Chapter 12 Disorders of the gastrointestinal system
RELEVANT ANATOMY AND PHYSIOLOGY OF THE GASTROINTESTINAL TRACT
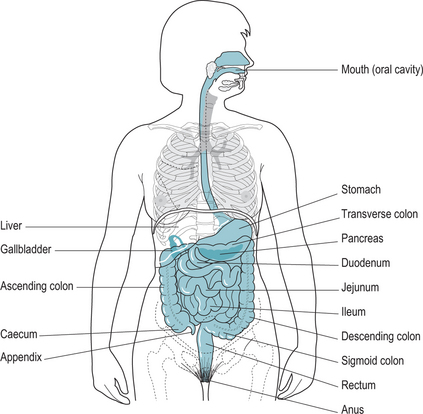
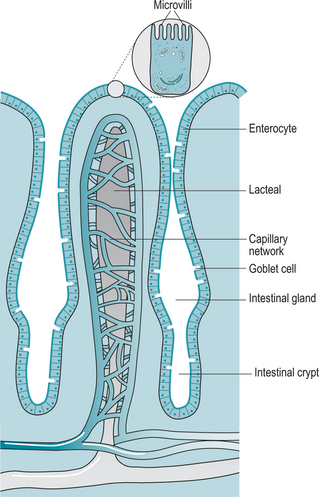
The small intestine extends from the distal sphincter of the stomach to the ileocaecal sphincter at the junction with the large intestine (Fig. 12.1). The small intestine is divided into the duodenum, jejunum and ileum, which are each highly adapted to digestion and absorption. The walls of the small intestine are folded (Fig. 12.2) to produce a large surface area for these processes. Glands secrete mucus and fluids, and the brush border provides enzymes to reduce proteins, carbohydrates and fats to their basic components for ease of absorption.
INFLAMMATORY BOWEL DISEASE
Ulcerative colitis is a disorder of the colon and rectum in which there is severe inflammation and oedema of the intestinal mucosa. Ulceration develops and the individual suffers from diarrhoea, urgency and abdominal pain. Ulcerative colitis varies in intensity and severity between individuals. The more severe forms result in malaise, fatigue and weight loss. Complications of the condition include anaemia, tachycardia, fever and dehydration.
Treatment of both conditions can be medical or surgical. Medical treatment involves the use of anti-inflammatory and immunosuppressant drugs and steroids. Surgery includes removal of the affected part of the intestine. This may cure ulcerative colitis as once removed it does not recur. In Crohn’s disease however, surgery will only be undertaken if there is no other possible treatment, as there is a high incidence of recurrence. Generally surgery involves removal of the affected area and an anastomosis of the two healthy ends although a colostomy/ileostomy may be required (Box 12.1).
INFLAMMATORY BOWEL DISEASE AND CHILDBIRTH
The peak onset of inflammatory bowel disease is between 20 and 40 years of age and thus the impact of the disease on pregnancy is an important clinical issue. Generally, both diseases are thought to follow a similar course that existed before conception, i.e. if in remission, this will continue through pregnancy, while active disease is likely to complicate pregnancy leading to increased maternal and fetal morbidity (Bush et al 2004). The risk of a relapse during pregnancy is considered to be 33%, which is no higher than in those not pregnant (www.crohn’s.org.uk). A relapse is more likely during the first trimester of pregnancy and postnatally. Those individuals who have an ileostomy may find some dysfunction in the later stages of pregnancy when the growing fetus displaces the intestines.
Drugs used in the treatment of IBD are relatively safe for use in pregnancy – certainly the risks of the disease are higher than the risks from the medicines used to keep the condition in remission (Langarragard et al 2007). However, some studies have shown an increase in congenital abnormalities (Alstead & Nelson-Piercy 2003).
Breast-feeding is not contraindicated either by the medication or from the effects of the disease process on the mother. The risk to the neonate of inheriting IBD is thought to be 8–9% (www.crohn’s.org.uk).
IRRITABLE BOWEL SYNDROME
Factors that appear to be involved in this condition are:
Treatment is to examine the diet and consider which if any foods exacerbate the symptoms. Some patients find that cutting out dairy products, red meat, fats, coffee and artificial sweeteners substantially reduces the symptoms of IBS. Pharmacological treatment is based on symptom relief (Bruno 2004).