There are four parts to this section:
1 Catheterisation
2 Catheter care
3 Bladder irrigation
4 Administration of catheter maintenance solutions
The concluding subsection, ‘Patient/carer education’, and the ‘Self-assessment questions’ refer to the four practices collectively.
Learning outcomes
By the end of this section, you should know how to:
▪ prepare the patient for any of these four nursing practices
▪ collect and prepare the equipment
▪ carry out catheterisation, catheter care, bladder irrigation and administration of catheter maintenance solutions.
Background knowledge required
Revision of the anatomy and physiology of the urinary system and external genitalia
Revision of ‘Wound Care’ technique (seep. 381)
Revision of local policy regarding catheter selection, catheter bags and administration of catheter maintenance solutions.
1. CATHETERISATION
Indications and rationale for urethral catheterisation
An estimated 15–25% of patients admitted to hospital have a urinary catheter passed (Tenke et al 2004). Because of the invasive nature of this procedure, the National Institute for Clinical Excellence (NICE) states that you must be competent before undertaking this nursing practice (National Institute for Clinical Excellence 2003). This competency should minimise the risks to the patient of discomfort, pain and catheter-associated urinary track infection (CAUTI).
Urinary catheters can be inserted:
▪ to re-establish a flow of urine in urinary retention
▪ to empty the bladder preoperatively
▪ to allow the monitoring of fluid balance in a seriously ill patient
▪ to facilitate bladder irrigation procedures
▪ to maintain a dry environment in urinary incontinence when all other forms of nursing intervention have failed
▪ for the administration of medication
▪ to promote comfort for terminally ill patients.
 Equipment
Equipment1. Trolley or adequate surface for equipment
2. Good light source, such as spotlight or torch
3. Sterile gloves
4. Clean apron
5. Sterile catheterisation or dressings pack
6. Mild soap and water and also sterile water-based solution for cleansing the genitalia
7. Sterile anaesthetic gel or water-soluble lubricant if anaesthetic gel is contraindicated
8. Sterile receiver
9. Sterile catheter of the type and size required
10. Appropriate equipment for catheter balloon inflation for non-pre-filled catheters only, e.g. syringe, needles and sterile water
11. Sterile closed drainage system if required, or catheter valve
12. Hypoallergenic tape
13. If requested, sterile specimen container appropriately labelled with a completed laboratory form and plastic specimen bag for transportation
14. Receptacle for soiled disposable items.
Catheters and catheter bags
Catheter type
The reason for urinary catheterisation can dictate the type and size of catheter (Fig. 10.1) to be used:
▪ a round-ended catheter can be used when a retained catheter is not required
▪ a Foley double-lumen, self-retaining catheter can be used when a short-term retained catheter is required
▪ a Foley triple-lumen, self-retaining catheter can be used when continuous bladder irrigation is required
▪ a Tiemann catheter can be used when the urethral canal is narrowed, for example when a male patient has an enlarged prostate gland; the shape of the catheter tip aids the passage of the catheter
▪ a whistle-tipped catheter can be used postoperatively to allow the passage of blood clots, particularly when bladder irrigation is not being utilised
▪ a silastic catheter can be used when a retained catheter is required for long-term use, as silastic is less irritant to the body tissue.
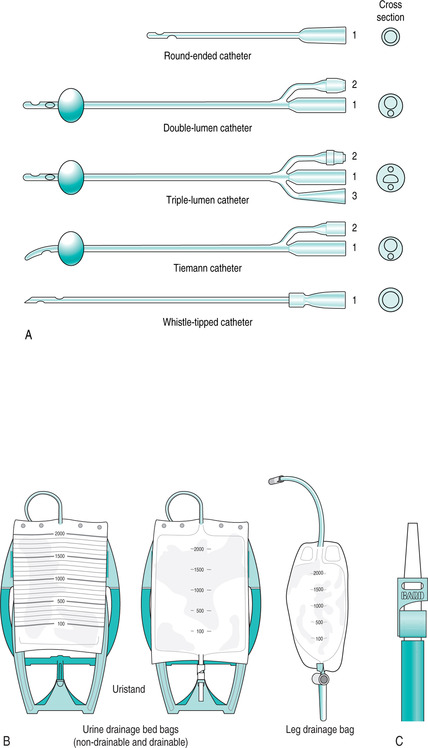 |
| FIGURE 10.1Catheterisation A Examples of catheters (1 channel for urine flow; 2 channel for balloon inflation; 3 channel for irrigating fluid flow) B Types of drainage bag C Catheter valve |
Sizes
The smallest Charriére size that will drain urine should be used (Tew et al 2005). A 10 ml balloon should be chosen unless under specialist advice (Stewart 2001). This is because the drainage eye of the catheter sits higher in the bladder with a 30 ml balloon, allowing residual urine to collect below the balloon, which in turn can lead to infection.
▪ 12–14FG is a suitable size of catheter for female and male patients. Intermittent self-catheterisation catheters are usually 10–12FG in size
▪ catheters are manufactured in female and male catheter lengths, male length catheters being approximately 42 cm long and female ones about 26 cm
▪ for routine use, select a catheter with a 10 ml balloon.
Materials
A variety of catheter materials is available, the choice being geared to the needs of the individual patient.
Short term (2–4 weeks):
▪ a latex catheter (these are rarely used)
▪ a PTFE-coated, latex Foley catheter.
Long term (up to 12 weeks):
▪ a silicone elastomer catheter – latex and silicone
▪ a hydrogel elastomer catheter – latex and hydrogel
▪ a polymer hydrogel catheter – latex and polymer hydrogel
▪ a 100% silicone catheter (latex free but there is a risk of diffusion of water from the balloon, therefore the water in the balloon must be checked regularly)
▪ a plastic nelaton catheter for intermittent self-catheterisation.
Only PVC and 100% silicone catheters contain no latex and must be used in patients with a latex allergy.
Catheter bags
There are three elements to be considered when choosing an appropriate catheter bag: the capacity, the length of the inlet tube and the type of outlet tap for emptying (Tenke et al 2004). The selection depends on the rationale for catheter use, patient preference and the patient’s manual dexterity. The leg bag can be supported by leg straps or by a variety of garments such as net sleeves. A ‘belly bag’ can also be prescribed in place of a leg bag. Worn around the waist this product is manufactured for users who may, for example, have a bilateral amputation (National Health Service Quality Improvement Scotland 2004).
 Guidelines and rationale for this nursing practice
Guidelines and rationale for this nursing practiceFemale patient
▪ explain the nursing practice to the patient to obtain consent and co-operation
▪ collect and prepare the equipment to ensure that all equipment is available and ready for use
▪ ensure the patient’s privacy to reduce anxiety
▪ observe the patient throughout this activity to note any signs of distress
▪ prepare and help the patient into a supine position with the knees bent, the hips flexed and the feet resting on the bed approximately 70 cm apart. This position provides good access to and visualisation of the genitalia
▪ arrange the lighting to assist with good visualisation of the genitalia
▪ wash the hands and put on the gloves, which will act as a barrier between the nurse’s skin and the patient’s tissues, thus reducing the incidence of contamination (National Institute for Clinical Excellence 2003, National Health Service Quality Improvement Scotland 2004)
▪ open and arrange the equipment, maintaining sterility to reduce contamination
▪ cleanse the labia minora, swabbing from above downwards to reduce the danger of cross-infection from the anal region
▪ using the non-dominant hand, separate the labia minora to reveal the urethral meatus. Hold this position until catheter insertion has been completed in order to prevent recontamination of the urethral meatus by the labia minora after cleansing
▪ insert anaesthetic gel or water-soluble lubricant into the urethral meatus to ease the passage of the catheter. The use of an anaesthetic gel is indicated to reduce discomfort and damage to the urethra and to reduce the risk of infection (National Institute for Clinical Excellence 2003). Caution should be used if there is urethral bleeding as this may cause systemic absorption of the anaesthetic. The British National Formulary states that it should be used with caution in patients with cardiac conditions, liver problems and epilepsy (British Medical Association 2005). Allow the time specified by the manufacturer for the anaesthetic to work
▪ with the dominant hand, cleanse the urethral meatus to prevent the introduction of micro-organisms into the urethra and/or bladder and position the sterile receiver to collect the urine from the catheter
▪ insert the lubricated catheter into the urethra in an upward and backward direction, which follows the anatomical route of the female urethra (Fig. 10.2)
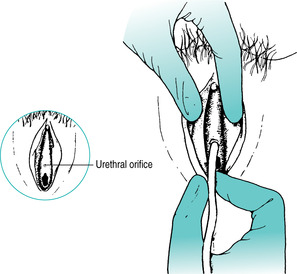 |
| FIGURE 10.2Catheterisation: inserting a catheter into the female urethraFrom Roper et al 1985, with permission |
▪ avoid contamination of the surface of the catheter until a flow of urine has been established, to prevent the introduction of micro-organisms
▪ if it is not intended that the catheter should be left in situ, gently remove the catheter when the urine flow ceases
▪ if the catheter is to be retained, gently advance the catheter 4–5 cm and slowly inflate the balloon according to the manufacturer’s directions. The inflated balloon will maintain the catheter’s position
▪ a complaint of pain may suggest that the inflating balloon is still within the patient’s urethra. Stop the inflation and withdraw the fluid inserted into the balloon. Advance the catheter another 4–5 cm and repeat the inflation process. The length of a patient’s urethra can vary so it is important to adjust practice to meet the individual patient’s needs and prevent complications
▪ attach a drainage system (Fig. 10.3) and properly manage all potential entry points of infection to prevent the development of ascending infection (Morrow 2006)
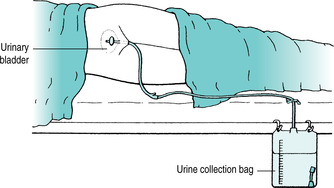 |
| FIGURE 10.3Closed bladder drainage system showing the drainage bag below the level of the bladder |
▪ anchor the catheter when appropriate by supporting the catheter and drainage tubing to reduce trauma to the bladder neck and urethra, which could lead to pressure sore development. Straps, e.g. G-straps are available to assist in this process
▪ dispose of the equipment safely to reduce any health hazard
▪ document the nursing practice appropriately, monitor the after-effects and report any abnormal findings immediately, providing a written record and assisting in the implementation of any action should an abnormality or adverse reaction to the practice be noted.
Male patient
This practice is usually carried out by a medical practitioner, a male nurse or a female nurse who has achieved the required level of competence. A female nurse may prefer to have a chaperone for this procedure.




▪ explain the nursing practice to the patient to obtain consent and co-operation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
