Drugs That Affect the Central Nervous System
Objectives
1 Describe how the central nervous system differs from the peripheral nervous system.
2 Explain the role of neurotransmitters at synaptic junctions.
4 Explain how drugs inhibit the actions of cholinergic and adrenergic fibers.
5 Identify two broad classes of drugs used to stimulate the adrenergic nervous system.
7 Review the actions of adrenergic agents and the conditions that require the use of these drugs.
Key Terms
central nervous system ( ) (p. 201)
) (p. 201)
peripheral nervous system ( ) (p. 201)
) (p. 201)
afferent nerves ( ) (p. 201)
) (p. 201)
efferent nerves ( ) (p. 201)
) (p. 201)
autonomic nervous system ( ) (p. 201)
) (p. 201)
neurons ( ) (p. 201)
) (p. 201)
synapse ( ) (p. 201)
) (p. 201)
neurotransmitters ( ) (p. 202)
) (p. 202)
receptors ( ) (p. 202)
) (p. 202)
norepinephrine ( ) (p. 202)
) (p. 202)
acetylcholine ( ) (p. 202)
) (p. 202)
cholinergic fibers ( ) (p. 202)
) (p. 202)
adrenergic fibers ( ) (p. 202)
) (p. 202)
cholinergic agents ( ) (p. 202)
) (p. 202)
adrenergic agents ( ) (p. 202)
) (p. 202)
anticholinergic agents (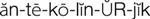 ) (p. 202)
) (p. 202)
adrenergic blocking agents (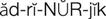
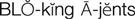 ) (p. 202)
) (p. 202)
catecholamines ( ) (p. 202)
) (p. 202)
alpha receptor (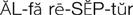 ) (p. 202)
) (p. 202)
beta receptor ( ) (p. 202)
) (p. 202)
dopaminergic receptors ( ) (p. 202)
) (p. 202)
The Central and Autonomic Nervous Systems
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
The control of the human body as a living organism comes primarily from two major systems: the nervous system and the endocrine system. In general, the endocrine system controls the body’s metabolism. The nervous system regulates the body’s ongoing activities (e.g., heart and respiratory muscle contractions), its rapid response to sudden changes in the environment (e.g., skeletal muscles contracting to help an individual to avoid danger), and the rates of secretion of some glands.
The nervous system is comprised of the central nervous system (CNS), which is made up of the brain and the spinal cord, and the peripheral nervous system, which includes the peripheral nerves subdivided into the afferent and efferent nerves. The afferent (peripheral) nerves conduct signals from sensory receptors (e.g., vision, pressure, pain, cold, warmth, touch, smell) throughout the body to the central nervous system. The CNS processes these signals and controls the body’s response by sending signals back through the efferent nerves of the peripheral nervous system. The peripheral nervous system is further subdivided into the somatic nervous system, which controls voluntary movement (e.g., skeletal muscle contractions), and the autonomic nervous system, which, as suggested by the name, works automatically and is not under voluntary control.
Each nerve of the central and peripheral nervous systems is actually composed of a series of segments called neurons. The junction between one neuron and the next is called a synapse. The transmission of nerve signals or impulses occurs because of the activity of chemical substances called neurotransmitters (e.g., transmitters of nerve impulses). A neurotransmitter is released into the synapse at the end of one neuron, thereby activating receptors on the next neuron in the chain or at the end of the nerve chain and stimulating receptors on the end organ (e.g., the heart, smooth muscle, or gland). Neurotransmitters can be excitatory, which means that they stimulate the next neuron, or inhibitory, which means that they inhibit the neuron. Because a single neuron releases only one type of neurotransmitter, the CNS is composed of different types of neurons that secrete separate neurotransmitters. Research indicates that there are more than 30 different types of neurotransmitters; the more common ones throughout the CNS are acetylcholine, norepinephrine, epinephrine, dopamine, glycine, gamma-aminobutyric acid (GABA), and glutamic acid. Substance P and the enkephalins and endorphins regulate the sensation of pain, and serotonin regulates mood. Other neurotransmitters include prostaglandins, histamine, cyclic adenosine monophosphate(cAMP), and amino acids and peptides. Neurotransmitter regulation by pharmacologic agents (e.g., medicines) is a major mechanism that allows for the control of disease processes caused by an excess or deficiency of these neurotransmitters. The use of inhibitory and excitatory neurotransmitters to control illnesses is explained in the rest of the chapters in this unit.
The Autonomic Nervous System
With the exception of skeletal muscle, the autonomic nervous system controls most tissue function. This nervous system helps to control blood pressure, gastrointestinal (GI) secretion and motility, urinary bladder function, sweating, and body temperature. In general, it maintains a constant internal environment (homeostasis) and responds to emergency situations.
There are two main branches of the autonomic nervous system: the sympathetic branch and the parasympathetic branch. The sympathetic and parasympathetic branches typically function in opposition with each other. However, this can be considered complimentary in nature rather than antagonistic. The sympathetic branch speeds up normal processes, and the parasympathetic branch slows down these processes. The sympathetic division typically functions in actions that require quick responses during the “fight-or-flight” response. The parasympathetic division functions as part of actions that do not require immediate reaction during the “rest-and-digest” response.
The two major neurotransmitters of the autonomic nervous system are norepinephrine and acetylcholine. The nerve endings that liberate acetylcholine are called cholinergic fibers; those that secrete norepinephrine are called adrenergic fibers. Most organs are innervated by both adrenergic and cholinergic fibers, but these fibers produce opposite responses. For example, in the heart, the stimulation of adrenergic fibers increases the heart rate, and the stimulation of cholinergic fibers slows the heart rate; in the eyes, the stimulation of adrenergic fibers causes pupillary dilation, and the stimulation of cholinergic fibers causes pupillary constriction (Table 13-1).
Table 13-1
Actions of Autonomic Nerve Impulses on Specific Tissues
| TISSUE | RECEPTOR TYPE | ADRENERGIC RECEPTORS (SYMPATHETIC) | CHOLINERGIC RECEPTORS (PARASYMPATHETIC) |
| Blood Vessels | |||
| Arterioles | |||
| Coronary | α; β2 | Constriction; dilation | Dilation |
| Skin | α | Constriction | Dilation |
| Renal | α1; β1 and β2 | Constriction; dilation | — |
| Skeletal muscle | α; β2 | Constriction; dilation | Dilation |
| Veins (systemic) | α1; β2 | Constriction; dilation | — |
| Eye | |||
| Radial muscle, iris | α1 | Contraction (mydriasis) | — |
| Sphincter muscle, iris | — | — | Contraction (miosis) |
| Ciliary muscle | β | Relaxation for far vision | Contraction for near vision |
| Gastrointestinal Tract | |||
| Smooth muscle | α; β1 and β2 | Relaxation | Contraction |
| Sphincters | α | Contraction | Relaxation |
| Heart | β1 | Increased heart rate, force of contraction | Decreased heart rate |
| Kidney | Dopamine | Dilates renal vasculature, thereby increasing renal perfusion | — |
| Lung | |||
| Bronchial muscle | β2 | Smooth muscle relaxation (opens airways) | Smooth muscle contraction (closes airways) |
| Bronchial glands | α1; β2 | Decreased secretions; increased secretions | Stimulation |
| Metabolism | β2 | Glycogenolysis (increases blood glucose) | — |
| Urinary Bladder | |||
| Fundus (detrusor) | β | Relaxation | Contraction |
| Trigone and sphincter | α | Contraction | Relaxation |
| Uterus | α; β2 | Pregnancy: contraction (α); relaxation (β2) | Variable |
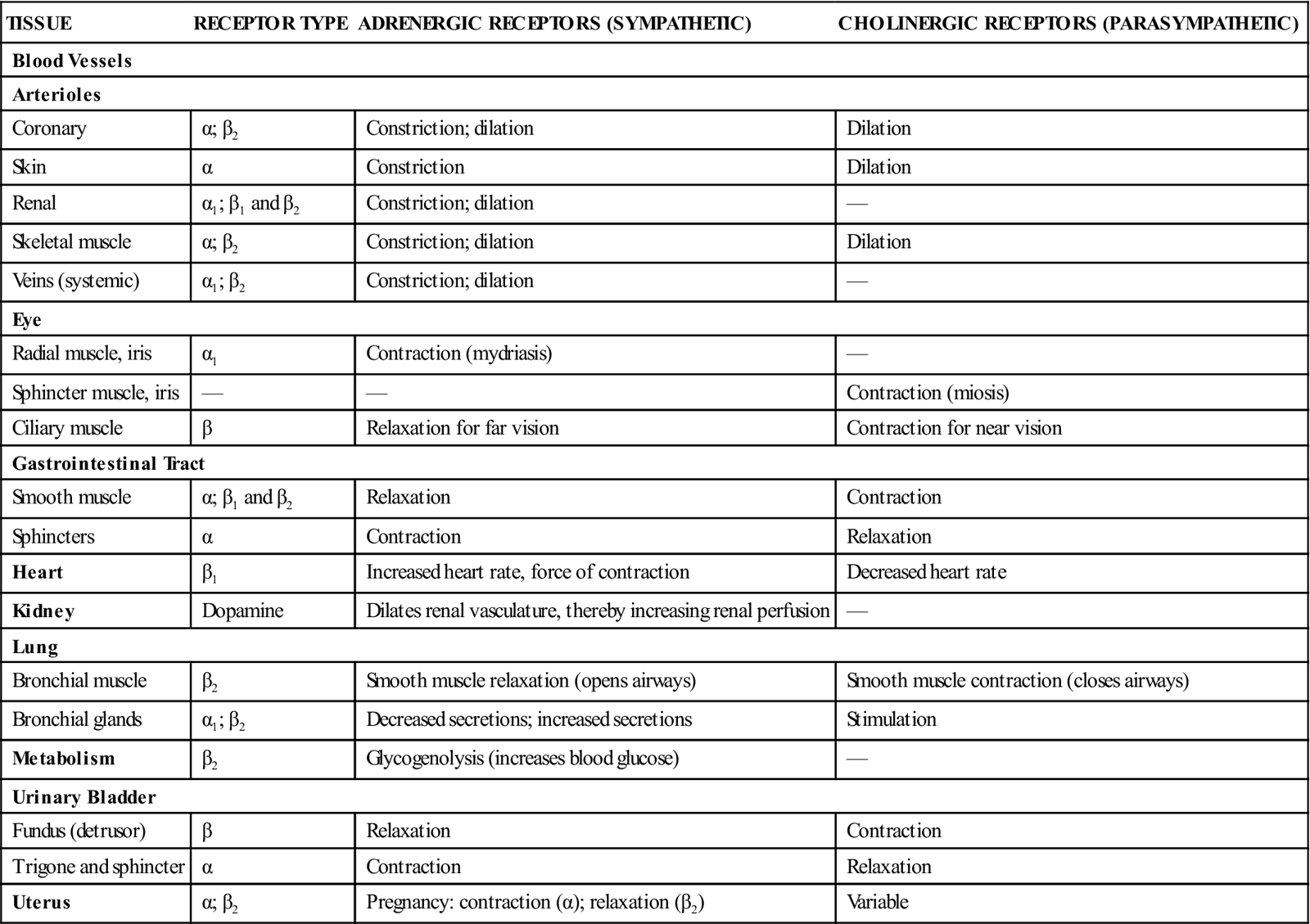
α, Alpha receptor; α1, alpha-1 receptor; β1, beta-1 receptor; β2, beta-2 receptor.
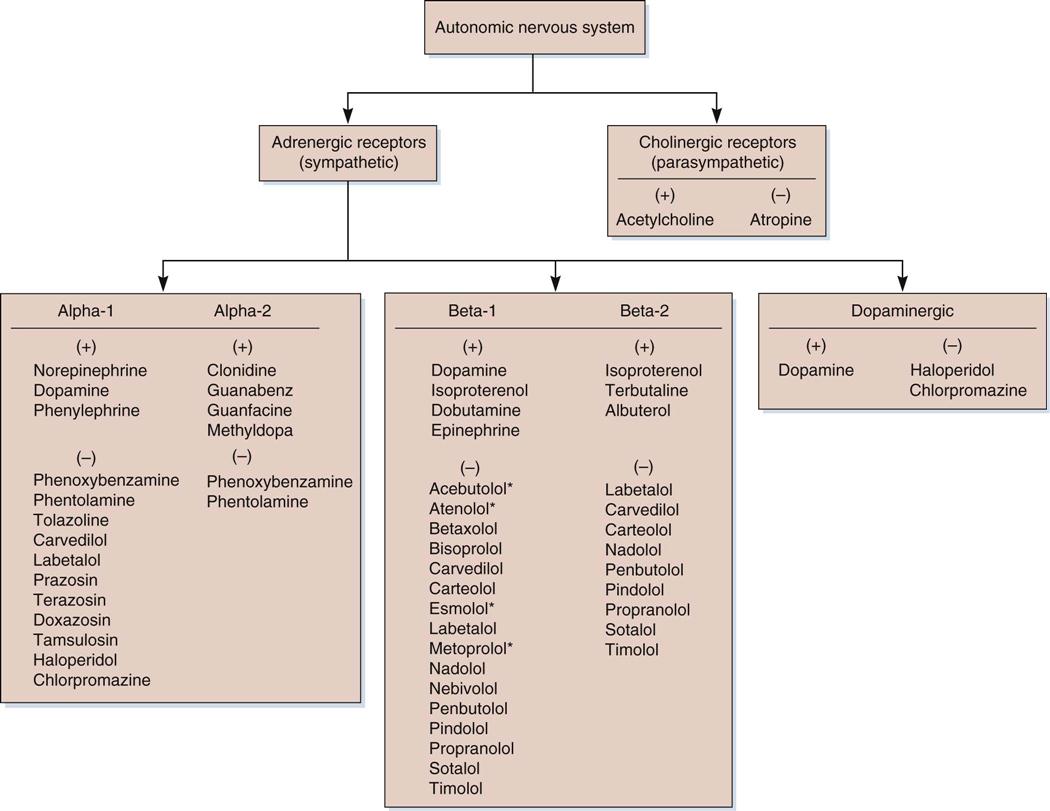
Medications that cause effects in the body similar to those produced by acetylcholine are called cholinergic agents or parasympathomimetic agents, because they mimic the action produced by the stimulation of the parasympathetic division of the autonomic nervous system. Medications that cause effects similar to those produced by the adrenergic neurotransmitter are called adrenergic agents or sympathomimetic agents. Agents that block or inhibit cholinergic activity are called anticholinergic agents, and those that inhibit the adrenergic system are referred to as adrenergic blocking agents. See Figure 13-1 for a diagram of the autonomic system and its representative stimulants and inhibitors.
Drug Class: Adrenergic Agents
Actions
The adrenergic nervous system may be stimulated by two broad classes of drugs: catecholamines and noncatecholamines. The body’s naturally occurring neurotransmitter catecholamines are norepinephrine, epinephrine, and dopamine. Norepinephrine is secreted primarily from nerve terminals; epinephrine comes primarily from the adrenal medulla; and dopamine is found at selected sites in the brain, the kidneys, and the GI tract. All three agents are also synthetically manufactured and may be administered to produce the same effects as those that are naturally secreted. Noncatecholamines have actions that are somewhat similar to those of the catecholamines; however, they are more selective for certain types of receptors, they are not quite as fast acting, and they have a longer duration of action.
As illustrated in Figure 13-1, the autonomic nervous system can be subdivided into the alpha, beta, and dopaminergic receptors. When stimulated by chemicals of certain shapes, these receptors produce a specific action. In general, the stimulation of the alpha-1 receptors causes the vasoconstriction of blood vessels. The alpha-2 receptors appear to serve as mediators of negative feedback, thereby preventing the further release of norepinephrine. The stimulation of beta-1 receptors causes an increase in the heart rate, and the stimulation of beta-2 receptors causes the relaxation of smooth muscle in the bronchi (bronchodilation), the uterus (relaxation), and the peripheral arterial blood vessels (vasodilation). The stimulation of the dopaminergic receptors in the brain improves the symptoms associated with Parkinson’s disease. Dopamine also increases urine output as a result of the stimulation of specific receptors in the kidneys that results in better renal perfusion.
Uses
As noted in Table 13-2, many drugs act on more than one type of adrenergic receptor. Fortunately, each agent can be used for a specific purpose without many adverse effects. If recommended doses are exceeded, however, certain receptors may be stimulated excessively, which can cause serious adverse effects. An example of this is terbutaline, which is primarily a beta stimulant. With normal doses, terbutaline is an effective bronchodilator. In addition to bronchodilation, higher doses of terbutaline cause central nervous system stimulation, which results in insomnia and wakefulness. See Table 13-2 for a list of the clinical uses of the adrenergic agents.
![]() Table 13-2
Table 13-2
| GENERIC NAME | BRAND NAME | AVAILABILITY | ADRENERGIC RECEPTOR | ACTION | CLINICAL USES |
| albuterol* | Proventil, Ventolin | Aerosol: 90 mcg/puff Tablets: 2, 4 mg Syrup: 2 mg/5 mL Tablets, extended release: 4, 8 mg | Beta-2 | Bronchodilator | Asthma, emphysema |
| arformoterol* | Brovana | Nebulizer: 15 mcg/2 mL in 2-mL vials | Beta-2 | Bronchodilator | Emphysema, chronic bronchitis |
| dopamine | — | Intravenous: 40, 80, 160 mg/mL in 5-, 10-, 20-mL ampules | Alpha, beta-1, dopaminergic | Vasopressor | Shock, hypotension; inotropic agent |
| dobutamine | — | Intravenous: 250 mg/20-mL vial; 500 mg/40-mL vial | Beta-1 | Cardiac stimulant | Inotropic agent |
| ephedrine* | — | Subcutaneous, intramuscular, intravenous: 50 mg/mL in 1-mL ampules Capsules: 25 mg | Alpha, beta | Bronchodilator, vasoconstrictor | Nasal decongestant, hypotension |
| epinephrine* | Adrenalin | Intravenous:1 : 1000 in 1-mL ampules; 1 : 10,000 in 10-mL pre-filled syringes | Alpha, beta | Allergic reactions, vasoconstrictor, bronchodilator, cardiac stimulant | Anaphylaxis, cardiac arrest; topical vasoconstrictor |
| formoterol* | Foradil, Perforomist, Oxeze | Capsule for inhalation: 12 mcg Nebulizer: 20 mcg/2 mL in 2-mL container | Beta-2 | Bronchodilator | Asthma, emphysema, chronic bronchitis |
| indacaterol* | Arcapta Neohaler | Capsule for inhalation: 75 mcg | Beta-2 | Bronchodilator | Emphysema, chronic bronchitis |
| isoproterenol | Isuprel | Subcutaneous, intramuscular, intravenous: 0.2 mg/mL solution; 1-, 5-mL vials | Beta | Bronchodilator, cardiac stimulant | Shock, digitalis toxicity, bronchospasm |
| metaproterenol | — | Tablets: 10, 20 mg Syrup: 10 mg/5 mL | Beta-2 | Bronchodilator | Bronchospasm |
| norepinephrine (levarterenol) | Levophed | Intravenous: 1 mg/mL in 4-mL ampules | Alpha-1 | Vasoconstrictor | Shock, hypotension |
| phenylephrine† | Neo-Synephrine | Subcutaneous, intramuscular, intravenous: 10 mg/mL in 1-mL ampules Ophthalmic drops: 0.12%, 2.5%, 10% Nasal solutions: 0.125%, 0.25%, 0.5%, 1% Tablets: 10 mg | Alpha-1 | Vasoconstrictor | Shock, hypotension, nasal decongestant; ophthalmic vasoconstrictor, mydriatic |
| salmeterol | Serevent Diskus | Aerosol powder: 50 mcg/dose | Beta-2 | Bronchodilator | Asthma, emphysema, chronic bronchitis |
| terbutaline* | Brethine, Bricanyl | Tablets: 2.5, 5 mg Subcutaneous: 1 mg/mL in 1-mL ampules | Beta-2 | Bronchodilator, uterine relaxant | Emphysema, asthma |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree