Section Thirteen Cardiac Pacing
PROCEDURE 85 Transcutaneous Cardiac Pacing
Transcutaneous cardiac pacing is also known as TCP, noninvasive cardiac pacing, external cardiac pacing, precordial cardiac pacing, temporary pacing, and external transthoracic pacing.
INDICATIONS
1. To provide emergency pacing in patients with hemodynamically unstable bradycardias (Class I recommendation according to the American Heart Association [AHA], 2005):
2. To increase heart rate in patients with a myocardial infarction who may present with bradycardia-dependent life-threatening ventricular rhythms (Hollander & Diercks, 2004).
3. To provide overdrive pacing in patients with supraventricular and ventricular tachycardias that are resistant to pharmacologic therapy or electrical cardioversion.
CONTRAINDICATIONS AND CAUTIONS
1. Misinterpreting a fine ventricular fibrillation as asystole may lead to inappropriate pacing when defibrillation is indicated.
2. TCP is contraindicated in severe hypothermia because the bradycardia may be physiologic as a result of a decreased metabolic rate (AHA, 2005).
3. TCP is relatively contraindicated in bradyasystolic arrest that lasts longer than 20 minutes because the chance of success is low.
4. Check the manufacturer’s guidelines regarding the length of time the pacing electrodes may be used for continuous pacing.
PATIENT PREPARATION
1. A simple explanation of the purpose and procedure for TCP should be given to the conscious patient. A description of the sensations, including discomfort, that are associated with TCP, and the sedation and analgesia options may be discussed. The sensation at low-current levels has been described as a superficial tingling and at high current levels as a deep thumping. The patient may require continuous reassurance and/or sedation during the procedure.
2. Administer sedatives or analgesics as indicated and prescribed.
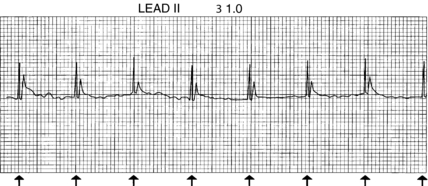
3. Place the ECG electrodes on clean, dry skin. Lead II gives a clearer picture of the pacing artifact (see Procedure 55). The ECG cable must be connected for the pacemaker to operate in the demand mode.
4. Obtain a hard-copy strip of the baseline rhythm along with vital signs.
PROCEDURAL STEPS
1. Following the manufacturer’s recommendations, attach the multifunction or pacing electrodes in either the anterior-anterior (sternum-apex) position (Figure 85-1) or the anteroposterior position (Figure 85-2). The skin should be clean and dry. Remove lotions and ointments with soap and water, and dry the skin completely afterward. No other cleaning agents should be used. Excessive hair should be clipped rather than shaved. Shaving causes microabrasions and increases the likelihood of skin burns. The electrodes should not be placed over wires, drains, dressings, ECG electrodes, implanted cardioverter-defibrillators, pacemakers, or medication patches. Rolling the electrodes onto the skin decreases the amount of air trapped beneath and improves electrical conduction. Press firmly on the adhesive area around the periphery to increase adherence. Press gently on the gelled area to remove any trapped air and to ensure good skin coupling.
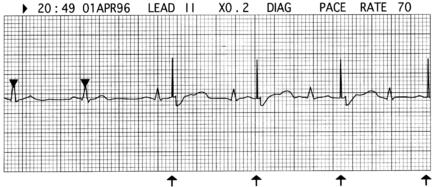
2. Select the pacing mode (demand or asynchronous). In some pacemakers, the mode is automatically “demand” if the ECG cable is attached. It switches to “asynchronous” when the ECG electrodes or cable is removed.
3. Select the pacing rate. The rate range is typically 60 to 100 beats per minute (bpm).
4. Set the output (mA) on zero and turn on the pacemaker.
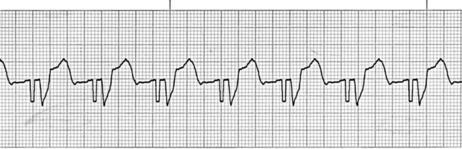
5. Hypoxia, acidosis, pericardial effusion, and tamponade may lead to higher capture thresholds (Del Monte & Gamrath, 1996). The identification of electrical capture may be difficult in the presence of ECG signal distortion (Figure 85-4). An artifact increases in size as the current is increased. Positioning the ECG electrodes as far as possible from the pacing electrodes may reduce the signal distortion. Sometimes changing the lead being monitored minimizes the distortion (Del Monte & Gamrath, 1996).
6. Assess the patient for mechanical capture by palpating a pulse. A Doppler, a pulse oximeter, or both may also assist in identifying and confirming the mechanical capture (Del Monte & Gamrath, 1996).
7. Document the electrical capture with a rhythm strip indicating the pacemaker settings. Document the mechanical capture with vital signs.
8. Assess the patient’s comfort level. Most patients have difficulty tolerating pacing currents above 50 mA. Sedation and analgesia should be used for conscious patients.
9. TCP is a bridge to a more definitive treatment. The patient should be prepared for the insertion of a transvenous pacemaker. See Procedure 86.

Figure 85-1 Sternum-apex electrode placement. In female patients, position the negative electrode under the breast.
(Modified from illustrations supplied by Medtronic Physio-Control Corporation, Redmond, WA.)
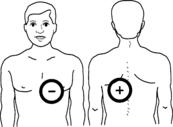
Figure 85-2 Anteroposterior electrode placement. In female patients, position the negative electrode under the breast.
(Modified from illustrations supplied by Medtronic Physio-Control Corporation, Redmond, WA.)
AGE-SPECIFIC CONSIDERATIONS
1. Severe bradycardias in children are usually the result of airway compromise and respiratory insufficiency (Fish, Kannankeril, & Johns, 2006). These issues should be addressed before pharmacologic agents or pacing is attempted.
2. Minimal heart rates indicating possible need for pacing are the following (Conway, 1997):
3. Consider using TCP in children who have primary bradycardia secondary to congenital or acquired heart disease (AHA, 2005).
4. As with adults, discomfort during TCP is a major drawback to its use. Sedation and artificial ventilation should be considered.
5. Smaller-sized pacing electrodes are available for patients who weigh less than 15 kg (ZOLL Medical Corporation, 2006). However, the smaller the pacing electrode, the higher the resistance. Therefore, using a larger electrode is beneficial as long as the adherence is good and the electrodes do not touch.
6. Placement of pacing electrodes in the pediatric population does not differ from that in the adult population (AHA, 2005; Primm & Reamy, 2002). Be sure that the pacing electrodes do not touch; use of the smaller pacing electrodes or an anteroposterior position may be necessary to ensure this in infants and small children.
7. Pediatric patients are at a higher risk for skin breakdown when TCP is used for longer than 30 minutes. In newborns and infants, the area under the pads should be inspected regularly for signs of thermal damage to the skin (ZOLL Medical Corporation, 2006).
COMPLICATIONS
1. Failure to capture is evidenced by pacer spikes that do not induce the wide QRS of an electrical capture (Figure 85-5). A capture threshold may change over time and should be determined frequently when the patient is dependent on a pacemaker (Del Monte & Gamrath, 1996).
2. Undersensing occurs when the pacemaker does not sense an intrinsic QRS and delivers a pacing spike. Failure to sense is recognized by competition between the pacing rhythm and the intrinsic rhythm and by a short interval between the native QRS and the pacing spike (Figure 85-6). If the pacer fails to recognize all the intrinsic QRS complexes, it operates as if it were in the asynchronous mode.
3. Oversensing is due to an inappropriate inhibition of the pacing by electrical signals from outside the heart (Figure 85-7). Extracardiac electrical signals include muscle artifact and electromagnetic signals in the environment. These may be corrected by decreasing the ECG size, which decreases the sensitivity to the native QRS. If the problem persists, it may be necessary to operate the pacemaker in the asynchronous mode to obtain reliable pacing (Del Monte & Gamrath, 1996).
4. Loss of the ECG monitoring leads causes the pacing device to default to asynchronous mode. This can lead to pacing energy being delivered during the heart’s vulnerable period.
5. Prolonged pacing (longer than 2 hours) in patients with poor peripheral perfusion can result in burns. Monitor the skin under the electrodes frequently (ZOLL Medical Corporation, 2006).
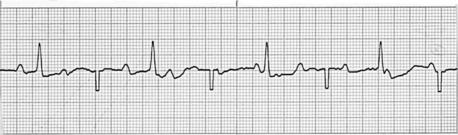
Figure 85-5 Failure to capture. Pacing stimuli fail to capture in a patient in complete heart block.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree