This chapter covers three types of gastrointestinal obstructive problems: biliary obstruction, gastric obstruction, and bowel obstruction. Obstructive disorders of the biliary and gastrointestinal tract are common complications in patients with advanced gastrointestinal, abdominal, pelvic, and hepatobiliary malignancies. Patients with an obstructive process are acutely ill and require intensive nursing care directed at symptom control.
BILIARY OBSTRUCTION
Obstruction of the biliary tract occurs when the hepatic or extrahepatic biliary ducts are occluded, causing a decrease in or obstructed flow of bile. Obstruction of the biliary tree may be caused by malignant or nonmalignant conditions.
Bile, which is produced by the hepatocytes, contains bile salts, water, cholesterol, electrolytes, and bilirubin. Bilirubin is the end product of heme degradation. The main function of bile is to emulsify fats. Half of the bile produced moves from the liver into the duodenum though a system of ducts, which ultimately drains into the common bile duct (CBD). The CBD passes through the head of the pancreas for about 2 centimeters before passing through the ampulla of Vater into the duodenum. In the liver, the bile is collected into the small bile canaliculi, which are small ducts surrounding the hepatocytes. The canaliculi empty into progressively larger ducts into the hepatic and common bile duct. Bile then is delivered to the gallbladder for concentration and storage or directly into the intestine (Corwin, 2000). About 50% of bile is stored in the gallbladder; after a person eats, it is released into the cystic duct, which joins the hepatic ducts from the liver to form the common bile duct.
Any occlusion of bile flow through the bile ducts may lead to obstructive jaundice. Biliary obstruction may arise from intrinsic occlusion or extrinsic compression. Jaundice is an excess of bilirubin in the blood; it is referred to as icterus when it is visible in the sclera or the skin. Obstruction of the bile canaliculi caused by a hepatic tumor, inflammation, or calculi causes intrahepatic jaundice. Because obstruction at this level reduces the flow of conjugated bilirubin into the bile duct, the amount of conjugated bilirubin absorbed into the blood increases. Posthepatic obstructive jaundice occurs when the bile flow is blocked at the level of the extrahepatic bile ducts by a tumor, porta hepatis lymphadenopathy, or gallstones. The liver is able to conjugate bilirubin, but the bilirubin is unable to reach the small intestine; therefore it enters the bloodstream, where most of it is excreted by the kidneys into the urine. If the obstruction persists, the bile canaliculi become congested and rupture, spilling bile into the lymph and bloodstream. Bilirubin binds to elastic tissue, causing the characteristic color changes of yellow skin and sclera.
EPIDEMIOLOGY AND ETIOLOGY
In the United States the incidence of biliary obstruction is approximately 5 per 1000 people. Biliary obstruction in patients with cancer may arise from mechanical causes, such as a primary or metastatic tumor, and it may be either intrahepatic or extrahepatic. Nonmalignant causes of biliary obstruction include gallstones, hepatic artery thrombosis, sclerosing cholangitis, iatrogenic conditions, pancreatitis, and biliary stricture secondary to previous surgery or hepatic intraarterial chemotherapy. Gallstones, the most common cause of biliary obstruction, have a higher incidence in females, individuals of Hispanic and Northern European origin, and prima women (Bonheur et al., 2006). Infectious causes of obstruction include HIV and oriental and parasitic cholangitis. Other, less common causes are Caroli’s disease, Mirizzi’s syndrome, and retroperitoneal fibrosis.
RISK PROFILE
• Patients with advanced malignancy in or near the biliary ducts are at risk for developing obstruction from tumor invasion.
• Malignant causes include cancer of the pancreas, ampullary carcinoma, and cholangiocarcinoma (Kichian & Bain, 2004). Metastatic lymphoma and melanoma have also been identified as causes of extrahepatic biliary obstruction (Stellato, 1987).
• Hepatic intraarterial chemotherapy with 5-fluoropyrimidines may cause obstructive jaundice by causing bile duct strictures (Shea et al., 1986).
• Enlarged lymph nodes at the porta hepatis may present a risk of obstruction.
• Nonmalignant causes include gallstones, chronic pancreatitis, and biliary stricture.
PROGNOSIS
Patients with biliary obstruction arising from pancreatic cancer, cholangiocarcinoma, and metastatic disease are at risk of developing ascending cholangitis. Surgical bypass or stenting, if done early in the disease process, may prolong life and improve symptoms. Unfortunately, these procedures may not always be possible in advanced disease, in which case life expectancy is limited. The mortality and morbidity of biliary obstruction depend on the cause of the obstruction. The duration of palliation by stenting depends on the disease and the type of stent used. (Earnshaw et al., 1992). Patients with biliary obstruction are gravely ill because of the obstruction and infection; however, treatment with antibiotics and GI procedures may dramatically improve their physical condition and symptoms.
PROFESSIONAL ASSESSMENT CRITERIA (PAC)
1. A complete history and physical examination are important in the evaluation and treatment of biliary obstruction. The following information should be obtained:
• Cancer history and treatment, including surgery, hepatic artery chemotherapy, and radiation
• Surgical history
• Medical history of gallstones, biliary colic, liver disease, pancreatitis, and risk factors for or a history of hepatitis
• Current medications and past use of hepatotoxic agents, drug use, and alcohol
• Review of systems, with attention to symptoms of pain in the right upper quadrant, anorexia, dyspepsia, nausea, weight loss, low-grade fever, fatigue, diarrhea, and symptoms of jaundice. The most obvious signs and symptoms of biliary obstruction, which are caused by jaundice, include pruritus, darkening or yellow skin, dark/frothy urine, pale or clay-colored stools, and bruising.
2. The physical exam may reveal weight loss or a low-grade temperature. The skin should be examined for jaundice, which in fair-skinned patients is most noticeable on the face, trunk, and sclerae, and in dark-skinned patients on the sclerae, conjunctivae, and hard palate. Examining the skin in natural sunlight is superior to examination in indoor light because jaundice may not be detectable in artificial lighting. Scratch marks and bruising are other noteworthy findings. In cirrhosis, purpuric spots, vascular angiomas, and palmar erythema may be present. Ecchymoses may be seen in obstructive or hepatocellular disease. The physical findings on the abdominal exam will vary, depending on the etiology of the obstruction. Dilated periumbilical veins indicate portal collateral circulation and cirrhosis. Ascites may be present in metastatic disease or cirrhosis. A right upper quadrant mass, hepatomegaly with a bruit, or splenomegaly may be present. The gallbladder may be palpable with obstruction of the common bile duct. The practitioner should also palpate for lymphadenopathy.
3. Laboratory diagnostics: The purpose of obtaining laboratory data is to distinguish between obstructive and nonobstructive (intrahepatic cholestasis) jaundice. A complete blood count (CBC) is done to check for anemia and hemolysis. A positive direct Coombs’ test is seen in hemolytic anemia. The total and direct bilirubin levels are elevated with obstruction. An increased indirect (free or unconjugated) bilirubin is seen in nonobstructive jaundice, such as autoimmune hemolysis, cirrhosis, and viral and drug-induced hepatitis. Liver function tests are useful, but it is important to realize that results will vary, depending on the extent of the obstruction or disease. Increased aspartate transaminase (AST) or alanine transaminase (ALT) with an increased bilirubin level indicates hepatocellular disease or injury. A normal or mildly elevated AST with an elevated bilirubin is seen in intrahepatic cholestasis and biliary obstruction. Elevated alkaline phosphatase and ALT levels three times the normal indicate obstruction or prolonged cholestasis. A decreased albumin may be seen in hepatocellular disease. The urine often is positive for bilirubin. The prothrombin time may be prolonged with cholestasis, obstruction, or hepatocellular injury. Lipase and amylase are elevated with pancreatitis. Hepatitis titers should be ordered if viral hepatitis is suspected.
4. Imaging studies: Radiographic studies frequently are performed to determine the etiology of the obstruction. Evaluation of the liver by ultrasound is done to differentiate between obstructive and nonobstructive jaundice, and it may also detect cirrhosis, hepatic abscess, cysts, hematoma, and tumors. This noninvasive procedure is helpful for viewing the intrahepatic duct structure and areas of the gallbladder (Bonheur et al., 2006). However, visualization may be poor as a result of obesity or overlying bowel gas. CT scanning with intravenous contrast may be necessary if the ultrasound exam is inconclusive. CT scans allow assessment of the liver’s size and structure, as well as abnormalities, but they are more expensive. Scintiscans, which are rarely used in clinical practice, have been used to distinguish between hepatocellular dysfunction and extrahepatic obstruction. However, they are not used as initial imaging; rather, they tend to be reserved for demonstrating a bile leak or evaluating stent placement (Drane, 1991). Percutaneous transhepatic cholangiography, which is used only when a percutaneous drain is placed, may help in the study of the anatomic details. Although rare, side effects of bleeding, biliary leakage, and sepsis can occur after this procedure. Endoscopic retrograde cholangiopancreatography (ERCP) is useful for patients who have pancreatic disease, because a view of the pancreatic ducts can also be obtained (Bonheur et al., 2006). Magnetic resonance cholangiopancreatography, when available, may be useful and reduces the need for invasive cholangiography (Lillemoe, 1999).
NURSING CARE AND TREATMENT
1. Palliation may be approached by biliary surgical bypass, stenting, and external drainage, and palliative approaches occasionally may be combined with chemotherapy and radiation. Malignant biliary obstruction may be treated by several different procedures, depending on the location and degree of obstruction and the patient’s medical status and prognosis. Nursing care varies according to the type of procedure used, therefore nurses who care for these patients should be familiar with the following procedures:
• Biliary bypass surgical procedures are performed to provide palliation in unresectable or recurrent tumors.
• Preoperative biliary drainage in patients undergoing pancreatic surgery for malignancy is commonly performed but is associated with an increased incidence of infection and pancreatic fistulae (Lillemoe, 1999).
• Choledochojejunostomy or hepaticojejunostomy can be done to relieve jaundice caused by extrahepatic obstruction.
• A Roux-en-Y choledochojejunostomy can be done to treat obstruction of the common bile duct near the cystic duct junction. This procedure involves taking a loop of the jejunum and anastomosing it to the common or left hepatic duct.
• Insertion of external biliary drains has been used to relieve obstruction preoperatively and for inoperable tumors. External drains require more nursing care, including flushing, dressing changes, and skin care; tubes may need to be changed every few months to prevent occlusion.
• Insertion of internal biliary stents, endoscopically or percutaneously, has become accepted practice for palliative management. Endoscopic retrograde cholangiopancreatography (ERCP) of malignant obstructive jaundice. Stents may be plastic or metal. However, percutaneous transhepatic stent placement is associated with a high risk of sepsis, biliary leakage, and hemorrhage (Joseph et al., 1986). Currently, internal expandable stents are acceptable for use in patients with a very limited life span (Lee et al., 1997).
2. Administration of antibiotics: Cephalosporins covering both gram-negative and gram-positive bacteria are commonly used.
3. The preprocedural workup includes review of the procedure and obtaining informed consent. Check laboratory results for coagulation parameters, prothrombin time, activated partial thromboplastin time, hematocrit, white blood count, platelet count, and liver function tests.
4. The period immediately after stent or drain placement requires close monitoring of the site and tube for signs of wound infection and tube patency. Temperature is monitored for infection. Assess for complications such as sepsis, peritonitis, hemorrhage, and pneumothorax. A sterile dressing change should be done every day for the first 5 days, then every 2 to 3 days. The nurse should monitor laboratory results, checking for electrolyte and bicarbonate imbalances. The bilirubin level should return to normal within 10 days after the procedure.
5. Care of external biliary drains or percutaneous transhepatic biliary stents should include teaching the patient and family about the skin, dressing, and catheter care. The drain is flushed every 8 to 24 hours with 10 to 20 mL of normal saline to keep the lines patent. The skin and exit site should be checked twice a day for signs of skin breakdown or infection. The skin around the drain should be washed daily, or more often if drainage occurs, and a clean dressing should be applied. The patient or family should be taught basic drain care and how to check for and report signs of infection, such as persistent pain, fever, or chills. Signs of stent occlusion or dislocation, such as recurrent jaundice or pruritus, should be reported immediately.
6. Pruritus is a frequent symptom in malignant biliary obstruction. The accumulation of bile salts in the skin is presumed to be the causative mechanism for pruritus, but other mediators that may contribute are histamine, kallikreins, prostaglandins, substance P, and endogenous opioids (Khandelwal & Malet, 1994). Pruritus associated with biliary obstruction can range from mild to severe. Several medications are used to manage the condition, with varying efficacy:
• Cholestyramine 4-6 g PO 30 minutes before meals to absorb bile acids. Side effects include fat malabsorption, possible altered absorption of other medications, and constipation.
• Antihistamines, such as hydroxyzine 25-50 mg PO TID. Major side effects are drowsiness, dizziness, and dry mouth. The sedative effect may be helpful for aiding sleeping
• Phenothiazines, such as prochlorperazine 10 mg PO q8h. Side effects include sedation, akathisia, extrapyramidal reactions, dry mouth, and orthostatic hypotension.
• H2-receptor blockers, such as ranitidine 150 mg PO BID, can be added to any of the previously listed medications if symptoms persist. Side effects include dizziness, headache, and diarrhea.
• 5-HT3 antagonists, such as ondansetron, have been used for cholestatic pruritus (Radere et al., 1994). Side effects may include headache, dizziness, and myalgias.
• Topical steroid creams, such as triamcinolone 0.1% ointment/cream BID. Steroid creams should never be used long term.
• Creams compounded with antidepressants, such as doxepin, may also be tried. They are thought to inhibit H1 and H2 receptors, thus reducing pruritus.
• Cream mixture of local anesthetics lidocaine and prilocaine (EMLA) BID to affected areas.
• Skin care includes bathing using mild soap and oil or lotion without alcohol. Moisturizing agents such as Aveeno, Aquaphor, and Neutrogena Sesame Oil are helpful for dry skin. Provide assistance with frequent turning and repositioning. Keep the patient’s nails trimmed short and filed to reduce trauma from scratching. Avoid hot baths. Cool compresses may be applied to the skin during episodes of acute pruritus. Cool, dry temperatures may reduce sweating and pruritus.
7. Pain may or may not be present with obstruction, depending on the etiology of the obstruction. The patient with pancreatic cancer may have a significant amount of pain, requiring pain assessment with around-the-clock or long-acting opioids. Perform a detailed pain assessment, and teach the patient to keep a diary of pain intensity, as well as the use of analgesics, and their effectiveness. Ongoing pain assessment and evaluation are required.
8. Nausea and anorexia can lead to altered nutrition. The impact of low-grade nausea on nutrition and quality of life should not be underestimated. Nausea should be assessed regularly and controlled with antiemetics including:
• Phenothiazines, such as prochlorperazine 10 mg PO q6h or 10 mg IV or IM q4h. Side effects include sedation, akathisia, extrapyramidal reactions, dry mouth, and orthostatic hypotension.
• Serotonin antagonists, such as dolasetron or Anzemet, may be helpful, but unfortunately many insurance companies cover the cost of these agents only for chemotherapy-induced nausea. Side effects include headache and dizziness. The nurse should regularly evaluate the effectiveness of the medications.
• Nonpharmacologic approaches for low-grade nausea include relaxation, hypnosis, imagery, diversion, and dietary modification.
9. Nutrition: Anorexia and altered taste occur with elevated bilirubin and liver function tests. Nutritional supplements and small, frequent, high-calorie, high-protein snacks are better tolerated than large meals. The patient should avoid drinking liquids close to snack time to avoid feeling full. For some patients, cold food may be more appealing than warm food with aromas. It is important to teach the family to offer snacks without pushing food. Enteral or parenteral supplements may be appropriate to consider as an early intervention in patients with a good prognosis or in malnourished patients with stable disease. Appetite stimulants may be helpful, such as megestrol acetate 400-800 mg PO daily or 80 mg PO 4 times a day. Side effects may include rash and fluid retention. Sensitive patient and family education for the terminally ill should include the anticipation of continual weight loss as an expected symptom.
10. Patients in the terminal phase should be treated and kept comfortable with palliative nursing care. Consultation with the palliative care nurse practitioner is helpful for developing a plan of care, reviewing and suggesting medications, and providing patient and family education and support.
EVIDENCE-BASED PRACTICE UPDATES
1. For patients with unresectable pancreatic tumors, a randomized trial has demonstrated a reduced hospital stay and similar morbidity and mortality with endoscopic stent placement compared to surgical bypass (Anderson et al., 1989).
2. Endoscopic stent placement has increased recurrent jaundice caused by an occluded or dislodged stent, and cholangitis occurs in 13% to 60% of patients (Frakes et al., 1993).
3. Quality of life is improved in patients with biliary obstruction from unresectable liver metastases, cholangiocarcinoma, and pancreatic carcinoma with surgical bypass or endoscopic or percutaneous stenting combined with adjuvant radiation and chemotherapy (Smith et al., 1994).
4. Positive psychosocial outcomes have been seen with placement of biliary stents (Ballinger et al., 1994).
5. No survival advantage is seen between palliative surgical bypass and nonsurgical palliation of obstruction in patients with unresectable malignancies. Surgery is associated with greater morbidity and mortality than endoscopic placement of stents (Smith et al., 1994).
6. Long-term patency rates in biliary stenting are difficult to measure because of the high mortality rate among patients with malignant biliary obstruction. However, longer stents with smooth-surfaced polymers or an antibacterial coating show median patency rates of 6 months (polymers) and 5 months (antibacterial coating), an improvement over plastic stents (Seitz et al., 1994).
TEACHING AND EDUCATION
External biliary catheter care: Show the patient and family members how to provide catheter care and how to observe for signs of bile leakage. Instruct them when to notify the physician or nurse about unusual findings during catheter care. Explain the following: The catheter is placed to straight drainage, and daily output is measured. Daily temperature is monitored for the first week, and elevations must be reported to the health care provider. Internal-external catheters can be capped after 24 hours to move the flow of bile into the duodenum. Biliary tubes require flushing three times a week. Catheters should be replaced every 3 to 4 months, because they may break or become occluded over time.
Skin care and products for pruritus: Review these products and provide the patient and family with a list of medications for pruritus; include the name, purpose, dosage, route, frequency, and side effects.
Nausea and vomiting: Explain that nausea and vomiting may occur if obstruction returns and as the disease progresses. Review medications for nausea; list the name, dosage, route, frequency, and side effects.
Palliative and hospice care: For patients who have advanced cancer, introduce the concept of palliative care and explain the hospice care services that are available.
NURSING DIAGNOSES
1. Acute pain related to biliary obstruction and/or procedure/surgery
2. Impaired skin integrity related to pruritus
3. Hyperthermia related to elevated body temperature
4. Imbalanced nutrition: less than body requirements related to anorexia and nausea
5. Ineffective coping related to acute condition
EVALUATION AND DESIRED OUTCOMES
1. The patient’s pain score will be zero or at an acceptable level.
2. The patient’s skin will be intact and the level of pruritus will be acceptable.
3. The patient’s temperature will be normal.
4. The patient will be able to tolerate oral intake without nausea or vomiting.
5. Jaundice will resolve, and bilirubin levels will return to normal.
6. the patient will be able to set realistic goals with regard to health expectations.
DISCHARGE PLANNING AND FOLLOW-UP CARE
• Signs and symptoms of complications of chronic internal or external drainage need to be reported: right upper quadrant pain, skin infection, bleeding, leakage of bile, rib erosion, and ascites.
• External biliary drainage tubes require regular flushing and dressing changes.
• Routine tube changes usually are necessary at 8- to 12-week intervals to prevent total occlusion.
• Laboratory tests for electrolyte and bicarbonate depletion must be monitored periodically.
GASTRIC OUTLET OBSTRUCTION
PATHOPHYSIOLOGICAL MECHANISMS
Gastric outlet obstruction is complete or partial obstruction of the distal stomach or proximal duodenum, which prevents the stomach contents from emptying completely into the duodenum. The normal physiology of gastric motility consists of peristaltic waves caused by contraction of the smooth muscle of the stomach. Normally the pacemaker cells depolarize the smooth muscle cells at a continual rate, called the basic electrical rhythm of the stomach. When food enters the stomach, it stretches, causing further depolarization and strengthening of the peristaltic wave. When the contraction reaches the antrum (the lower part of the stomach), the wave becomes stronger, mixing the food and causing closure of the pyloric sphincter. As peristalsis continues, a small amount of material is forced through the pyloric sphincter into the duodenum. (Corwin, 2000). Hormones released in the small intestine also help to regulate gastric motility. Secretin and cholecystokinin (CCK) are released in response to chyme in the duodenum, which reduces the motility of the stomach. Gastric inhibitory peptide is released in response to fat in the duodenum, which decreases gastric motility (Huether, 2006).
In gastric outlet obstruction, the transport of chyme is partially or completely blocked along the alimentary canal. The obstruction may be caused by a neoplasm growing in the stomach or duodenum, an extramural mass or adhesion, or a tumor in an adjacent organ (e.g., the head of the pancreas), which causes compression. Tumors in the head of the pancreas cause compression of the duodenal C loop, resulting in nausea and vomiting, whereas tumors of the body or tail obstruct the junction of the duodenum and jejunum at the ligament of Treitz (Lillemoe & Barnes, 1995). Other primary tumors that may cause obstruction by direct extension include colon or kidney cancer. As the obstruction persists, gas and chyme accumulate, and gastric motility initially may increase, causing a cramping- or colic-type pain, nausea, and vomiting.
EPIDEMIOLOGY AND ETIOLOGY
The exact incidence of gastric outlet obstruction is not known, but it occurs much less often than intestinal obstruction. Approximately 30% to 50% of patients with advanced gallbladder cancer develop a gastroduodenal obstruction (Jones, 1991). Among patients with pancreatic cancer, 5% have gastric outlet obstruction at the time of diagnosis, and 8% to 25% develop this complication if gastric bypass is not performed (Singh et al., 1990).
RISK PROFILE
• Gastroduodenal obstruction in patients with cancer usually is caused by a primary gastric tumor that is unresectable or by advanced pancreatic cancer.
• Gastric outlet obstruction is a common complication of advanced gastric cancer. Adhesions may contribute to obstruction.
• Malignant conditions that may give rise to gastroduodenal obstruction include gallbladder, pancreatic, colon, and kidney cancers.
• Benign peptic ulcer disease may also be a risk factor.
PROGNOSIS
The prognosis depends on the type and stage of malignancy and the patient’s functional status and response to treatment such as chemotherapy, radiation, or surgical bypass. Curative reconstruction of GI continuity is possible in cases of obstruction caused by early stage primary gastric tumors. Resection for cure is possible in only 15% of patients with pancreatic cancer at the time of diagnosis (Waranapa & Williamson, 1992), and fewer than 20% survive for longer than 1 year after diagnosis (Warshaw & Fernandez-del Castillo, 1992).
PROFESSIONAL ASSESSMENT CRITERIA (PAC)
1. A complete history and physical examination should be done. The presenting symptoms of gastric outlet obstruction depend on the degree of occlusion, and they may occur acutely, insidiously, or intermittently. With a partial obstruction, the patient may present with a recent history of early satiety, anorexia, weight loss, nausea, and vomiting. Pain may or may not be present. With a complete obstruction, the patient usually has severe vomiting of large amounts of undigested food. Hematemesis may be present with gastric tumors.
2. The purpose of the diagnostic evaluation is to confirm the site and etiology of the obstruction so that appropriate palliative interventions can be implemented. Barium contrast studies and endoscopy can demonstrate gastric or duodenal obstruction. Supine and abdominal x-ray films may show dilation and fluid levels proximal to the site of the obstruction.
NURSING CARE AND TREATMENT
1. A surgical consult usually is ordered to determine whether resection is indicated. The nurse’s role is to make sure that the patient and family understand the surgical options and recommendations and to provide preoperative and postoperative care. The goals of surgery are to re-establish gastrointestinal continuity and to relieve symptoms. The type of palliative surgery performed depends on the disease process and the patient’s prognosis and risk factors. Procedures may include subtotal or total gastrectomy (Fig. 17.1), bypass gastrojejunostomy, a Devine antral exclusion procedure (the stomach is transected just proximal to the tumor and a jejunal loop is anastomosed to the proximal stomach), splenectomy, or partial pancreatectomy. During the immediate postoperative period, the patient must be watched for signs of hemorrhage, hypovolemia, hypotension, reflux aspiration, small bowel obstruction, and anastomotic leak. The surgical incision must be examined routinely for signs of infection or fistula formation.
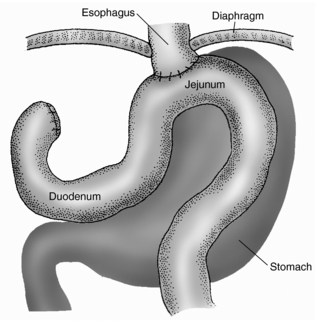 |
| Fig. 17.1Total gastrectomy.(From Ignatavicius, D. D., & Workman, M. L. [2006]. Medical-surgical nursing: Critical thinking for collaborative care. [5th ed.]. St. Louis: Mosby.) |
2. A gastrointestinal consult usually is ordered to determine whether procedures to alleviate the obstruction are an option. The nurse’s role is to assist in explaining the procedure and providing preprocedural and postprocedural care. Insertion of large-caliber stents (16 to 22 mm) is a nonsurgical alternative for treating gastric outlet obstruction that has minimal risks and high success rates. The success rate for self-expanding metal stents is 80% to 100% in gastroduodenal outlet obstructions (Zollikofer et al, 2000). Although stents placed endoscopically across the obstruction may be helpful for relieving symptoms, recurrent stent occlusion may occur.
3. Percutaneous endoscopic gastrostomy (PEG): When surgery is not feasible, insertion of a PEG tube can provide symptomatic treatment. Endoscopically, a stoma is created from the abdominal wall into the stomach, and a short feeding tube is inserted percutaneously. In cases of obstruction, these PEG tubes are used for gastric venting and drainage. A low-profile gastrostomy device (LPGD) has a firm or balloon-style internal bumper or retention disk that prevents the GI contents from leaking onto the skin. Attention to skin and wound care is important.
4. A percutaneous jejunostomy (PEJ) tube may also be used for the delivery of enteral nutrition. PEJ tubes bypass the stomach, allowing feeding below the level of obstruction.
5. Palliative chemotherapy and radiation may provide symptomatic relief, and nursing care aimed at managing treatment side effects is necessary in these cases.
6. Pain may be present, especially with pancreatic tumors, and should be treated aggressively (see Chapter 36).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
