Principles of phlebotomy and intravenous therapy
Intravenous infusion
Learning outcomes
Having read this chapter, the reader should be able to:
• discuss the indications for an intravenous infusion
• describe the different types of fluid solution commonly used for an intravenous infusion
• describe the formula for calculating the flow of an intravenous infusion
• discuss the complications associated with infusion therapy and how these are recognized and managed
• discuss how fluid balance is monitored and the significance of this.
• discuss the role and responsibilities of the midwife in relation to intravenous infusion therapy
Women may require intravenous infusion therapy for a variety of reasons but this can be debilitating for the woman, affect her mobility, body image and independence; consequently she may require assistance in caring for herself and for her baby. Intravenous infusion therapy is not without risk ranging from localized complications to more serious systemic ones. Zheng et al (2014) suggest 20–70% of patients receiving an intravenous infusion will develop infusion phlebitis. This chapter focuses on the skills involved with the setting up, monitoring and discontinuation of an intravenous infusion, including reference to the types of solution commonly used and the monitoring of fluid balance. These are skills primarily used in the hospital setting for the childbearing woman and occasionally the baby.
Definition
An intravenous infusion is the introduction of sterile fluid into the venous circulation through the use of pressure. Access to the circulation is usually via the veins of the back of the hand, wrist or lower arm if intravenous therapy is expected to be short term; the subclavian vein or internal jugular vein is the preferred access site if long-term therapy is required (lasting several days or weeks). The latter is rarely used in midwifery. Infusions can be continuous or intermittent (which may be as a secondary infusion).
Equipment
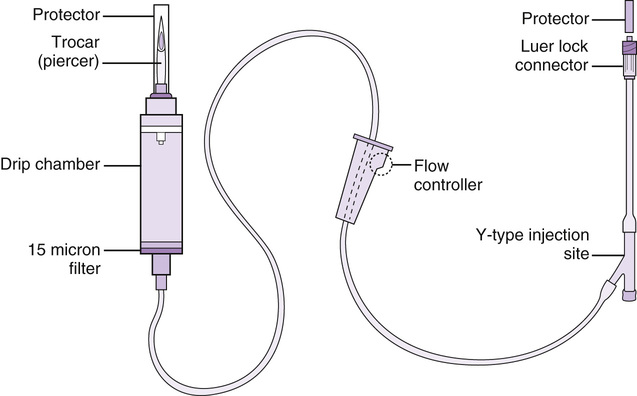
Intravenous administration set (‘giving set’)
These are sterile pre-packed sets consisting of a long piece of air-filled tubing with a trocar at the top end that is inserted into the bag/bottle of fluid, a drip chamber (which may contain a filter), and a nozzle at the bottom end that connects to a cannula. The tubing has an adjustable roller clamp around it that adjusts the fluid flow (Fig. 48.1) which should be positioned on the upper third of the tubing. The position of the clamp should be changed periodically to prevent the tubing from kinking, as it may then attempt to straighten out, pushing the clamp open (Ansell & Dougherty 2011). There are two main types used in midwifery – one for the administration of clear fluids and one for blood transfusion (Chapter 49), the latter having a double chamber and a filter. The tubing has needleless ports through which drugs can be administered.
Calibrated burette sets (volume control devices) can be used when a medical infusion device is unavailable to obtain greater control over the flow rate. Calibrated burette sets allow for very small amounts of fluid to be administered and are more likely to be used in the neonatal unit than the maternity unit or to administer diluted drugs.
The use of a closed system of infusion will reduce the risk of infection; with each connection that is added to the infusion line, the infection risk increases (Ansell & Dougherty 2011). For example, three-way taps (stopcocks) used between the cannula and infusion line are difficult to keep clean and can act as a reservoir for microorganisms, which multiply in the warm, moist environment, increasing the risk of infection (Ansell & Dougherty 2011, Felver 2015).
Medical infusion devices
There are a variety of infusion devices available that allow the infusion flow to be regulated electronically, administering a prescribed amount of fluid over a set time. The midwife should know how the infusion devices work and ensure they are properly cleaned and maintained. Whenever possible, the pump should be connected to a power source to maintain the battery charge. Relying on the battery to continue the infusion for many hours is not best practice. Aceves et al (2013) suggest the battery can die around 2 minutes after the low-battery alarm sounds.
Most of the pumps are smart pumps which can be pre-programmed to create a library of fluids and drugs commonly used in the clinical setting. These bypass the requirement to input the infusion rate and volume manually. Each programme can have predetermined limits which can be set as ‘hard’ – that is, they cannot be overridden – as going above that level would administer a toxic dose or cause harm (Thimbleby & Cairns 2010), or ‘soft’ which can be overridden (Upton & Quinn 2013). Independent double checking of the programme should occur to reduce user error (NPSA 2007).
When pre-programmed pumps are unavailable, the midwife should calculate the rate of infusion (mL/hour) using the manufacturer’s instructions. Generally the formula used is:
For example, if an infusion pump is to administer 500 mL Hartmann’s solution over 4 hours, the rate should be set at:
The use of medical infusion devices does not remove the problem with infusion errors. There are still around 250 patient safety incidents concerning the use of medical infusion devices reported to the National Patient Safety Agency (NPSA) each month (NPSA 2010). The Medicines and Healthcare Products Regulatory Agency (MHRA 2013) found, from their investigation of 1085 incidents between 2005 and 2010, that no cause could be found in 68% of cases (which may be due to insufficient information, incorrect reporting or the device was working as intended). However, user error was the cause for 21% of incidents and 11% were device-related issues.
Syringe pumps
Syringe pumps can be used for the administration of drugs (e.g. insulin, opioids) and are useful when a small volume (50 mL or less) of a highly concentrated drug is required (see Chapter 23) or the drug is to be administered over a set period of time. The fluid/drug is contained within a syringe which is connected to the syringe pump and the plunger is depressed by the pump to deliver at the required rate. A 60-mL syringe is usually the largest size that can be used, with smaller syringes being used for the majority of pumps.
Volumetric pumps
Volumetric pumps are electronic devices that can accurately measure the volume of fluid to be infused and administer at preset rates; different pumps may require different administration sets. An alarm will sound if there is a blockage preventing flow of the fluid, when the fluid volume has been delivered, increased pressure is required (e.g. infiltration) and when the battery is low. Some pumps will alarm if infiltration occurs and obstructs the flow, although deWit & O’Neill (2014) caution that the infiltration can be extensive before it is detected.
Many of the pumps have air detectors to detect and prevent the passage of single bubbles (approximately 100 mcg/L) although they are very sensitive and will alarm more frequently if they detect ‘champagne bubbles’ (MHRA 2013).
Calculating the flow rate of the intravenous fluid when no infusion device is used
When there is no infusion device available, the infusion can be administered using gravity and the flow rate calculated and set manually. The midwife should refer to the administration set being used for details of the number of drops per millilitre, referred to as the drop factor. Commonly the drop factor is 20 for clear fluids, although this can vary between 10–60 drops/mL (Piper 2013) and 15 for blood. The drop factor is determined by the size of the tubing lumen; micro-drips administer 60 drops per millilitre and are useful for the administration of small fluid volumes whereas a macro drip is usually used for rates greater than 75 mL/hour (Bowen 2014). The following formula is used to calculate the number of drops per minute:
For example, if 500 mL Hartmann’s solution is prescribed over a 4-hour period, using an administration set with a drop factor of 20, the flow rate will be:
It is important to ensure the fluid is infused over the correct period of time to prevent over- or under-infusion, both of which can have serious consequences. The flow rate should be checked regularly to ensure it is still running at the correct rate. Piper (2013) suggests every 15 minutes, then when stable, hourly. The flow rate is influenced by a number of factors, e.g. height of fluid in relation to the insertion site, the fluid type, the woman’s blood pressure, movements and position, patency of the cannula and kinks in the tubing (Bowen 2014). Ansell & Dougherty (2011) advise the fluid container can be hung 1–1.5 m above the infusion site for adequate pressure within the infusion to overcome venous pressure and facilitate the flow of the fluid into the circulation. If it is higher, they suggest the intravenous pressure can be too great which can cause infiltration (Ansell & Dougherty 2011). Bowen (2014) suggests that half of the initial flow rate can be lost during the first hour of infusion highlighting the importance of checking and readjusting the rate regularly.
If the infusion is switched on to free-flow, the volume of fluid delivered in a specific time frame will vary. Pierce et al (2013) found that 250 mL phenylephrine placed at 80 cm and running through a micro-drip and an 18-gauge cannula would empty in <10 minutes whereas a 1000 mL bag of crystalloid at 100 cm through a 14-gauge cannula would empty in less than 30 minutes. This again highlights the importance of regularly checking the flow rate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


