Chapter 10 Thyroid disorders
RELEVANT ANATOMY AND PHYSIOLOGY
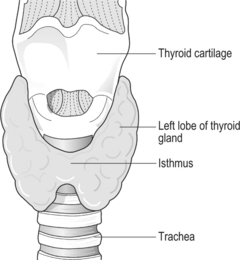
The thyroid gland is an endocrine gland, responsible for producing, storing and secreting the thyroid hormones. The gland is located anteriorly to the trachea, just below the level of the thyroid cartilage, which forms the anterior surface of the larynx, and superior to the cricoid cartilage (Fig. 10.1).
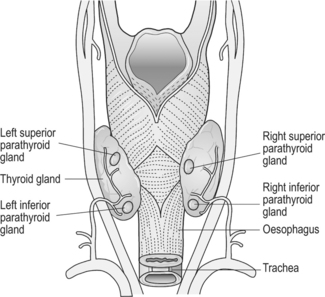
The thyroid gland is shaped like a ‘butterfly’, having a right and left lobe joined by a narrow isthmus; normal weight in adults is 15–25 g. The thyroid gland has an extensive blood supply from the superior and inferior thyroid arteries, which are branches of the subclavian and external carotid arteries. Venous blood drains into three veins – superior and middle thyroid veins drain into the internal jugular vein. The inferior thyroid veins anastomose with each other and drain into the left brachiocephalic vein in the thorax. Four parathyroid glands are located behind the thyroid gland on its posterior aspect (Fig. 10.2)
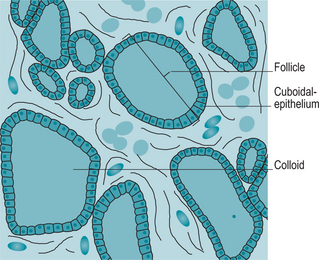
Each lobe of the gland is divided into follicles, and each follicle is lined with a single spherical layer of cuboidal epithelium, surrounding a noncellular centre. The central follicular cavitycontains a viscous gelatinous protein type material in suspension, referred to as a colloid (Fig. 10.3).
Simultaneously, one or two iodide ions are attached to tyrosine molecules in thyroglobulin. Tyrosine–iodide ion molecules are paired forming molecules of thyroid hormones, resulting in the formation of the hormone thyroxine, T4 containing 4 iodide ions, and the hormone tri-iodothyronine, or T3 containing 3 ions (Martini 2005).
Thyroid hormones are released in response to hormonal signals from the hypothalamus and pituitary gland. Thyrotrophin releasing hormone (TRH) is secreted into the blood in response to low circulating concentrations of thyroid hormones. This in turn acts on the anterior pituitary which stimulates the secretion of thyroid stimulating hormone (TSH) and as the concentration of thyroid hormones rise, the production rates of TRH and TSH decrease. Therefore, the release of thyroid hormones is controlled by the level of thyroid stimulating hormone in the blood, and control is by a negative feedback system (Box 10.1).
The levels of T4 (thyroxine) and T3 (tri-iodothyronine) circulating in the blood are quite different. The thyroid gland makes more T4 than T3, and T4 has a longer half-life, but significantly, T4 is less active and is used more as a storage form. In the peripheral circulation and at cell level T4 can be converted to T3 (de Swiet et al 2002).
Most of the thyroid hormones entering the bloodstream become attached to thyroid binding globulins, and only very small amounts remain unbound and are free to diffuse into peripheral tissues. Thyroid hormones readily cross cell membranes and they activate receptors involved with energy transformation and utilization; in other words, they regulate the metabolism of nearly all body cells. The critical effects from a midwifery perspective are that the thyroid hormones regulate carbohydrate, lipid and protein metabolism and the normal development of the nervous system in fetus and infant. They also promote normal growth and the hydration and secretory activity of the skin (Table 10.1). Female reproduction and lactation are also influenced (Marieb & Hoehn 2007).
Table 10.1 Effects of thyroid hormones on body organs and tissues
Marieb & Hoehn 2007, Martini 2005, Jordan 2002.
THYROID DISORDERS
Aetiology of thyroid disease
Pathophysiology
Excessive thyroid hormones produce signs and symptoms caused by an increase in the metabolic rate resulting in a variety of symptoms (Table 10.2).
Table 10.2 Symptoms of hyperthyroidism
Management
There are three approaches to treatment of this condition.
Surgery
Partial thyroidectomy is only performed after the patient has achieved a euthyroid state and is useful if there is a large or unsightly goitre. Oral potassium iodide may occasionally be prescribed 1–2 weeks prior to surgery to reduce thyroid size and vascularity and inhibit thyroid hormone release, thereby reducing the risk of postoperative haemorrhage (Watkinson 2003).
Radioactive iodine therapy
Radioactive iodine, iodine 131, may be used to treat hyperthyroidism. It is given orally in a single dose at an outpatient clinic. It acts by destroying follicular cells or inhibiting the cells’ ability to replicate. Patients are advised that eating should be avoided for at least 4 h after administration of the isotope. This is to allow the drug to be absorbed adequately. Following this, the patient should drink at least 2 L of fluid over 24 h in order to excrete the free radioactive iodine as quickly as possible. This treatment is not usually offered to women of childbearing age (Dibbs 2001).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree