CHAPTER 11. Wound Management
Nancy J. Denke
ANATOMY AND PHYSIOLOGY
Skin is the largest organ of the body, receiving approximately one third of the circulating blood volume. It is one of the fastest-growing tissues, regenerating every 4 to 6 weeks4 and plays an important role in homeostatic regulation of the body. 5 Skin is composed of three layers: epidermis, dermis, and subcutaneous tissue (Figure 11-1). The epidermis, or outer layer, provides protection against chemicals and microorganisms and generates cells that promote wound healing. The epidermis is avascular and receives nutrients from underlying blood vessels in the dermis and subcutaneous tissues. 16 Thickness of the epidermis varies with location; it is significantly greater in the soles of the feet and palms of the hand than in the eyelids. Thickening of the epidermal layers (calluses) is caused by repeated pressure or friction, such as that seen with poorly fitted shoes, repetitive actions such as plucking guitar strings, or manual labor such as raking the yard.
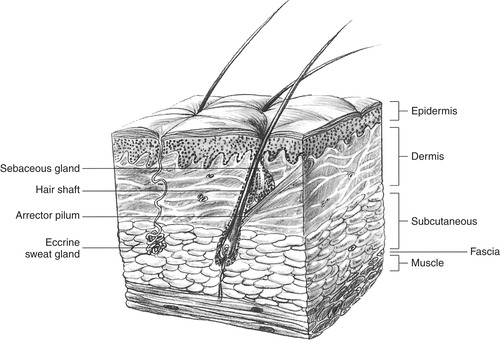 |
| FIGURE 11-1 Epidermis, dermis, and subcutaneous tissue. (From Davis P, Sheldon GF, Drucker WR I: Surgery: a problem solving approach, ed 2, St. Louis, 1995, Mosby.) |
The dermis lies below the epidermis and is composed of collagen and elastin fibers and provides strength, elasticity, and protection against external forces. 4 It is the thickest layer of the skin. The connective tissue of the dermis has a rich vascular supply, along with lymphatic vessels, nerves, and thermoreceptors. Collagen found in the dermis provides tensile strength, whereas elastin allows skin to resist deformation. Collagen is produced by fibroblasts, which become active during inflammatory conditions and wounding. 5 Sensory receptors for pain, touch, pressure, heat, and cold are also found in the dermis, whereas hair follicles and sweat glands are found between the epidermal and dermal layers of the skin.
The subcutaneous layer lies below the dermis and above the muscle tissue, providing body contour. It stores fat below the dermis and provides insulation against heat loss. In addition, the subcutaneous tissue provides protection against injury and acts as an energy storage site. Hypoperfusion of subcutaneous tissue negatively affects wound healing. Complications of impaired healing, such as infections, often have their origin in the subcutaneous tissue. 5
Skin regulates body temperature through sweating and evaporation. Insensible fluid loss through the skin and lungs accounts for 450 to 600 mL/day or 12 to 16 calories/hr of heat loss. 7 Skin provides innate immunity because mast cells and Langerhans cells (macrophages) in the skin respond to antigens and pathogens. The normal skin flora (i.e., coagulase-positive and coagulase-negative staphylococci, streptococci, and diphtheroids) confer a line of defense against other microbes in the environment.
WOUND HEALING
Normal wound healing occurs in three overlapping phases: the inflammatory, proliferative, and remodeling (or maturation) phases. Each phase is sequential, creating the pathway for the next phase to occur.
Inflammatory Phase
The initial, or inflammatory, phase is a protective mechanism that begins immediately with tissue injury and lasts 3 to 5 days. The inflammatory phase begins with the coagulation cascade, platelets adhering to injured vessels to form a clot. It is a complex series of events consisting of cellular and histologic reactions in the affected blood vessels and adjacent tissues. 4 Macrophages (which produce growth factors and cytokines) are attracted to the area, and bacteria and debris are phagocytized and then removed as the body attempts to repair itself. Beneath the clot a network of fibrinogen strands form to unite wound edges. Prostaglandins cause vasodilation, leading to increased capillary permeability, which allows plasma to leak into tissue surrounding the wound, forming “inflammatory exudates.”15 Scab formation begins within 2 hours to minimize fluid loss and prevent bacterial invasion.
Proliferative Phase
The proliferative phase can begin as early as 12 to 72 hours after injury and usually ends approximately 3 weeks later. 4 After scab formation begins, inflammatory processes begin, and the wound becomes painful and edematous. Vasodilation in injured tissues leads to protein leakage and antibody release, which creates a medium for white blood cells arriving at the site 6 hours after injury. White blood cells attack bacteria through phagocytosis by using neutrophils to surround and engulf bacteria, providing short-term defense against infection; monocytes provide long-term defense against infection. Macrophages recruit fibroblasts and create a network of collagen fibers, which in the presence of vitamin C and adequate oxygenation begin the granulation of tissue. 15
During granulation, fibroblast activity peaks, forming new capillary beds, meshing with damaged tissue, and providing oxygen and proteins for tissue growth. During fibroblast activity, collagen is produced for dermal scar tissue. This scar tissue is initially translucent, grayish red, moist, and friable, leading it to bleed easily and become damaged with minimal force. Wound contraction begins following fibroblast formation, angiogenesis, and collagen synthesis and is stimulated by platelet growth factors, prostaglandins, bradykinins, and angiotensin. During contraction, myofibroblasts (fibroblast cells that attach to collagen fibers) pull wound edges closer together and decrease the size of the wound. This wound contraction and remodeling can continue for 6 to 18 months after injury. 5
Remodeling Phase
This third and final phase of wound healing begins about 2 to 3 weeks after injury and can last up to 2 years. 4 Initially collagen fibers develop randomly. However, within 2 weeks these fibers reorganize into thick fibers along stress lines and increase in strength over weeks or months. At 2 weeks approximately 10% to 20% of the tensile strength has returned, whereas at 10 weeks approximately 80% of the preinjury tensile strength has returned. 14 Heredity, stress, and movement of the affected area determine the amount of scarring. Healing, with increasing collagen density and nerve regeneration, may actually take years.
Factors Affecting Wound Healing
Wound healing is significantly affected by preexisting conditions such as arterial/venous insufficiency, lymphedema, morbid obesity, neuropathy, neoplasms, sickle cell disease, infection, diabetes, and malnutrition. 9Table 11-1 describes the effects of preexisting factors on wound healing. Another variable that may affect wound healing is the environment of the patient at the time of the injury. Bacterial contamination on the patient can increase the risk for infection, with wounds of the mouth, perineum, and web spaces of the feet hosting the highest concentration of resident flora. 14
| WBCs, White blood cells. | |
| Factor | Effects on Wound Healing |
|---|---|
| Nutritional deficiencies | |
| Protein | Decreases supply of amino acids for tissue repair |
| Vitamin C | Delays formation of collagen fibers and capillary development |
| Zinc | Impairs epithelialization |
| Inadequate blood supply | Decreases supply of nutrients to injured area, decreases removal of exudative debris, inhibits inflammatory response |
| Corticosteroid drugs | Impair phagocytosis by WBCs, inhibit fibroblast proliferation and function, depress formation of granulation tissue, inhibit wound contraction |
| Infection | Increases inflammatory response and tissue destruction |
| Mechanical friction on wound | Destroys granulation tissue, prevents apposition of wound edges |
| Advanced age | Slows collagen synthesis by fibroblasts, impairs circulation, requires longer time for epithelialization of skin, alters phagocytic and immune responses |
| Obesity | Decreases blood supply in fatty tissue |
| Diabetes mellitus | Decreases collagen synthesis, retards early capillary growth, impairs phagocytosis (result of hyperglycemia) |
| Poor general health | Causes generalized absence of factors necessary to promote wound healing |
| Anemia | Supplies less oxygen at tissue level |
WOUND EVALUATION
Initial assessment of wounds follows assessment and stabilization of the airway, breathing, and circulation. Mechanisms of injury can provide clues to severity of injury. Wounds caused by small objects may be superficial, whereas crush injuries by a large dog’s bite can cause significant deep tissue damage. Appearance of the wound provides clues to the difficulty of wound closure. Jagged edges require more skill to close and may not heal as well. The time elapsed since injury is critical because delayed care increases the risk for complications such as infection. Special closure techniques are required for wounds more than 12 hours old.
Patient age, physical condition, current health status, and occupation also affect wound healing. Medical conditions such as diabetes mellitus, secondary peripheral neuropathy, morbid obesity, malnutrition, or use of medications such as corticosteroids can delay wound healing. Aspirin and nonsteroidal antiinflammatory drugs affect coagulation and healing. Patient occupation may influence long-term wound management and compliance with wound care. Social factors should not be overlooked. Patients who smoke often exhibit a delayed wound healing process, thus increasing their risk for infection. Allergy history and immunization status should also be evaluated during initial assessment.
The patient should be assessed for associated injuries such as fractures, dislocations, or neurovascular compromise. Tendon or ligament injuries, presence of a foreign body, and peripheral nerve damage should also be considered and managed appropriately. Wounds that are heavily contaminated at the time of wounding are at an extreme risk for becoming infected. Farming-related accidents and human bites are representative of wounds that are usually heavily contaminated at the time of injury. 14
SPECIFIC WOUNDS
Wounds are categorized into six basic types: abrasions, abscesses, avulsions, lacerations, puncture wounds, and bites. Their severity varies with the cause of injury and amount of tissue damaged. Wounds may be a minor inconvenience that do not alter lifestyle or affect work requirements. More severe wounds may cause significant discomfort and affect self-care, self-image, and work. In some cases, lifestyle is permanently altered. Prevention of a chronic wound caused by a treatable acute injury is always a major concern.
Abrasions
Abrasions occur when skin is rubbed or scraped against a hard surface. Friction removes the epithelial layer and can also remove part of the epidermis so deeper layers are exposed. Examples of abrasions are floor burns, carpet burns, road rash, or brush burns (Figure 11-2). Abrasions have the same physiologic effect as a partial-thickness burn; thus a significant risk for infection exists from loss of skin and its protective properties. Fluid loss also occurs with loss of surface area.
 |
| FIGURE 11-2 Abrasion. (From McSwain NE Jr, Paturas JL: The basic EMT: comprehensive prehospital patient care, ed 2, St. Louis, 2001, Mosby.) |
Foreign bodies left in the skin stain the epidermis and cause permanent scars or a “tattoo.” Cleansing is critical in management of abrasions to prevent this complication. Local anesthesia by topical application or infiltration should be used for abrasions with heavy contamination. Topical antibiotic ointment and nonadherent dressings are used; however, abrasions may occasionally be left open to air. Dressings should be changed daily until eschar forms. Clothing or sunblock should be used for 6 months to prevent discoloration of fragile new tissue.
Abscesses
Localized collection of pus beneath the skin causes an abscess. Pus may eventually erupt; however, wound management does not include waiting for this to occur. The wound is cleaned, infiltrated with local anesthetic, and drained. An elliptical area of tissue may be removed to facilitate drainage, and then the wound is packed loosely with iodoform or similar material and covered with loose dressing. Antibiotics are indicated when the patient has a fever or when there is reoccurrence of abscess formation. Follow-up with a health care provider is imperative to closely monitor the patient and wound healing.
Avulsions
An avulsion is full-thickness skin loss in which approximation of wound edges is not possible. A degloving injury is a severe avulsion injury in which skin is peeled away from the hand, foot, or a greater portion of an extremity. Figure 11-3 shows a degloving injury of the scalp. Degloving injuries of the fingers are more common and involve injury to tendons and ligaments. Management includes local anesthesia by injection or topical application followed by irrigation and debridement of devitalized tissue. A split-thickness skin graft is often necessary with large avulsions. The wound should be covered with a bulky dressing to protect exposed tissue.
 |
| FIGURE 11-3 Degloving injury of the scalp. (From Auerbach P: Wilderness medicine, ed 4, St. Louis, 2001, Mosby.) |
Contusions
Blunt trauma that does not alter skin integrity causes a contusion or bruise. Swelling, pain, and discoloration occur with extravasation of blood into damaged tissues. After assessment of neurovascular status, therapeutic interventions include cold packs and analgesia as necessary. Large wounds or those located in an extremity should be carefully observed for cellulitis or development of compartment syndrome.
Lacerations
Lacerations are open wounds caused by shearing forces through dermal layers. Superficial lacerations (Figure 11-4) involve the epidermis and dermis, whereas more severe injuries involve deeper layers, including subcutaneous tissue and muscle (Figure 11-5). Initial interventions focus on controlling bleeding and assessing neurovascular function distal to the injury. Anesthetic should be used to facilitate removal of foreign bodies and excision of necrotic or devitalized tissue. Exploration is indicated when damage to underlying structures is possible. Wound closure involves approximation of edges followed by closure with a tape closure, staples, or sutures. Deeper wounds are closed in layers. After the wound is closed, a thin layer of antibiotic ointment may be applied followed by a nonadherent dressing.
 |
| FIGURE 11-4 Superficial laceration. (Courtesy Thomas Lintner, MD.) |
 |
| FIGURE 11-5 Deep laceration. (From Roberts J, Hedges J: Clinical procedures in emergency medicine, ed 4, Philadelphia, 2004, WB Saunders.) |
Puncture Wounds
Puncture wounds are caused by tissue penetration with a sharp object such as a knife blade or injection from high-pressure nail guns or paint guns, which can exert pressures up to 2000 pounds per square inch (psi). 18 Injection injuries cause more severe damage to underlying tissues than indicated by the appearance of the surface wound. Lack of consistency in therapeutic approach can lead to serious complications in a substantial number of puncture wounds. Because puncture wounds do not have a dramatic appearance, the wounds are often undertreated. Regardless of appearance, the zone of injury and the wound’s proximity to underlying structures should be assessed. Infection is reported in 10% to 15% of puncture wounds.
A greater risk for infection exists in wounds that are more than 6 hours old, large and deep, contaminated with foreign matter and debris, occur outdoors, penetrate through footwear, have osseous involvement, or occur in patients with underlying disease such as diabetes mellitus or immunosuppression. 18 Risk for wound contamination increases with high-pressure injuries. Management includes removal of necrotic tissue followed by drain placement and sterile dressing application. Injuries of this type are at a greater risk for being infected with an anaerobic organism. Morbidity and mortality rates are increased due to a delayed identification of the organisms and increased deep tissue necrosis. Impaled objects should be stabilized until safe removal is possible. A foreign body can be removed if the object is small and if removal does not cause further damage. Plain radiographs may be helpful to identify the location of select embedded objects; however, standard films may not show objects such as small pieces of glass, wood, or plastic. In these cases, xeroradiography, ultrasonography, computed tomography, or magnetic resonance imaging can help locate the object. Fluoroscopy has also been used to successfully identify foreign bodies such as needles or wires. Some objects may be left in place or removed surgically.
Bites
Bites may be caused by animals or humans and involve contusions, avulsions, lacerations, and puncture wounds. Teeth can crush or tear tissue, causing extensive damage. An estimated 1 to 2 million people in the United States are bitten by animals each year; dog bites account for 80% to 90% of these injuries, whereas cat bites are reported in 5% to 18%. Exotic animals such as primates, felines, alligators, and camels also cause bite injuries. Regardless of the source, bite wounds are considered contaminated. Infection, abscess, cellulitis, septicemia, osteomyelitis, tenosynovitis, rabies, tetanus, and loss of body parts are potential complications of bite wounds.
Human bites usually result from fighting, sexual activity, or can be self-inflicted. Accidental bite injuries of the tongue, cheeks, and lips can occur during falls or seizures. Surgical closure may or may not be necessary. Infection is the greatest risk with human bites because human saliva contains 100,000,000 organisms per milliliter, 13 including Staphylococcus aureus, streptococci, Proteus, Escherichia coli, Pseudomonas, and Klebsiellae organisms. 13 More than 3% of these organisms are penicillin-resistant S. aureus. Hepatitis B virus may also be transmitted through human saliva; however, risk for human immunodeficiency virus infection appears to be low. 18 The most serious of these human bites is the “fight-bite,” in which there is penetration of the metacarpal joint capsule by a tooth. These “fight-bites” must be treated with antibiotics because of the high incidence of infection, and the hand must be immobilized to place the joint at rest and improve healing. Immobilization decreases the lymphatic flow and the flow of microflora. 10
Management of human bite wounds includes neurovascular assessment, wound exploration, copious irrigation, debridement of devitalized tissue, and application of a bulky dressing. The wound is initially left open, except for those wounds on the face. Prophylactic antibiotics should be given within 3 hours of ED arrival. The use of penicillin plus a β-lactamase inhibitor (such as Augmentin) is the recommended antibiotic of choice for these bites. Alternative agents include cefoxitin or erythromycin. 6
Animal bites carry the risk for infection, tetanus, and rabies. The Centers for Disease Control and Prevention estimates that as many as 4.5 million dog bites occur annually, with almost 800,000 requiring medical attention; 12% were seen in EDs. 2 Infection occurs in 5% to 15% of dog bite wounds and in a significant number of cat bite wounds. Up to 33 organisms have been identified in dog saliva. Cat saliva contains Pasteurella multocida, an extremely virulent organism that can lead to septic arthritis and bacteremia. An increased risk for infection exists in persons more than 50 years of age and in those with hand wounds, deep puncture wounds, and treatment delays of greater than 24 hours.
Dog bites frequently involve associated crush injury from compressive forces of the canine jaw—up to 400 psi in some breeds—with injury to underlying vessels, bones, and nerves. Most dog bites occur on the extremities, head, and neck, with fewer bites on the trunk. Children are more likely to have wounds on the head, face, and neck. Antibiotic use for dog bites is controversial because there is a very low rate of infection. 10 Of all cat bites, 57% to 86% are puncture wounds caused by the cat’s long, slender fangs, which penetrate deeply into underlying tissue and inoculate the wound with bacteria; these wounds are hard to irrigate and tend to become infected because of this reason. Most cat bites are found on the arm, forearm, and hand. Children are more likely to have wounds on the head and trunk. Organisms commonly found in cat bites include Staphylococcus and Streptococcus species and most often P. multocida.10
Treatment for cat and dog bites is essentially the same: copious irrigation followed by cleaning, debridement, and wound closure for small wounds. It is useful to separate animal bites into high versus low risk when deciding to suture the wound or provide appropriate antibiotic coverage. Proponents of oral antibiotics have two different perspectives on the value of amoxicillin/clavulanate therapy versus amoxicillin and cephalexin therapy. Amoxicillin/clavulanate is assumed to cover staphylococci and Pasteurella species. A single medication taken 3 times a day should have good compliance. In contrast, two-drug therapy with amoxicillin and cephalexin may offer better coverage but may result in poorer compliance. Five days of prophylactic antibiotics is generally considered adequate. 2. and 6.
Although these are less effective options, patients who are allergic to penicillin may use one of the following:
• Cefuroxime (cat)
• Doxycycline (cat)
• Erythromycin
• Trimethoprim-sulfamethoxazole
Clindamycin plus ciprofloxacin (adults) or clindamycin plus trimethoprim-sulfamethoxazole (pediatrics) may provide better coverage. Azithromycin may be an effective alternative because of high tissue concentration. 2. and 6. High-risk wounds include all human and cat bites; hand and foot wounds; wounds surgically debrided; puncture wounds involving joints, ligaments, tendons, and bones; bites with delayed treatment more than 12 hours; and bites in immunocompromised patients. These wounds generally should not be sutured, but they do require antibiotics. Hand bites should also be splinted in a position of function and elevated. Low-risk wounds include bites involving the extremities, face, or body. These wounds are generally sutured and do not require antibiotic coverage unless already infected. Rabies and tetanus prophylaxis should be considered for all patients.
WOUND PREPARATION
There are two methods of wound cleaning used to remove bacteria and contamination with foreign material. High-pressure irrigation, the preferred method, is excellent in removing debris and decreasing the rate of infection. Appropriate personal protective equipment should be used because of probable exposure to splashing body fluids. Cleansing the wound by direct contact (such as using a soft brush) is effective in wound debridement but potentially destroys tissue. The wound can be cleansed with isotonic saline or other acceptable solutions (Table 11-2). Hydrogen peroxide should not be used because it causes absorption of oxygen in the wound and cell destruction and gives no protection against anaerobes. Soaps with strong cleaning agents or those containing alcohol may cause further tissue damage. Wounds with heavy contamination must be irrigated for a minimum of 5 minutes; at times lengthier irrigation may be needed. A wound culture may be obtained before or after irrigation if gross contamination is present.
| PMN, Polymorponuclear neutrophil. | ||||
| Agents | Antimicrobial Activity | Mechanics of Action | Tissue Toxicity | Indications and Contraindications |
|---|---|---|---|---|
| Povidone-iodine solution (iodine complexes) (Betadine) | Available as 10% solution with polyvinylpyrrolidone (povidone) containing 1% free iodine with broad rapid-onset antimicrobial activity | Potent germicide in low concentrations | Decreases PMN migration and life span at concentration >1% May cause systemic toxicity at higher concentrations; questionable toxicity at 1% concentration
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree

Get Clinical Tree app for offline access

| |