Agonal rhythm, 427.89
Asystole, 427.5
Atrial fibrillation, 427.31
Atrial flutter, 427.32
Cardiac rhythms/arrhythmias, 427.9
First-degree AV block, 426.11
Idioventricular rhythm, 426.89
Junctional/nodal, 427.89
Premature atrial contractions, 427.61
Premature ventricular contractions, 427.69
Pulseless electrical activity, 427.89
Second-degree block (Mobitz type I) (Wenckebach), 426.13
Second degree block (Mobitz type II), 426.12
Sinus arrhythmia, 427.9
Sinus bradycardia, 427.89
Sinus tachycardia, 427.89
Supraventricular tachycardia, 427.89
Third-degree AV block (complete heart block), 426.0
Ventricular fibrillation, 427.41
Ventricular tachycardia, 427.1
Note: Emergency cardiovascular care is an evolving science. Practitioners are strongly encouraged to regularly attend advanced cardiovascular life support (ACLS) update courses because national guidelines are periodically revised.
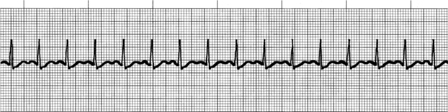
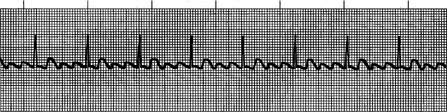
I. Normal sinus rhythm (NSR)
(Figure 18-1)
A. Characteristics.
1. Regular rate and rhythm
2. PR interval and QRS complex normal.
a. PR interval 0.20 seconds or less
b. QRS complex 0.12 seconds or less
B. Rate is 60 to 100 beats/minute (bpm).
 |
| FIGURE 18-1Normal sinus rhythm.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
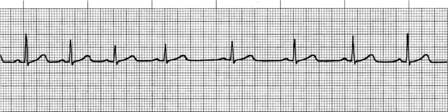
(Figure 18-2)
A. Characteristics.
1. Regular rate and rhythm
2. PR interval and QRS complex normal
B. Rate 60 bpm or less than expected relative to underlying condition or cause
C. Etiology.
1. Increased vagus nerve activity (e.g., in athletes, during Valsalva maneuver)
2. Digitalis (Digoxin)
3. Propranolol (Inderal)
4. Quinidine
5. Hypoxemia
D. Clinical manifestations.
1. Decreased cardiac output
2. Hypotension
3. Loss of consciousness
4. Other signs of poor perfusion
E. Treatment.
1. Primary ABCD survey: Assess ABCs, secure airway noninvasively, and ensure that monitor/defibrillator is available.
3. For serious signs or symptoms related to bradycardia, continue as follows:
a. Atropine, 0.5 mg IV; repeated every 3 to 5 minutes as needed, not to exceed a total dose of 3 mg
b. Transcutaneous pacing—especially indicated with symptomatic type II second-degree atrioventricular (AV) block or third-degree AV block until transvenous pacemaker can be inserted
c. Consider dopamine (Intropin), 2-10 mcg/kg/minute
d. Consider IV epinephrine drip at 2-10 mcg/minute (1 mg of 1:1000 solution mixed in 500 mL normal saline; administered at 1-5 mL/minute).
 |
| FIGURE 18-2Sinus bradycardia.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
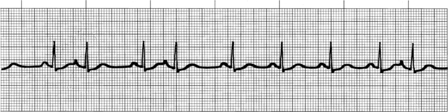
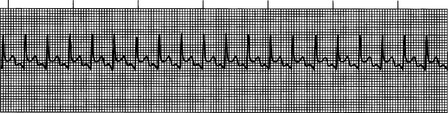
III. Sinus tachycardia (ST)
(Figure 18-3)
A. Characteristics.
1. Regular rate and rhythm
2. PR interval and QRS complex normal
B. Rate 100 bpm or more and typically less than 150 to 160 bpm
C. Etiology.
1. Pain
2. Fever
3. Anxiety
4. Shock
5. Hypovolemia
6. Congestive heart failure
7. Cocaine use
E. Treatment.
1. Treat the underlying problem or cause.
2. Medications are not indicated.
 |
| FIGURE 18-3Sinus tachycardia.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
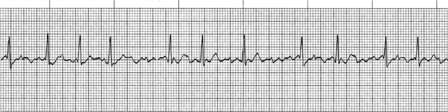
IV. Sinus arrhythmia
(Figure 18-4)
A. Characteristics.
1. Rate is variable (i.e., variable R-R interval).
2. Normal PR interval and QRS complex
3. Rate varies with respirations.
B. Etiology: common in children and the elderly
C. Clinical manifestations: none known
D. Treatment: none known
 |
| FIGURE 18-4Sinus arrhythmia.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
V. Premature atrial contractions (PACs)
(Figure 18-5)
A. Characteristics.
1. Occur when an ectopic focus in the atria fires before the next sinus node impulse. P waves usually look different (i.e., either smaller or peaked).
B. Etiology: unknown
C. Clinical manifestations: none
D. Treatment: none
 |
| FIGURE 18-5Premature atrial contractions.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
VI. Atrial fibrillation (A-Fib)
(Figure 18-6; also see Figure 18-26 at the end of this chapter)
A. Characteristics.
1. No discernible P waves; fibrillatory waves are noted instead.
2. PR interval is not measurable (wavy baseline).
3. QRS complex is regularly irregular.
4. Atrial rate is commonly 300 to 400 bpm or greater.
5. Ventricular rate is usually 100 to 160 bpm or greater.
B. Etiology.
1. Congestive heart failure
2. Hypoxemia
3. Valvular disease
4. Hyperthyroidism
C. Clinical manifestations.
1. Patient may be asymptomatic.
2. Patient may report palpitations.
3. Decreased cardiac output leads to hypotension and loss of consciousness.
D. Treatment.
1. Management of atrial fibrillation and/or atrial flutter is based on these parameters:
a. Normal heart function
b. Whether CHF exists
c. Whether Wolff-Parkinson-White (WPW) syndrome is present
d. Whether the goal is to control the rate or convert the rhythm, considering the duration of onset (i.e., less than or longer than 48 hours)
f. Management of narrow, complex, irregular tachycardia rate control can be accomplished with diltiazem, beta blockers, or magnesium for rapid ventricular response.
g. If WPW is suspected, AV nodal blocking drugs can cause a paradoxical increase to the fast atrial fibrillation impulse; therefore, these drugs should not be used.
2. To control rate in patients with atrial fibrillation/flutter and to ensure normal heart function, the following recommendations apply:
a. If atrial fibrillation/flutter has persisted longer than 48 hours, converting agents should be used with extreme caution in patients not receiving adequate anticoagulation because of the possibility of embolic events.
b. Consider the following choices:
i. Calcium channel blockers
(a) Diltiazem (Cardizem), 15-20 mg (0.25 mg/kg) IV over 2 minutes
(b) May repeat in 15 minutes at 20-25 mg (0.35 mg/kg) over 2 minutes
(c) Maintenance infusion rate is 5-15 mg/hour titrated to heart rate (may also use verapamil).
ii. Beta blockers
(a) Atenolol (Tenormin), 5 mg IV, slowly over 5 minutes
(b) Wait 10 minutes, then administer a second dose of 5 mg IV, slowly over 5 minutes.
(c) In 10 additional minutes, if tolerated well, may begin 50 mg PO
(d) Then, give 50 mg PO twice daily (esmolol or metoprolol may also be used).
3. To convert the rhythm in a patient with atrial fibrillation/flutter and duration of less than 48 hours:
a. Use the following agents for patients with normal (preserved) heart function:
i. Amiodarone (Cordarone)
(a) Maximum cumulative dose, 2.2 g/24 hours IV
(b) May cause profound vasodilatation and hypotension
(c) Rapid infusion: 150 mg IV over the first 10 minutes (15 mg/minute); may repeat rapid infusion (150 mg IV) every 10 minutes as needed
(d) Slow infusion: 360 mg IV over 6 hours (i.e., 1 mg/minute)
(e) Maintenance infusion: 540 mg IV over 18 hours (i.e., 0.5 mg/minute)
ii. Ibutilide (Corvert)
(a) For adults weighing 60 kg or more, administer 1 mg (10 mL) over 10 minutes; a second dose may be administered at the same rate 10 minutes later.
(b) For adults weighing less than 60 kg, administer 0.01 mg/kg initially IV.
b. For patients with impaired heart function, use Class IIb agents.
i. Amiodarone (Cordarone)
(a) Maximum cumulative dose, 2.2 g/24 hours IV; may cause profound vasodilatation and hypotension
(b) Rapid infusion: 150 mg IV over the first 10 minutes (15 mg/minute); may repeat rapid infusion (150 mg IV) every 10 minutes as needed.
(c) Slow infusion: 360 mg IV over 6 hours (i.e., 1 mg/minute)
(d) Maintenance infusion: 540 mg IV over 18 hours (i.e., 0.5 mg/minute)
4. To convert the rhythm in a patient with atrial fibrillation/flutter in whom duration has been longer than 48 hours or unknown:
a. NO direct current (DC) cardioversion
i. Note: When pharmacologic agents or shock is used, embolic events may occur during the conversion of atrial fibrillation/flutter to normal sinus rhythm from atrial thrombi, unless the patient has been adequately anticoagulated.
ii. Use pharmacologic agents with extreme caution if duration has been longer than 48 hours, or
b. Delayed cardioversion
i. Anticoagulation × 3 weeks, cardiovert the patient and then continue anticoagulation for an additional 4 weeks, or
c. Early cardioversion
i. Begin heparin IV immediately (e.g., heparin 80 units/kg IV bolus followed by 18 units/kg/hour IV continuous infusion).
ii. Conduct a transesophageal echocardiogram (TEE) to rule out atrial thrombi.
iii. Cardiovert within 24 hours after TEE.
iv. Continue anticoagulation therapy for an additional 4 weeks
5. To control rate in patients with atrial fibrillation/flutter and impaired heart function (i.e., CHF or ejection fraction less than 40%), the following recommendations apply:
a. If atrial fibrillation/flutter has persisted for longer than 48 hours, pharmacologic converting agents should be used with extreme caution in patients not receiving adequate anticoagulation because of the possibility of embolic events.
b. Consider only one of the following Class IIb choices:
i. Digoxin
(a) Loading dose of 10-15 mcg/kg of lean body weight
ii. Diltiazem
(a) 15-20 mg (0.25 mg/kg) IV over 2 minutes
(b) May repeat in 15 minutes at 20-25 mg (0.35 mg/kg) over 2 minutes
(c) Maintenance infusion rate is 5-15 mg/hour titrated to heart rate.
iii. Amiodarone
(a) Maximum cumulative dose, 2.2 g/24 hours IV
(b) May cause profound vasodilatation and hypotension
(c) Rapid infusion: 150 mg IV over the first 10 minutes (15 mg/minutes); may repeat rapid infusion (150 mg IV) every 10 minutes as needed
(d) Slow infusion: 360 mg IV over 6 hours (i.e., 1 mg/minute)
(e) Maintenance infusion: 540 mg IV over 18 hours (i.e., 0.5 mg/minute)
6. To convert the rhythm in a patient with atrial fibrillation/flutter, impaired heart function (i.e., CHF or EF less than 40%), and duration less than 48 hours:
a. Consider DC cardioversion, Class I (preferred intervention)
b. Amiodarone, Class IIb
i. Maximum cumulative dose, 2.2 g/24 hours IV
ii. May cause profound vasodilatation and hypotension
iii. Rapid infusion: 150 mg IV over the first 10 minutes (15 mg/minute); may repeat rapid infusion (150 mg IV) every 10 minutes as needed
iv. Slow infusion: 360 mg IV over 6 hours (i.e., 1 mg/minute)
v. Maintenance infusion: 540 mg IV over 18 hours (i.e., 0.5 mg/minute).
7. To convert the rhythm in a patient with atrial fibrillation/flutter, impaired heart function (CHF or EF less than 40%), and duration greater than 48 hours or unknown:
a. Anticoagulation therapy as previously discussed.
b. DC cardioversion.
8. To control rate and convert rhythm in a patient with atrial fibrillation/flutter of 48 hours’ duration or less who has Wolff-Parkinson-White syndrome, the following agents are recommended:
a. Amiodarone
b. Ibutilide
c. Flecainide
d. Propafenone
e. Digoxin
f. Clonidine
g. Magnesium
h. Impaired heart function, Class IIb drug
i. Amiodarone and no other drugs.
9. To control rate and convert rhythm in a patient with atrial fibrillation/flutter of longer than 48 hours’ duration who has Wolff-Parkinson-White syndrome, the following recommendations apply:
a. Early cardioversion (less than 24 hours)
i. Administration of heparin immediately and TEE to rule out atrial clot, followed by cardioversion within 24 hours
ii. Continue anticoagulation for 4 weeks or longer.
b. Delayed cardioversion (longer than 3 weeks)
i. Use anticoagulation for 3 or more weeks (until an international normalized ratio [INR] of 2 to 3), followed by cardioversion.
ii. Continue anticoagulation for an additional 4 weeks or longer.
 |
| FIGURE 18-6Atrial fibrillation.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
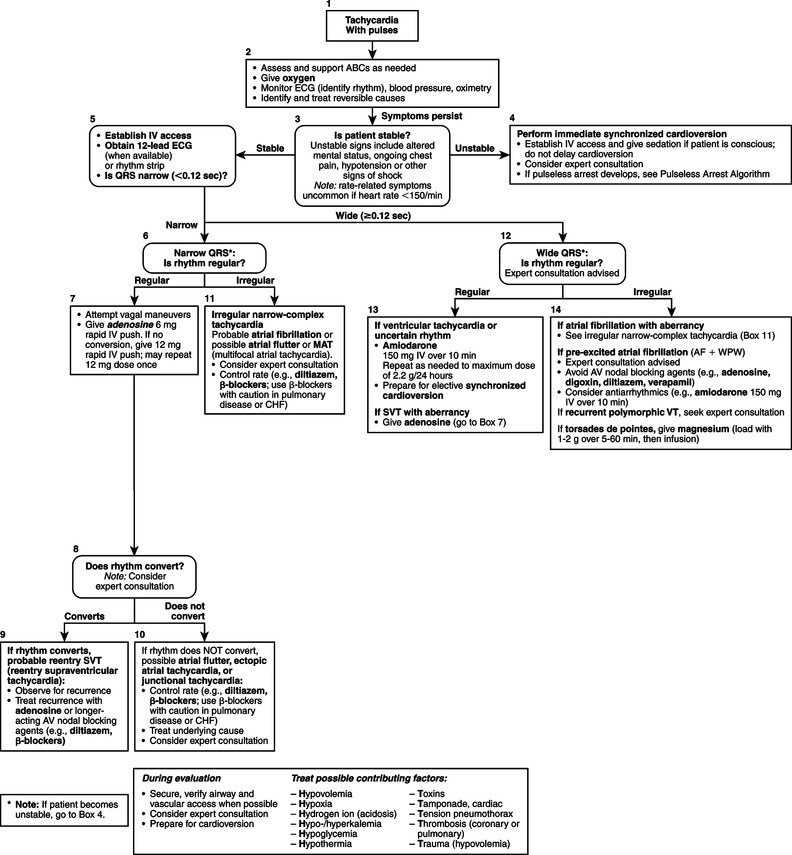 |
| FIGURE 18-26ACLS Tachycardia Algorithm.(Redrawn from Field JM, editor: Advanced carsiovascular life support, Dallas, Tex, 2006, American Heart Association.)American Heart Association |
VII. Atrial flutter (A-flutter)
(Figure 18-7; also see Figure 18-26)
A. Characteristics.
1. Sawtooth appearance of flutter waves (F waves), especially if the rhythm strip is turned upside down
2. PR interval is not measurable.
3. Atrial rate ranges from 240 to 360 bpm.
4. QRS complex is usually normal.
B. Etiology.
1. Congestive heart failure
2. Hypoxemia
3. Valvular disease
4. Hyperthyroidism
C. Clinical manifestations.
1. Decreased cardiac output
2. Hypotension
3. Loss of consciousness
D. Treatment: same as for atrial fibrillation
 |
| FIGURE 18-7Atrial flutter.(From Cohn EG, Gilroy-Doohan M: Flip and see ECG, ed 2, Philadelphia, 2002, WB Saunders, with permission.) |
 Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|