There are two parts to this section:
1 Insertion of a central venous catheter
2 Measuring and recording central venous pressure
Learning outcomes
By the end of this section, you should know how to:
▪ prepare and support the patient for this nursing practice
▪ collect and prepare the equipment
▪ assist the medical practitioner with safe insertion of the central venous catheter
▪ monitor and record the central venous pressure (CVP)
▪ care for the central venous catheter.
Background knowledge required
Revision of the anatomy and physiology of the cardiovascular system, especially the heart, main vessels and veins of the neck and upper thorax
Indications and rationale for monitoring central venous pressure
A central venous line may be required for three main reasons:
▪ to enable the rapid or high-volume fluid infusion of irritant substances (e.g. cytotoxic drugs or total parenteral nutrition)
▪ to monitor the venous pressure
▪ to allow frequent venous blood monitoring.
The CVP recording is the measurement of the pressure in the right atrium of the heart and is quantified in cmH2O. Sixty per cent of the circulating blood volume is held within the venous system, the CVP being the product of blood volume and venous tone. The pressure recorded reflects the circulating fluid volume; this may need to be assessed in seriously ill patients in whom a close monitoring of fluid balance is needed. It may be indicated:
▪ for the preoperative monitoring of patients who have suffered haemorrhage or trauma to monitor fluid balance closely
▪ for postoperative monitoring following major surgery, especially when intravenous therapy or parenteral nutrition is being administered, to monitor fluid balance
▪ for patients who have severe dehydration, for example after vomiting, diarrhoea or haemorrhage, to monitor fluid replacement therapy
▪ for patients who have cardiac disease, to monitor fluid overload
▪ for patients who have renal disease, to monitor fluid overload
▪ for patients who have acute renal failure during haemodialysis or ultrafiltration procedures to monitor fluid balance.
1. INSERTION OF A CENTRAL VENOUS CATHETER
Outline of the procedure
This procedure is carried out by a medical practitioner using an aseptic technique. The procedure involves the passage of a catheter through the veins to the superior vena cava or the right atrium of the heart (Fig. 11.1). The catheter is then connected to the manometer and giving set, and an intravenous infusion is commenced (see ‘Parenteral nutrition’, p. 237).
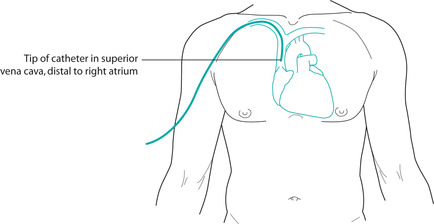 |
| FIGURE 11.1Central venous pressure: position of the catheter in relation to the heart |
The position of the patient
The position of the patient is important during this procedure and is dependent on the choice of the entry site for catheterisation. Veins on the right side are usually selected because they provide easier access to the heart than do those on the left (Royal College of Nursing 2003). There are three main entry sites (the first two being more frequently used; Royal College of Nursing 2003).
The subclavian vein
The patient lies supine with the arms by his or her side. The head of the bed is lowered by 10° to lessen the danger of an embolus occurring.
The patient lies supine, with no pillow, and with the neck extended. The head is rotated away from the site of entry and well supported in position. The head of the bed is lowered by 10°. This position is important to prevent an air embolus occurring.
The median cephalic vein
The patient lies supine. The chosen arm is extended with the palm upwards and the elbow supported to ensure easy access to the entry site.
Additional equipment
1. Sterile gown
2. Sterile gloves
3. Minor operation sterile pack or sterile drape and towels
4. Waterproof protection for the bed
5. Alcohol-based antiseptic for cleansing the skin. Evidence suggests that alcohol-based chlorhexidine is more effective than iodine solution (Pellowe et al 2004)
6. Scissors or clippers to remove any body hair from the intended site of insertion (Royal College of Nursing 2003)
7. Venous pressure manometer set
8. Non-viscous sterile intravenous fluid, e.g. normal saline or dextrose 5% (which will be prescribed by the medical practitioner)
9. Appropriate sterile catheter depending on the site of entry used, e.g. a single-, double- or triple-lumen catheter (Fig. 11.2)
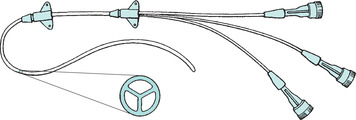 |
| FIGURE 11.2Triple-lumen catheter |
10. Sterile needles and black silk sutures
11. ECG monitoring equipment if required
12. Local anaesthetic and equipment necessary for its administration.





