Section 1 General principles of children’s nursing
1.1 Introduction
What to expect
What is expected of the role of the children’s nurse?
 Work as part of the multidisciplinary team
Work as part of the multidisciplinary team
 Provide psychological and physiological care to children that is individualized and holistic
Provide psychological and physiological care to children that is individualized and holistic
 Be an advocate for the child and parents
Be an advocate for the child and parents
 Provide support for the families’ needs
Provide support for the families’ needs
 Care for relatives of the child and significant others
Care for relatives of the child and significant others
 Display appropriate and effective communication skills
Display appropriate and effective communication skills
 Take part in ethical and moral decision making
Take part in ethical and moral decision making
 Assist with and undertake research-based care
Assist with and undertake research-based care
 Accept changing practices and innovations
Accept changing practices and innovations
 Gain an awareness of self-development
Gain an awareness of self-development
 Support and educate less-qualified colleagues
Support and educate less-qualified colleagues
 Record observations/document care
Record observations/document care
The multidisciplinary team (MDT)
Physiotherapist
Development aspects of a child (Piaget theory of development)
The four stages of this theory are:
Preoperational stage: 2–6 years
In the preoperational stage, children’s concerns are:
 Separation anxiety, leading to feelings of insecurity, abandonment, anxiety, loneliness
Separation anxiety, leading to feelings of insecurity, abandonment, anxiety, loneliness
 Inaccurate understanding of the body can lead to fears of mutilation
Inaccurate understanding of the body can lead to fears of mutilation
 Changes in rituals, routines, and an unfamiliar environment can cause a child to feel insecure
Changes in rituals, routines, and an unfamiliar environment can cause a child to feel insecure
 Inability to reason beyond the present and immediate environment so explanations have to be related to the here and now
Inability to reason beyond the present and immediate environment so explanations have to be related to the here and now
 Illness may be seen as punishment so child needs demonstrations of love and affection to reassure him/her about this.
Illness may be seen as punishment so child needs demonstrations of love and affection to reassure him/her about this.
Formal operational stage: 11 years plus
In the formal operational stage, children’s concerns are:
 Altered body image due to puberty
Altered body image due to puberty
 Separation from peers, school and family
Separation from peers, school and family
 Frustration with being dependent on others for help
Frustration with being dependent on others for help
 Threats of helplessness, and strong desire for mastery
Threats of helplessness, and strong desire for mastery
 Dislike of being excluded, so will want to be involved in discussions about care and treatment decisions
Dislike of being excluded, so will want to be involved in discussions about care and treatment decisions
 Prone to construe beyond their knowledge so may assume headaches to be a brain tumour.
Prone to construe beyond their knowledge so may assume headaches to be a brain tumour.
Reflection
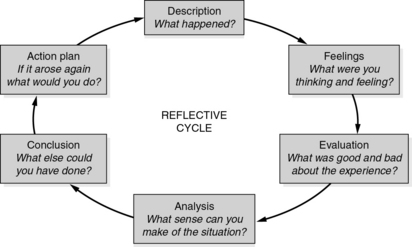
This advocates the use of some sort of guide to ensure this happens and there are many cognitive models of reflection available, for example Boud et al (1985), Gibbs reflective cycle (1988) (see Fig. 1.1) and Johns model of structured reflection (1995) (see Table 1.1).
Table 1.1 Johns’ model of structured reflection (10th edition)
| Write a description of the experience | |
| Cue questions | |
| Aesthetics | What was I trying to achieve? Why did I respond as I did? What were the consequences of that for: the patient? others? myself? How was this person feeling? (Or these persons?) How did I know this? |
| Personal | How did I feel in this situation? What internal factors were influencing me? |
| Ethics | How did I feel in this situation? What factors made me act in incongruent ways? |
| Empirics | What knowledge did or should have informed me? |
| Reflexivity | How does this connect with previous experiences? Could I handle this better in similar situations? What would be the consequences of alternative actions for: the patient? others? myself? How do I now feel about this experience? Can I support myself and others better as a consequence? Has this changed my ways of knowing? |
Boud et al (1985) Returning to the situation
 were the effects of what you did or did not do?
were the effects of what you did or did not do?
 what ‘good’ emerged from this situation?
what ‘good’ emerged from this situation?
 were your experiences in comparison with your colleagues?
were your experiences in comparison with your colleagues?
 are the main reasons for feeling differently from your colleagues?
are the main reasons for feeling differently from your colleagues?
 are the implications for your colleagues or the clients?
are the implications for your colleagues or the clients?
 needs to happen to alter the situation?
needs to happen to alter the situation?
 are you going to do about the situation?
are you going to do about the situation?
 happens if you decide not to alter anything?
happens if you decide not to alter anything?
 might you do differently if faced with a similar situation again?
might you do differently if faced with a similar situation again?
 are the best ways of getting further information about the situation should it arise again?
are the best ways of getting further information about the situation should it arise again?
Critical thinking
Critical thinking involves the development of cognitive processes such as higher-level thinking and reasoning. It encourages the individual to become open-minded, consider alternative perspectives, and respect the right of others to hold different opinions (Clarke & Holt 2001). Critical thinking can be used when situations or problems arise whereby there is no definitive answer. Children’s nurses need to be equipped and ready to find solutions, make decisions, and solve unique and complex problems within their clinical environment. As a children’s nurse you will have to contend with tensions, prioritize care and deal with difficult technical terms when trying to get your view across. Critical thinking can facilitate your expression or articulate to others the sensitivity, complexity of making decisions in practice (Edwards 2007). To think critically, one needs to be inquisitive, curious, enthusiastic, willing to seek the truth and courageous about asking questions to obtain the best action for patients. Table 1.2 shows the phases involved in the critical thinking process.
Table 1.2 Main areas to consider as part of critical thinking
| Phase 1 | ||
| 1. | Interpretation and organization of the information | Descriptions of the situation or problem Logically assemble the information in the mind or on paper Use a concept or mind map starting with a broad concept with linking words that are interrelated and connected. If possible attempt to apply a systematic, organized and diligent approach to the situation (disorganized and abstract is also satisfactory at this time) |
| 2. | Hidden assumptions | What are these? Values, attitudes and beliefs held by all those involved, are they opposite to your own beliefs or interests Consider positive and negative judgements that might be included Try to be open minded |
| 3. | Nursing knowledge involved (both objective and subjective) | Look for the evidence: theoretical/research The ethical principles involved Knowledge from past experiences (personal or professional) Practical knowledge/skills What are your gut feelings about this – use your intuition |
| 4. | Break down the situation/information into parts | Is there a relationship between the parts? How does one effect the other? Analysis – examination of the ideas/arguments and possible courses of action. |
| 5. | Consider all of the options | Include other people’s views/perspectives Continual questioning of the issues involved Consideration of all of the possibilities Flexibility – view the situation in many different ways with a variety of ideas. Be inquisitive, curious, courageous about asking questions to obtain all of the information |
| 6. | Are there any conflicting issues | What are they? Nurse–patient Professional–ethical Nurse–nurse/doctor–nurse/other HCP–nurse Air the concerns with each other Team-working, communication, negotiation skills to resolve conflicts |
| 7. | Consider all of the options, again, synthesizing of ideas | Try to make sense of the muddle that is formulating in your mind or on paper Put them in some type of order with the preferred solution and consider the consequences of one decision over another Delete the ones that no longer apply or there are no resources, can never happen What is the best way forward and why? |
| 8. | A decision has to be made | A decision/solution/conclusion has to be reached Self confidence and trusting own reasoning when making decisions / solving problems |
| Phase 2 | ||
| 9. | Defending the decision | A reason why that decision was made How the decision was reached Has to be explained how the decision was arrived at Justification has to be given |
| 10. | Accountability and responsibility for the decision made | Taking / accepting responsibility for the decision that has been made Being accountable legally, ethically and professionally |
| 11. | Evaluation of the process | Critical reflection/reflective practice Self-regulation/changing practices in the light of new insight and knowledge Correcting oneself if found to be wrong Learning from the situation/process/action plan for future learning needs Personal learning and continuing professional development (CPD) |
| 12. | Creativity and innovation | Implementation of the decision/solution Implementing change, doing things in a different way, being creative and innovative (may go back to the start) Changing, refining or developing new policies/procedures Moving practice forward, doing things differently due to knowledge gained |
Infection control issues
Broad-spectrum antibiotics
 These antibiotics do not only destroy the invading bacteria, but also devastate the normal flora present in the gastrointestinal tract (GIT) and can lead to diarrhoea.
These antibiotics do not only destroy the invading bacteria, but also devastate the normal flora present in the gastrointestinal tract (GIT) and can lead to diarrhoea.
 Broad-spectrum antibiotics destroy resident flora living in the mucous membranes of the mouth and vagina, allowing pathogens (commonly Candida albicans, which causes thrush) to colonize, leading to fungal infections.
Broad-spectrum antibiotics destroy resident flora living in the mucous membranes of the mouth and vagina, allowing pathogens (commonly Candida albicans, which causes thrush) to colonize, leading to fungal infections.
NSAIDs
 Sends messages to the brain and pain may be felt
Sends messages to the brain and pain may be felt
 Simulates the inflammatory response, which leads to swelling, putting pressure on localized nerve endings, resulting in pain, redness and heat
Simulates the inflammatory response, which leads to swelling, putting pressure on localized nerve endings, resulting in pain, redness and heat
 Stimulates the clotting cascade, so any interference with its release can induce bleeding of the nose, vagina, or bleeding from wounds, etc.
Stimulates the clotting cascade, so any interference with its release can induce bleeding of the nose, vagina, or bleeding from wounds, etc.
 Controls renal blood flow and if prostaglandin is reduced then glomerular filtration rate (GFR) will be reduced leading to sodium and water retention
Controls renal blood flow and if prostaglandin is reduced then glomerular filtration rate (GFR) will be reduced leading to sodium and water retention
 NSAIDs are acidic and increase the acidity of the stomach and so can lead to the formation of ulcers; strict adherence to administering these drugs after meal times is essential (Galbraith et al 2008)
NSAIDs are acidic and increase the acidity of the stomach and so can lead to the formation of ulcers; strict adherence to administering these drugs after meal times is essential (Galbraith et al 2008)
 It is essential that children taking NSAIDs should not take other protein-bound anticoagulants (such as aspirin) as these displace highly protein-bound drugs from proteins, leading to more free anticoagulants in the bloodstream
It is essential that children taking NSAIDs should not take other protein-bound anticoagulants (such as aspirin) as these displace highly protein-bound drugs from proteins, leading to more free anticoagulants in the bloodstream
 These drugs reduce the inflammatory response and as such healing mechanism may also be delayed.
These drugs reduce the inflammatory response and as such healing mechanism may also be delayed.
Administration of chemotherapy and radiotherapy
 Administration of chemotherapy and radiotherapy can depress the bone marrow
Administration of chemotherapy and radiotherapy can depress the bone marrow
 Bone marrow produces neutrophils and monocytes, which mature to become macrophages
Bone marrow produces neutrophils and monocytes, which mature to become macrophages
 Administration of chemotherapy and radiotherapy can lead to increased risk of patients becoming neutropenic, which leads to an increased risk of septicaemia.
Administration of chemotherapy and radiotherapy can lead to increased risk of patients becoming neutropenic, which leads to an increased risk of septicaemia.
Steroids
 Steroid hormones are synthesized by the adrenal cortex, and cortisol is a naturally occurring hormone
Steroid hormones are synthesized by the adrenal cortex, and cortisol is a naturally occurring hormone
 Corticosteroids are anti-inflammatory and suppress the immune response, which affects healing; this can lead to susceptibility to infection and impaired wound healing
Corticosteroids are anti-inflammatory and suppress the immune response, which affects healing; this can lead to susceptibility to infection and impaired wound healing
 Patient may be exposed to bacteria, which would not normally breach innate immune defences (Galbraith et al 2008).
Patient may be exposed to bacteria, which would not normally breach innate immune defences (Galbraith et al 2008).
Reduced nutritional intake
Adequate nutritional intake (e.g. glucose, fats, protein, vitamins and minerals) is required to produce the cells and molecules of innate immunity. If nutrients are not available, new molecules and cells cannot be produced, reducing the body’s innate defence’s protection against infection. The nutritional requirements for wound healing (see Section 2) include an adequate protein intake. Proteins supply the amino acids necessary for repair and regeneration of tissues, and produce many of the proteins involved in the immune responses. There are hospital practices that exacerbate bad nutrition and hence affect the child’s immune response:
 Preoperative patients only need to be fasted for 4–6 hours.
Preoperative patients only need to be fasted for 4–6 hours.
 Postoperative feeding should be initiated immediately; leaving fasting until the return of bowel sounds is traditional, ritualistic and unnecessary.
Postoperative feeding should be initiated immediately; leaving fasting until the return of bowel sounds is traditional, ritualistic and unnecessary.
 The prescription of 5% dextrose solution to maintain nutrition only promotes malnutrition as one litre of 5% dextrose solution contains approximately 800 kcal.
The prescription of 5% dextrose solution to maintain nutrition only promotes malnutrition as one litre of 5% dextrose solution contains approximately 800 kcal.
Note: All healthcare professionals and families can reduce the risk of transmission of hospital-acquired infection in children by following infection control practices, as outlined in Table 1.3.
Table 1.3 Infection control practices
| Type | Reasons | Practice |
|---|---|---|
| The use of a single room | This is generally used to protect staff and other patients in the ward area (isolation) or to simply protect the patient due to immunosuppression (protective isolation) | Protective clothing is not generally required, visitors do not go from patient to patient and are not in contact with other patients Visitors do not handle infectious material Wash hands before and after the visitor leave the room is all that is necessary |
| Hand-washing | This is responsible for a large proportion of cross infection, and is the most important method of preventing the spread of infection (Finn 1997) | Thorough hand washing before attending a patient ensures the majority of micro-organisms acquired transiently from other patients are removed An awareness of micro-organisms demonstrates the importance of thoroughly washing and drying hands |
| Protective clothing | The transmission of micro-organisms on staff clothing is possible, but unlikely It is more likely to arise on the front Contaminated uniforms with body fluids increases the microbial load, plastic aprons provide adequate protection as they are impermeable | Plastic aprons under cloth gowns if there is a risk of spillage Disposable gloves for any activity Discarded after use and wash hands If no contact occurs with other patients, infection is unlikely to spread if the nurse leaves the room |
| Masks and eye protection | Recommended for infections that are spread by respiratory droplets They do not work when wet, as damp masks do not filter micro-organisms effectively Efficiency diminishes when worn for long periods Easily contaminated by the hands during repositioning or removal, and as such are unreliable against airborne infections, especially viral (ICNA 1984) | Not necessary for most procedures Are important to protect health care workers and should be worn for any activity where there is a risk of body fluid splashing into the face |
| Waste material | If contaminated with blood or body fluids should be discarded in a yellow waste bag, in the patient’s room The outer surface of waste bags does not become significantly contaminated, no reason to enclose the waste in a second bag | All body fluids should be safely discarded directly into a bedpan washer or macerator |
| Equipment | Beds, curtains, bedclothes, toys, bedpans, sphygmomanometers The majority of micro-organisms are not able to survive in the absence of moisture, warmth and nutrients, then as long as the equipment and other surface areas are kept clean and dry, the potential for the multiplication of bacteria will be removed | If it is known that microorganisms can contain spores and able to survive when food is scarce, hot water or special chemicals may be required to cleaning |
Care planning and documentation
Key points to remember about nursing documentation:
 Should contain all the relevant information needed to care for the child
Should contain all the relevant information needed to care for the child
 Should be a structured plan based on a holistic assessment of the child’s and family’s needs
Should be a structured plan based on a holistic assessment of the child’s and family’s needs
 Should be discussed and planned with both the child and primary carer(s)
Should be discussed and planned with both the child and primary carer(s)
 Should reflect primary carer’s preferred contribution to the child’s care
Should reflect primary carer’s preferred contribution to the child’s care
 Should be personalized to each child
Should be personalized to each child
 Should be written clearly and legibly with black pen
Should be written clearly and legibly with black pen
 Should be updated, reviewed and evaluated regularly to ensure relevancy.
Should be updated, reviewed and evaluated regularly to ensure relevancy.
Nursing process
Assessment
 Explain to the child the purpose of the assessment and seek their agreement
Explain to the child the purpose of the assessment and seek their agreement
 Undertake a comprehensive assessment using a child- and family-centred approach
Undertake a comprehensive assessment using a child- and family-centred approach
 Obtain information directly from the child as much as possible to demonstrate respect for their knowledge and experience
Obtain information directly from the child as much as possible to demonstrate respect for their knowledge and experience
 If assessing a non-verbal child or infant, seek the relevant information from the parents or primary carer
If assessing a non-verbal child or infant, seek the relevant information from the parents or primary carer
 Identify the physical, psychological, social, developmental, cultural, spiritual and sexual needs of the child
Identify the physical, psychological, social, developmental, cultural, spiritual and sexual needs of the child
 Assess and record baseline observations and report anything out of normal range
Assess and record baseline observations and report anything out of normal range
 Ask the child and carer if they have any questions or concerns and address those concerns
Ask the child and carer if they have any questions or concerns and address those concerns
 Provide information about the process and prepare child and carer for what to expect
Provide information about the process and prepare child and carer for what to expect
 Obtain informed consent for any interventions or investigations planned.
Obtain informed consent for any interventions or investigations planned.
Planning
 From the assessment identify the short-, medium- and long-term needs of the child.
From the assessment identify the short-, medium- and long-term needs of the child.
 Take account of how child or young person would like to be involved in the delivery of their care.
Take account of how child or young person would like to be involved in the delivery of their care.
 Take account of parents’, carers’ and family members’ views of the child’s care needs and how they would like to contribute to their child’s care.
Take account of parents’, carers’ and family members’ views of the child’s care needs and how they would like to contribute to their child’s care.
 Then set the goals/outcomes and identify specific interventions to fulfil these goals and expected outcomes.
Then set the goals/outcomes and identify specific interventions to fulfil these goals and expected outcomes.
 Negotiate and agree the care plan with the child and primary carer, taking account of all relevant information.
Negotiate and agree the care plan with the child and primary carer, taking account of all relevant information.
 Agree roles and responsibilities with those involved in caring for the child.
Agree roles and responsibilities with those involved in caring for the child.
 Explain the care plans to the child and family and clarify any information that is unclear.
Explain the care plans to the child and family and clarify any information that is unclear.
 Care plans should be individualized to each child and family situation.
Care plans should be individualized to each child and family situation.
 Document and record all relevant information and communication during the care planning process.
Document and record all relevant information and communication during the care planning process.
Implementation
 Prioritize the interventions required and carry out the interventions according to the care plan.
Prioritize the interventions required and carry out the interventions according to the care plan.
 Ensure care is delivered consistently to meet the goals/outcomes.
Ensure care is delivered consistently to meet the goals/outcomes.
 Work with MDT to meet the identified healthcare needs.
Work with MDT to meet the identified healthcare needs.
 Work in partnership with parents and primary carers to deliver the care required.
Work in partnership with parents and primary carers to deliver the care required.
 Record and monitor child’s response to the interventions.
Record and monitor child’s response to the interventions.
 Keep child and carer informed on the progress and outcomes of interventions and investigations.
Keep child and carer informed on the progress and outcomes of interventions and investigations.
 Be flexible in the delivery of interventions that are non-urgent.
Be flexible in the delivery of interventions that are non-urgent.
Essential skills for preregistration students
1. Care, compassion and communication
2. Organizational aspects of care
3. Infection prevention and control
4. Nutrition and fluid management
Government directives in children’s nursing
 hospital services meet the needs of children, young people and their parents, and
hospital services meet the needs of children, young people and their parents, and
 they provide effective and safe care, through appropriately trained and skilled staff working in suitable, child-friendly, and safe environments.
they provide effective and safe care, through appropriately trained and skilled staff working in suitable, child-friendly, and safe environments.
It would be useful to read the documents that fully outline these standards which can be located on the website www.nhs.uk/NHSEngland/NSF/Pages/Children.aspx.
Voluntary organizations
In Europe the EACH organization (European Association for Children in Hospital) promotes the welfare of all children, before, during and after a hospital stay. EACH is made up of 19 associations from Europe, which promote the care of hospitalized children through the EACH charter. The EACH Charter contains a list of 10 rights for all children in hospital (www.each-for-sick-children.org/each-charter). These are listed in Table 1.4.
Table 1.4 The 10 rights of children in hospital
| Article 1 | Children shall be admitted to hospital only if the care they require cannot be equally well provided at home or on a day basis |
| Article 2 | Children in hospital shall have the right to have their parents or parent substitute with them at all times |
| Article 3 | Accommodation should be offered to all parents and they should be helped and encouraged to stay Parents should not need to incur additional costs or suffer loss of income In order to share in the care of their child, parents should be kept informed about ward routine and their active participation encouraged |
| Article 4 | Children and parents shall have the right to be informed in a manner appropriate to age and understanding Steps should be taken to mitigate physical and emotional stress |