Section Twelve Electrical Therapy
PROCEDURE 82 Synchronized Cardioversion
PROCEDURE 83 Automated External Defibrillator Operation
PROCEDURE 84 Emergency Management of the Patient with an Implantable Cardioverter-Defibrillator
PROCEDURE 81 Defibrillation
Defibrillation is also known as direct-current countershock, electrical countershock therapy, unsynchronized cardioversion, or defib. The word defibrillate refers to an effect on the heart (deplorizing all myocardial cells simultaneously) and is not synonymous with delivery of a shock from a defibrillator. This section deals only with manual use of defibrillators; see Procedure 83 for information on the automatic external defibrillator.
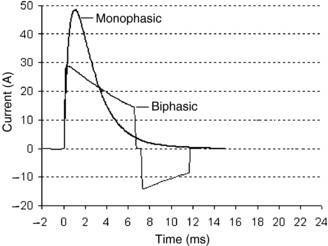
Since 1996, external defibrillators have been available with two different types of energy waveforms: the monophasic and the biphasic. In a monophasic defibrillator, the electrical current travels in one direction between the paddles or electrodes. In a defibrillator that has a biphasic waveform, the electrical current starts in one direction and then reverses direction part way through (Figure 81-1). This allows the peak current delivered by a biphasic shock to be lower than the same peak current delivered by a monophasic shock. The majority of currently produced defibrillators now exclusively use some form of biphasic energy waveforms. The American Heart Association (AHA) (2005) has not made a recommendation for optimal biphasic defibrillation energy levels, but biphasic shock energies of 200 joules (J) or less are safe and effective. “The consensus is that it is reasonable to use 150 J to 200 J for the initial shock with a biphasic truncated exponential waveform or 120 J with a rectilinear biphasic waveform” (AHA, 2005, p. IV-208). Other studies have provided data demonstrating good results for cardioversion of atrial fibrillation and defibrillation of ventricular fibrillation with biphasic shocks up to 360 J (Jain & Wheelan, 2002).
CONTRAINDICATIONS AND CAUTIONS
1. Rapid defibrillation is crucial to increase the patient’s chance of survival. For each minute that passes, there is a 7% to 10% reduction in successful defibrillation (AHA, 2005).
2. Successful defibrillation depends on the metabolic state of the myocardium. Factors that affect the metabolic state include severe hypothermia, hypoxia, acidosis, and electrolyte imbalances.
3. Transthoracic impedance, or resistance, to current flow can affect the ability to defibrillate the myocardium. Factors that determine transthoracic impedance include:
4. Remove transdermal medication patches or ointments from the patient’s chest because they may also allow an inappropriate path for the current.
5. The defibrillation electrodes should be placed at least 1 inch away from an implantable medical device (AHA, 2005). Damage can occur if the generator is directly defibrillated. The generator may also absorb the discharged current and thus reduce the chance of successful defibrillation.
6. Defibrillation may become necessary during noninvasive pacing. This may require turning off the pacemaker before the external defibrillation can be performed. Most devices that provide both noninvasive pacemakers and defibrillation disable the pacemaker function when defibrillation is selected. If pacing electrodes have already been applied, hard paddles should neither touch the disposable electrodes nor lie on top of them.
7. An implantable cardioverter-defibrillator (ICD) is an implanted electronic device used in patients who are at high risk for ventricular fibrillation or ventricular tachycardia. An ICD is designed to monitor cardiac rhythms and deliver countershocks if ventricular fibrillation or ventricular tachycardia is identified. If ventricular tachycardia or ventricular fibrillation is present despite an ICD, an external shock should be given immediately. Place the paddles or electrodes at least 1 inch from the ICD. The internal ICD electrodes may cover a section of the epicardium and interfere with the current flow to the heart. If shocks delivered up to 360 J or clinically equivalent biphasic shocks fail to defibrillate the patient, change the paddle or defibrillation electrode placement to an alternative site (anteroposterior or axillary-axillary).
8. Hypothermia. On initial presentation, ventricular fibrillation should be treated with defibrillation. If there is no success with the initial shock, rewarming should be started. Most attempts at defibrillation are unsuccessful when the patient’s core temperature is below 28° to 30° C (82.4° to 86° F) (Danzl, 2006).
PROCEDURAL STEPS
1. Identify ventricular fibrillation or pulseless ventricular tachycardia through a three-lead ECG monitoring system (lead I, II, or III), through the disposable defibrillation electrodes, or through hard paddles (“quick look”).
2. Turn on the defibrillator, making sure the synchronized selection is off.
3. Select an energy level. The first defibrillation is performed with 360 J (monophasic) or 150 J to 200 J with a biphasic truncated exponential waveform or 120 J with a rectilinear biphasic waveform.
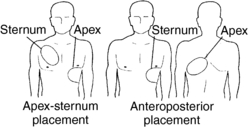
5. Ensure the proper placement of the paddles or the defibrillation electrodes on the chest (Figure 81-2).
6. Say “Clear” loudly, and visually assess that all personnel have no direct or indirect contact with the patient.
7. Deliver a countershock by depressing both discharge buttons simultaneously, or, in the case of disposable electrodes, press the shock button on the device.
8. Immediately resume CPR for 2 minutes or five cycles.
9. Observe the rhythm. If ventricular fibrillation or pulseless ventricular tachycardia persists, deliver another shock at the same or higher energy level. Restart CPR for 2 minutes and then deliver a third shock at same or higher energy level if the second shock is unsuccessful, and proceed with advanced cardiac life-support recommendations. If an organized rhythm results from the defibrillation, check the pulse and obtain a hard copy of the postshock rhythm.
AGE-SPECIFIC CONSIDERATIONS
1. Ventricular fibrillation is rare in infants and children, but it can occur as a result of respiratory arrest. Two J per kilogram is the initial energy delivered to defibrillate, and the strength should be doubled for repeated shocks (AHA, 2005). The AHA (2005) states that biphasic energy settings should be the same as for monophasic defibrillators. There are inadequate data to recommend effective lower doses.
2. For infants and children who weigh more than 10 kg, the AHA recommends using adult electrodes or paddles because the smaller pediatric electrodes increase transthoracic impedance (AHA, 2005).
3. In children and infants, regardless of the electrode or paddle size, they must not touch each other (AHA, 2005).
4. If hard paddles are used, enough pressure should be applied to the paddles so that complete contact with the chest wall is ensured.
5. Neonatal and pediatric patients may be propped on their side and an anteroposterior paddle placement may be used (AHA, 2005). This may be helpful if only adult paddles or disposable electrodes are available.
COMPLICATIONS
1. Skin irritation, redness, or burns may result if an inadequate conductive medium is used or if there are multiple countershocks.
2. Arcing of the current may occur if the defibrillation gel is spread across the chest wall.
3. A current literature search does not yield any references to bystander death due to contact with a patient during defibrillation. However, there have been documented cases of harm requiring hospitalization.
American Heart Association (AHA). American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 112(suppl. IV), 2005. Available online at www.circulationaha.org
Danzl D.F. Accidental hypothermia. In: Marx J.A., Hockberger R.S., Walls R.M., et al. Rosen’s emergency medicine: Concepts and clinical practice. 6th ed. St Louis: Mosby; 2006:2236–2254.
Jain V.C., Wheelan K. Successful cardioversion of atrial fibrillation using 360-joules biphasic shock. American Journal of Cardiology. 2002;90:331–332.
PROCEDURE 82 Synchronized Cardioversion
Synchronized cardioversion is also known as cardioversion, direct-current synchronized countershock, and electrical synchronized countershock therapy. The goal of synchronized cardioversion is to deliver a defibrillation shock outside the relative refractory period of the electrocardiogram (ECG) cycle (Barnason, 2003), protecting the patient from going into ventricular fibrillation.
Cardioversion may be performed with either a monophasic or a biphasic waveform (see Procedure 81). The cardioversion energies given below are all monophasic. If the defibrillator is a biphasic unit, use the clinically equivalent energy dose as provided by the manufacturer. Jain and Wheelan (2002) presented three case studies in which 360 joules (J) of biphasic energy was used without adverse effects.
INDICATIONS
1. To terminate ventricular tachyarrhythmias in a patient who has a pulse. Patients who are stable are given oxygen and antiarrhythmic medications as the first line of treatment. Synchronized cardioversion is used if these methods fail (AHA, 2005). Patients who are unstable with signs and symptoms related to tachycardia, including chest pain, dyspnea, decreased level of consciousness, low blood pressure (systolic less than 90 mm Hg), pulmonary congestion, congestive heart failure, ischemia, or infarction, are prepared for immediate synchronized cardioversion if the ventricular rate is greater than 150 beats per minute (bpm). A brief trial of antiarrhythmic medications is sometimes used during set-up for the cardioversion. When the ventricular rate is less than 150 bpm, synchronized cardioversion is used after failed trials of medications according to Advanced Cardiac Life Support (ACLS) guidelines. Wide-complex tachycardias of uncertain type may be treated in similar fashion.
2. In the stable patient with narrow-complex supraventricular tachycardia, cardioversion is used only if medication administration and vagal maneuvers fail to convert the rhythm to a normal sinus rhythm.
3. To terminate atrial fibrillation and atrial flutter. Synchronized cardioversion is used as a first-line therapy for atrial rhythms with a rapid ventricular response (more than 100 bpm) accompanied by clinical distress (AHA, 2005). See cautions for patients who have had atrial fibrillation and atrial flutter for longer than 48 hours.
CONTRAINDICATIONS AND CAUTIONS
1. Airway protection may be necessary, especially when the patient is sedated. Intubation equipment and materials must be readily available.
2. The hemodynamic status must be monitored continuously. A sudden deterioration may warrant rapid synchronized cardioversion or an unsynchronized countershock.
3. Premedication with sedative and analgesic medications is warranted if the patient’s condition permits.
4. Remove any transdermal medication patches or ointment from the chest because they may allow an inappropriate path for the current.
5. Digoxin or quinidine toxicity increases the risk of ventricular tachycardia and ventricular fibrillation after cardioversion. Patients receiving a maintenance dose of digoxin therapy can be safely treated with low-dose energy (50 J or less) cardioversion (Bolton, 2004).
6. If the patient is stable, electrolyte imbalances should be corrected before synchronized cardioversion is administered. Hypokalemia can predispose patients to postshock arrhythmias after cardioversion (Hambach, 2005).
7. Cardioversion is not used as the first-line treatment of stable atrial fibrillation and atrial flutter in a patient with onset of the arrhythmia longer than 72 hours prior because there is a risk of embolization of a mural thrombus (Yealy & Delbridge, 2006). Options include rate control with medication, consultation with the patient’s primary care provider, and a search for atrial clots.
8. If the patient’s condition permits, intravenous access should be established before this procedure (see Procedure 60).
9. Paddle or electrode placement must be modified if the patient has a permanent pacemaker or an implanted cardioverter-defibrillator (ICD). Place the paddles or electrodes at least one inch from the implanted device (AHA, 2005). The internal ICD electrodes may cover a section of the epicardium and interfere with the current flow to the heart. If shocks delivered up to 360 J or clinically equivalent biphasic shocks fail to convert the rhythm, change the paddle or electrode placement to alternative sites (anteroposterior or axillary-axillary).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree