesity | Keep weight within normal limits by diet and exercise. |
| High cholesterol >200 mg/dL | Low-fat diet and exercise; medication. |
| Hypertension | Encourage blood pressure <120/80 mm Hg. |
| Diabetes | Good control by keeping blood sugar within normal limits (<110 mg/dL). |
| Cigarette smoking | Quit smoking. |
| Sedentary lifestyle | Exercise program of 30-min sessions three to five times a week. |
| Excessive stress | Use stress-reduction techniques regularly, such as exercise, relaxation techniques; reduce hostility; maintain a positive support system. |
| Excessive alcohol intake | Limit alcohol consumption to no more than recommended levels: men, 2 drinks/day; women, 1 drink/day. |
| Cocaine use | Do not use cocaine. |
The use of cocaine and methamphetamine has added to the problem of heart disease (American Heart Association, 2011). Cocaine causes vasoconstriction and is thought to speed up the atherosclerosis process. Also, cocaine has been known to cause sudden cardiac death, or stroke, in susceptible individuals. Research is finding that the ingestion of both alcohol and cocaine greatly increases the chance of cardiac death. Methamphetamine increases heart rate, causes vasoconstriction that can lead to hypertension, and speeds up electrical conduction, potentially causing dysrhythmias and myocardial infarction (MI). Cigarette smoking–related health problems are heavy contributors to heart disease, and smoking is a key factor in sudden cardiac death.
Nurses can play an important role in teaching others about hypertension and can support patient efforts to avoid the disease and its long-term consequences.
Although systolic blood pressure rises as a natural process of aging because arteries become less elastic, systolic hypertension should be treated in the elderly patient. Hypertension in the elderly is associated with an even higher risk of heart disease, stroke, and death from coronary thrombosis (Aronow et al., 2011). Hypertension has been associated with more rapid memory loss and loss of cognitive function in some research studies.
Contribute to reducing the incidence of the harmful effects of hypertension by participating in community screening programs and education. Nurses and other health care professionals have an obligation to serve as models for a healthy lifestyle.
Diagnostic Tests and Procedures
In addition to a routine physical examination and medical history, the physician has access to a number of procedures and tests to help diagnose cardiovascular disease (Figure 18-7). Noninvasive procedures usually are performed first

Specific cardiovascular diagnostic tests and their nursing implications are listed in Table 18-2. In women, an electron-beam computed tomography for coronary artery calcium scoring may be better than the standard treadmill test for detecting heart disease. A stress echocardiogram also is helpful.
Table 18-2
Common Diagnostic Tests for the Cardiovascular System
| Test | Purpose | Procedure | Nursing Implications |
| Chest radiograph | Shows size and shape of heart and mediastinal structures | Performed standing in a gown or in high Fowler’s position in bed. | No special requirements. |
| Electrocardiography (12-lead electrocardiogram [ECG]) | Records electrical impulses of the heart to determine rate, rhythm of heart, site of pacemaker, and presence of injury at rest | Small electrodes are placed on the chest and extremities, to show conduction patterns in different directions of electrical flow. Signal-averaged ECG can be used for patients at high risk for serious ventricular arrhythmias. | Inform patient that there is no discomfort with this test. Maintain electrical safety. Normal finding: normal ECG. |
| Holter monitor (ambulatory ECG) | Correlates normal daily activity with electrical function of the heart to determine whether activity causes abnormalities | Patient wears a small ECG recorder for 6, 12, or 24 hr while going about usual tasks. A diary is kept to show at what time the various activities were performed and any symptoms experienced. The tape is analyzed to correlate any dysrhythmia with the activity at that time. | Remind patient that all activities must be recorded in the diary: brushing teeth, climbing stairs, sexual intercourse, bowel movements, sleeping, etc. Caution patient not to remove the electrodes and not to get the recorder or wires wet. Have patient wear a loose shirt during test. |
| Exercise ECG stress test (treadmill) | Records electrical activity of the heart during exercise Insufficient blood flow and oxygen show up in abnormal waveforms | Small electrodes are placed on the chest, and a tracing is made while the patient exercises on a treadmill, bicycle, or stairs. The degree of difficulty of the exercise is increased as the test continues to see how the heart reacts to increasing work demands. Vital signs are continuously recorded. May be combined with radionuclide imaging or echocardiograph. Physician is present. | Requires a signed consent form. Have patient wear comfortable clothes and walking shoes. Light meal 2-3 hr prior, then NPO. Regular medications are given. Chest is shaved as needed for electrode placement. Inform patient that the test will be stopped if chest pain, severe fatigue, or dyspnea develops. |
| Chemical stress test with dipyridamole, adenosine, or dobutamine | Used for those who cannot exercise for an ECG stress test | An ECG is done and the drug is injected. Blood pressure and pulse are taken and recorded q 15 min while the drug takes effect by diverting blood flow from the coronary arteries, causing cardiac ischemia. Thallium or technetium-99m (99mTc) may be injected during exercise at maximum heart rate. Scanning images are taken with a gamma camera over a period of 40 min. A repeat scan may be done in 3-4 hr. The patient is NPO during the test. | Mild nausea or headache may occur. Explain that patient will lie on back for the imaging. If BP drops too low, phenylephrine is given. |
| Nuclear imaging (thallium perfusion imaging) | Evaluates blood flow in various parts of the heart; determines areas of infarction | Thallium-201 is injected IV, radioactive uptake is counted over the heart by a gamma scintillation camera. May be done in conjunction with an exercise ECG stress test. | Explain that the radioactivity used is a very small amount and lasts only a few hours. Explain that a camera will be positioned over the heart. ECG electrodes are placed on the chest; scanning is done 10-15 min after injection; can be done as an outpatient procedure. May be done in two parts a few hours apart. |
| Technetium pyrophosphate scan and multiple-gated acquisition (MUGA) scan | Determines area and extent of myocardial infarction Assesses left ventricular function | 99mTc is injected IV and is taken up by areas of infarction, producing hot spots when scanned. Multiple serial images are obtained. Best results occur when done 1-6 days after a suspected MI. | Inform patient that radioisotopes will be given IV and that it will be necessary to lie still while the machine scans the heart. The patient’s glucose must be between 60-140 mg/dL. If scan is combined with exercise, patient will need to be NPO and must refrain from tobacco and caffeine for 24 hr before the test. |
| Ventilation-perfusion scan (V-Q scan) | Detects blood clots, particularly pulmonary emboli | A radioisotope is injected, and after a waiting period for uptake, a scintillation scanning camera is used to measure the amount of radioactivity present in the area in question. | Determine whether patient has an allergy to the dye. After the test encourage large fluid intake to flush the dye through the kidneys. |
| Positron emission tomography | Evaluates myocardial perfusion | IV nitrogen-13-ammonia is injected and a scan performed to show myocardial metabolic function. Then fluoro-18-deoxyglucose is injected and a scan performed. In a normal heart, the scans will match; in an ischemic heart, the scans will differ. | Inform patient that radioisotopes will be given IV and that it will be necessary to lie still while the machine scans the heart. The patient’s glucose must be between 60-140 mg/dL. If scan is combined with exercise, patient will need to be NPO and must refrain from tobacco and caffeine for 24 hr before the test. |
| Echocardiography | Useful in evaluating size, shape, and position of structures and movement within the heart Test of choice for valve problems | A metal wand that emits sonar waves is guided over the chest wall while the patient is supine or turned on the left side. Takes 30-60 min. May be done in combination with the exercise (stress) test. | Inform patient that there is no discomfort, although conduction jelly may feel cool. Normal finding: no abnormalities of size or location of heart structures; normal wall movement. |
| Stress echocardiogram | Detects differences in left ventricular wall motion before and after exercise | Resting echocardiogram images are obtained. The patient exercises, and then within 1 min, postexercise images are obtained. | Explain the procedure and the importance of returning to the examining table immediately after exercising. No heavy meal beforehand, no smoking or caffeine for 6-8 hr before test. Tell patient to wear walking shoes. |
| Dobutamine echocardiogram | A substitute for an exercise stress test when individual cannot exercise Detects abnormal heart wall motion | IV dobutamine, a positive inotropic agent, is infused. The dosage is increased at 5-min intervals during the echocardiogram. | Administer IV dobutamine as ordered. Monitor vital signs; watch for symptoms of distress. |
| Transesophageal echocardiogram (TEE) | Provides images of the heart, mitral valve, atrial septum, and thoracic aorta | Pharynx is anesthetized with topical agent. With patient in left side-lying position, an endoscope and a transducer are placed in the esophagus behind the heart. Recordings of the images are made. Test takes about 20 min. | NPO for 4-6 hr before test. Initiate IV access before test for sedation. Apply ECG leads for monitoring during test. Monitor pulse oximetry and BP. Observe after test until sedation has worn off. |
| Angiogram (venogram) | Identifies thrombi within the venous system | A tourniquet may be placed on the extremity and dye is injected into the affected extremity. Radiographs are taken at timed intervals. Also used to identify venous stenosis. | Requires a signed consent form. Assess for allergies to radiopaque dye. Hydrate the patient prior to the procedure. Tell patient it takes 30-90 min and that a warm flush may be felt when the dye is injected. |
| Arteriogram | Visualizes arterial anatomy and vascular disease in carotid, vertebral, aorta, renal, coronary, and peripheral arteries | A catheter is placed via the femoral artery into the desired artery. Radiopaque contrast is injected while x-ray images are obtained. Digital subtraction techniques obliterate bony structures from the views. CO2 gas may be used in place of dye if the patient is allergic to the dye. A balloon may be used during the procedure to open constricted areas. A stent may be placed in the vessel to keep it open. Magnetic resonance angiography may also be used to visualize vessels. | Requires a signed consent form. NPO for 2-8 hr before test. Mark peripheral pulses before procedure. Check renal function studies before test and alert physician of abnormal values. Mucomyst may be administered a day before and after the test to prevent dye induced nephropathy. Warn that dye may cause some bladder distention during the test. |
| Cardiac catheterization with coronary angiography | Assesses pumping action of both sides of the heart Measures pressure within the heart chambers Measures cardiac output Calculates differences in oxygen content of arterial and venous blood Assesses size and patency of coronary arteries and presence of collateral circulation | Catheter is inserted into vein or artery, depending on which side of the heart is to be tested. Femoral artery or brachial vein is often used. With local anesthetic and sedation, the catheter is threaded up into the heart, and pressure readings and oxygen saturation determinations are taken. Contrast media may be injected to visualize the size and shape of the chambers and structures. Takes 1½-3 hr. Fluoroscopy is used during the procedure. Angiography performed by dye injection during cardiac catheterizations. Computed tomographic angiography used to enhance images. Video recording made during procedure for later review. | Requires a signed consent form. Patient is NPO for 6-8 hr before test. Assess for allergy to iodine, shellfish, or contrast dye. Have patient void before giving preoperative medication. Record baseline vital signs and mark location of pedal pulses. Inform patient that procedure involves being strapped to a table that tilts, will have an IV, and patient must lie still during test. ECG leads will be in place during the test. If dye is used, patient will feel a hot flush for a minute after the dye is injected. Patient may be asked to cough during the procedure. Patient will be constantly monitored and emergency equipment is at hand. Post-test: vital signs q 15 min × 4, q 30 min × 4, then q 1 hr × 4, or until stable. Assess peripheral pulses with vital signs and question patient about numbness or tingling. Inspect insertion site for bleeding or sign of hematoma. Pressure dressing or clamp, or sandbag weight are left in place for 1-3 hr. If femoral insertion site was used, keep patient flat and leg extended for 6 hr. If brachial site was used, immobilize arm for 3 hr. If dye was used, encourage fluids unless contraindicated. Mark location of distal pulses before the procedure. Postprocedure, prevent hip flexion on affected side. |
| Ultrasound Coronary | Determines patency of coronary arteries and presence of collateral circulation | Performed during cardiac catheterization. A flexible catheter with a miniature transducer at the tip is introduced into a peripheral vessel and advanced into a coronary artery. The transducer emits high-frequency sound waves, which create a two- or three-dimensional image of the vessel lumen. | Consent form required. See cardiac catheterization for post-test care. |
| Lower extremity | Assesses occlusion or thrombosis in an artery or vein | Skin is bared and a water-soluble gel is applied to the area to be assessed. A Doppler transducer is passed over the area of the vessel. A gray-scale image of the vessel is obtained. A computer provides a two-dimensional image of the vessel along with an image of blood flow. | Instruct to abstain from smoking for 30 min before the test. |
| Carotid duplex examination | Studies blood flow in external carotid arteries | Patient is positioned supine with neck extended. The probe is moved up and down each side of the neck over the external carotid arteries. | Explain that plaque in the arteries can be visualized in this manner. This test assists in determining need for endarterectomy surgery. |
| Computed tomography (CT) scan | Determines size and condition of aortic aneurysm | Noninvasive, unless dye contrast used. Patient is positioned on scanning table and moved under the scanner. | Instruct patient in necessity of holding still during scan. |
| Magnetic resonance imaging (MRI) Magnetic resonance angiography (MRA) | Evaluates cardiac tissue integrity, detects aneurysms, determines ejection fraction and cardiac output, and determines patency of proximal coronary arteries | Noninvasive magnetic resonance is used to depict tissue images. IV gadolinium is injected as a contrast medium for the MRA. | Explain about the cylinder within which the patient will be positioned. Warn that there will be loud noises from the machine. Administer antianxiety medication if needed and ordered; provide music if patient desires it. |
| Electrophysiology studies | Measures and records electrical activity from within the heart to determine the area of origin of the dysrhythmia and the effectiveness of the antidysrhythmic drug for the particular dysrhythmia | Three to six electrodes are placed in the heart through the venous system. They are attached to an oscilloscope that records the intracardiac and ECG waveforms simultaneously. After baseline tracings are taken, the cardiologist tries to trigger the dysrhythmia that is to be studied by programmed electrical stimulation through the electrodes. Once the dysrhythmia is triggered, an antidysrhythmic drug is administered to determine its effectiveness in stopping the abnormal rhythm. Studies may take from 1½-4 hr; serial studies may be done on different days. | Provide psychological support for the patient, who is often scared of having dysrhythmias induced. Antidysrhythmic drugs may be stopped 24 hr or more before the test to eliminate them from the patient’s system. Assure the patient of constant monitoring and that emergency equipment and staff will be on hand. Keep patient NPO after midnight. Patent IV line is maintained. Electrodes are placed using fluoroscopy. Patient will be supine on an x-ray table. Chest surface electrodes will be placed before the electrodes are threaded into the heart. The femoral vein is most commonly used; the groin is shaved, and local anesthesia is used. Post-test care: much the same as for cardiac catheterization. |
| Impedance plethysmography | Estimates blood flow in a limb based on electrical resistance present before and after inflating a pneumatic cuff placed around the limb Detects deep vein thrombosis | Measurements of electrical resistance are taken before and after a pneumatic cuff placed around the limb is inflated. Electrodes are placed on opposite sides of the limb. | Instruct to wear loose clothing. Explain that some discomfort may occur during inflation of the cuff. The patient is placed on an examination table and positioned supine in a relaxed, comfortable position. The limb is properly positioned, and electrodes and the pneumatic cuff are applied. |
| Hemodynamic monitoring via Swan-Ganz catheter | Determines pressure, flow, and oxygenation within the cardiovascular system Normal values: Preload: RAP 2-8 mm Hg PAWP 6-12 mm Hg PADP 4-12 mm Hg Afterload: MAP 70-105 mm Hg Oxygenation: Arterial Hgb Sao2 95%-99% Mixed venous Hgb Sao2 69%-80% | A special catheter, infusion system, transducer, and a monitor are prepared and the catheter is placed in the heart or great vessels by the physician. | The system must be calibrated to perform properly. Readings are taken for right atrial, pulmonary artery, and pulmonary wedge pressures. Other data can then be calculated regarding stroke volume, cardiac output, and oxygenation. Triglycerides contribute to arterial disease. As triglycerides rise, so do low-density lipoproteins, which are a factor in atherosclerosis. The lipoproteins (LDL, VLDL, and HDL) are increased in hyperlipidemia. Lipoprotein fractions are determined by electrophoresis and are used to assign a “risk” factor in cardiovascular disease. High levels for HDL appear to protect against coronary artery disease and MI, whereas increased levels of LDL are associated with increased atherosclerosis and MI. |
| Laboratory Tests* | |||
| B-type natriuretic peptide (BNP) | Determines degree of HF. | Obtain 5-7 mL of venous blood in an EDTA lavender-top tube. | No fasting is required. |
| C-reactive protein (CRP) | Assesses cardiac risk; increased with inflammation Low risk <1 mg/dL High >3 mg/dL | Obtain one red-top tube of venous blood. | Some laboratories require fasting; water is permitted. |
| Serum lipids | Determines level: Normal values: Cholesterol: 150-200 mg/dL HDL: 32-75 mg/dL LDL: 73-200 mg/dL (with two or more risk factors, <73 mg/dL) Triglycerides: 50-250 mg/dL | Elevation of cholesterol is a risk factor for atherosclerotic heart disease. | Patient is NPO except for noncaloric liquids for 12 hr. |
| Vertical auto profile (cholesterol) | Provides more comprehensive cardiac risk assessment | Requires a blood draw and can be done along with total lipid profile. | Should fast for 12 hr |
| Myoglobin | Detects damage to the myocardium from a myocardial infarction. Normal range: <90 mcg/L | Requires a blood draw of 5 mL in a red-top tube. Apply pressure to venipuncture site. | Explain procedure. No fasting is required. |
| Troponin I (Tn I) Troponin T (Tn T) | <0.3 mcg/L <0.1 mcg/L | Specific to heart muscle damage. Levels may elevate within 4-6 hr after MI, peak within 10-24 hr, and return to normal within 10 days. | |
| Creatine phosphokinase (CPK) | Men: 55-170 IU/L Women: 30-135 IU/L | Elevated within 4-8 hr following heart attack (may also rise with injury to other muscles). Peaks within 12-24 hr, returns to normal levels within 3-4 days. | |
| Homocysteine | Men: 5.2-12.9 μmol/L Women: 3.7-10.4 μmol/L | Elevation is considered an independent risk factor for ischemic heart disease. | Blood sample in blue- or purple-top tube; 10- to 12- hr fast required. |
| CK-MB (creatine kinase) | <3 ng/mL | Elevates within 2-6 hr after an MI, peaks within 12-24 hr, and returns to normal within 3 days. CK-MB is specific to myocardial injury. | |
| Myeloperoxidase antigen (MPO) | <6 U/mL | Detects or assists in ruling out microangitis of the arteries. | Requires 0.5 mL blood in a yellow-top tube. No fasting required. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree