INTRA-AORTIC BALLOON PUMP
II. Indications
A. Preinfarction angina refractory to pharmacologic therapy
B. Acute myocardial infarction
C. Refractory ventricular arrhythmias related to ischemia
D. Severe mitral valve regurgitation
E. Severe ventriculoseptal defect
F. Before or after heart surgery
G. Low cardiac output states, such as septic shock
III. Contraindications
A. Absolute
1. Aortic aneurysm
2. Bypass grafting from the aorta to peripheral vessels
3. Aortic insufficiency
B. Relative
1. Peripheral or central atherosclerosis
2. Bleeding disorders
3. History of embolic event
IV. Components
A. Consists of a thin, polyurethane balloon mounted on a catheter
B. The catheter is inserted into the patient’s aorta surgically or percutaneously by threading it up through the femoral artery into the descending aorta. Note that the coronary arteries originate from the aorta immediately above the aortic valve.
C. The catheter is connected to a bedside console that shuttles helium into and out of the balloon “in concert” with the cardiac cycle.
V. Therapeutic effects
A. The IABP improves coronary artery perfusion, reduces afterload, and improves perfusion to vital organs.
B. Inflation and deflation of the balloon are automatically timed with the cardiac cycle.
C. The IABP inflates during diastole (when the arotic valve is closed). This displaces blood backward, which increases perfusion to the coronary arteries, and also displaces blood forward, which increases perfusion to vital organs.
D. The balloon deflates just before contraction (systole—when the aortic valve opens). This sudden deflation reduces the pressure in the aorta, decreases afterload, and reduces mycardial oxygen demand. These in turn assist the heart during systole.
VI. Management considerations
A. Vital signs and hemodyamics should be frequently monitored.
B. Ensure accurate timing/pump operation based on any of the following:
1. R wave of the ECG (Figure 12-1)
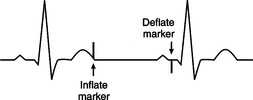 |
| FIGURE 12-1Use of timing markers as a reference on the electrocardiogram (ECG) tracing.(From Mims BC, Toto KH, Leuke LE et al: Critical care skills: a clinical handbook, Philadelphia, 1996, WB Saunders, with permission.) |
2. Upstroke (dicrotic notch [DN]) of the arterial line tracing
3. Spike from a pacemaker
4. Wave form on the balloon pump (Figure 12-2). The following checklist may be used to ensure optimal balloon inflation/deflation:
a. Inflated at the DN
b. Should see a clear V at the inflation point (IP)
c. Peak diastolic pressure (PDP) should be greater than or equal to the peak systolic pressure (PSP).
e. Ensure that the BAEDP is 5 to 15 mmHg less than the patient’s aortic end-diastolic pressure (PAEDP).
f. Note that the assisted peak pressure is less than the PSP.
g. Calculate the end-diastolic dip to reflect the decreased workload of the heart: BAEDP − PAEDP = 5 to 15 mmHg.
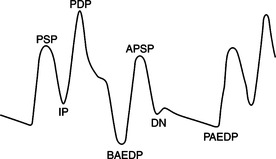 |
| FIGURE 12-2Timing the waveform to check for proper timing of counterpulsation.(From Mims BC, Toto KH, Leuke LE et al: Critical care skills: a clinical handbook, ed 2, St. Louis, 2004, WB Saunders, with permission.) |
C. Involved leg must be kept straight.
D. Head of the bed should be elevated only slightly.
E. Monitor for complications.
1. Lower extremity ischemia related to occlusion of the femoral artery by the catheter or by emboli from catheter thrombus formation
2. Displacement of the catheter related to patient movement
3. Balloon perforation
4. Infection
F. Weaning parameters: hemodynamically stable vital signs, including the following:
1. Normal cardiac index (2.5 L/minute or greater)
2. Normal mean arterial pressure (MAP) (greater than 70 mmHg)
3. Normal pulmonary capillary wedge pressure (6-12 mmHg)
4. Absence of chest pain
5. Absence of other signs of inadequate perfusion
G. Weaning method: either
1. Decrease the volume in the balloon with each inflation (e.g., in periods of 25% reduction), or
2. Decrease the frequency of inflation (e.g., from every cardiac sequence to every other, to every third).
VII. Complications
A. Balloon rupture
B. Embolus
D. Destruction of red blood cells caused by the pump
E. Inability to wean the patient from the pump
PACEMAKERS
I. Definition
A. Electronic devices that deliver stimuli (i.e., impulses) to the cardiac muscle in an effort to maintain adequate heart rate and cardiac output when the patient’s intrinsic pacemaker becomes insufficient
B. May be used for single (ventricular) or dual (atrial, ventricular, or atrio ventricular [AV]-sequential) chamber pacing
II. Primary indications—with symptomatic patients or those refractory to pharmacologic therapy
A. Bradyarrhythmias
B. Heart block
C. Sick sinus syndrome
D. Asystole
E. Atrial tachyarrhythmias
F. Ventricular tachyarrhythmias
III. Components
A. The pacing system consists of a power source, called the pulse generator, that senses the patient’s intrinsic cardiac activity and delivers stimuli to the cardiac muscle on the basis of patient’s intrinsic cardiac activity.
B. The pacemaker contains a unipolar or bipolar lead/electrode catheter that is placed in the right atrium or right ventricle, in contact with the endocardium.
C. The tip of the lead/electrode makes contact with the cardiac muscle and is responsible for transferring electrical stimuli from the pulse generator to the heart.
D. Temporary pacemakers usually have a pulse generator that is external to the body, but the pulse generator of permanent pacemakers is usually internal.
IV. Operational definitions




A. Capture—process that occurs when the pulse generator’s delivered impulse/stimulus is adequate to depolarize cardiac muscle
1. A single-chamber pacemaker will depolarize the atrium or the ventricle, resulting in a large P wave (atrial) or a large QRS complex (ventricular), following the respective pacing artifact (Figure 12-3).
 |
| FIGURE 12-3Medtronic single-chamber pacemaker.(From Mims BC, Toto KH, Leuke LE et al: Critical care skills: a clinical handbook, ed 2, St. Louis, 2004, WB Saunders, with permission.) |
2. A dual-chamber pacemaker will depolarize the right atrium and the right ventricle as needed (Figure 12-4).
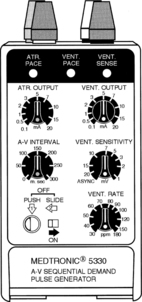 |
| FIGURE 12-4Medtronic atrioventricular (AV) sequential demand pulse generator.(From Mims BC, Toto KH, Leuke LE et al: Critical care skills: a clinical handbook, ed 2, St. Louis, 2004, WB Saunders, with permission.) |
B. Spike/artifact—vertical line that is seen before the R wave or the QRS complex, indicating pacemaker firing (i.e., before the R wave [atrial pacemaker]; before the QRS complex [ventricular pacemaker])
C. Sensing—activity that occurs when the pacemaker recognizes intrinsic electrical activity of the heart. The pacemaker then “resets” the timing mechanism, resulting in inhibition of the pacing stimulus. Sensing is designed to prevent potentially life-threatening competition between the artificial pacemaker and the patient’s intrinsic pacemaker.
D. Rate responsiveness—refers to a special modulation that enables the pacemaker to increase or decrease the rate of firing as needed
E. Programmability—ability to painlessly and noninvasively change pacemaker settings or parameters on the basis of patient needs
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
