Learning outcomes
By the end of this section, you should know how to:
▪ prepare the patient for this procedure
▪ collect and prepare the equipment
▪ syringe a patient’s ear.
Background knowledge required
Revision of the anatomy and physiology of the external and middle ear
Review of local policy for this procedure.
Indications and rationale for syringing an ear
Impacted cerumen (ear wax) can cause hearing loss, social withdrawal and perforated ear drums (Guest et al 2004). Ear syringing is the removal of this cerumen from the external auditory canal with water or a prescribed solution using specialized equipment. Because of the complications and contraindications related to this procedure it should only be performed by an appropriately trained professional (Harkin 2000).
This may be required:
▪ to clear the external canal of an obstruction that may be blocking it
▪ to wash out softened wax that may be impeding the transmission of sound waves to the tympanic membrane.
Outline of the procedure
Using an auriscope, the external canal and ear drum are examined. If the tympanic membrane is intact and no other abnormalities are detected, the practice of syringing the ear can be carried out. It is sometimes not possible to visualise the tympanic membrane at this stage because of the impacted wax and in this case the patient should be prescribed an appropriate softener, to be instilled as prescribed, to allow the cerumen to be irrigated effectively. Despite the range of softeners, it should be noted that there is a lack of research to support the rationale of choice behind each available make (Guest et al 2004, Hand& Harvey 2004). Under these circumstances, cost and patient compliance must be considered by the prescriber during their assessment.
For some patients the used of a softener for four days may be all that is required for effective removal of the impacted cerumen (Hand& Harvey 2004). However, if cerumen persists following this treatment and if there is no history of a ruptured ear drum, the ear can then be syringed. Although this practice is still called ‘ear syringing’, in practice the use of a metal syringe to irrigate cerumen has been condemned due to the number of cases of damage caused to ear drums, e.g. perforation of the tympanic membrane (Coopey 2001). Over a five-year period in the 1990s, 19% of cases settled by the Medical Defence Union were caused by incorrect ear syringing.
A machine called a Propulse II (Fig. 14.1) is now routinely used for this procedure. This is an electronically operated apparatus with a control dial to ensure a safe and constant delivery of warm water at the optimum pressure for ear irrigation. The use of ‘individual use’ jet tips ensures adherence to infection-control guidelines and the machine is cleansed on a daily basis following the manufacturer’s guidelines. Ears should not be syringed in the following cases:
▪ evidence of a purulent or bloodstained discharge indicating a perforated ear drum
▪ evidence of otitis media in the last six weeks
▪ patients with a cleft palate (due to increased risk of infection due to poor development of the facial bones)
▪ previous ear surgery, unless patients have been discharged from ENT for more than 18 months (Harkin 2000).
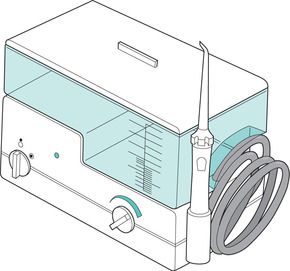 |
| FIGURE 14.1Propulse II electronic ear irrigator |




