Principles of cardiopulmonary resuscitation
Neonatal resuscitation
Learning outcomes
Having read this chapter, the reader should be able to:
Up to 1% of low-risk babies (Rovamo et al 2013) and between 10–20% of all newborns (Schilleman et al 2010, Vento & Saugstad 2011) require ventilatory assistance at birth. Internationally, O’Donnell (2012) advises that between four and seven million babies require resuscitation with 0.06% of babies ≥34 weeks’ gestation needing chest compressions; the sequelae of birth asphyxia is estimated to have a mortality of two million a year with 99% of deaths occurring in developing countries (Murilaa et al 2012). The aim of neonatal resuscitation is to restore tissue oxygen delivery before irreversible damage occurs which may affect long-term neurodevelopment and increase the mortality rate (Harach 2013). Prompt initiation of resuscitation is critical (Amin et al 2013) and the quality of care provided during the first few minutes after birth has a significant effect on long-term health (Rovamo et al 2013). Niermeyer & Clarke (2011) suggest that with each minute resuscitation is delayed, the time to the first gasp increases by about 2 minutes and the onset of spontaneous breathing can be delayed beyond 4 minutes. It is therefore vital that the midwife is able to anticipate and recognize the baby that requires resuscitative assistance at birth and provide this efficiently and competently to reduce morbidity and mortality associated with birth asphyxia.
The International Liaison Committee on Resuscitation (ILCOR) is a multinational group with representation from eight international resuscitation councils – American Heart Association (see Kattwinkel et al 2010), European Resuscitation Council (see Richmond & Wyllie 2010), Heart and Stroke Foundation of Canada (see Finan et al 2011), Resuscitation Council of Asia, Resuscitation Council of South Africa, Australian and New Zealand Resuscitation Council (see NZRC), and the Inter-American Heart Foundation. They review and debate the evidence on neonatal resuscitation and their recommendations are produced as guidelines by Resuscitation Councils across the world. There may be subtle differences between the different Resuscitation Councils according to whether or not they adopt the recommendations in their entirety. The midwife who intends to work in a different country is advised to review that country’s Resuscitation Council guidelines.
At birth there are a number of adaptations the baby has to make to successfully transition from intrauterine to extrauterine life. The airways of the lungs are fluid filled prior to birth and must quickly change to being air filled for effective ventilation to occur. The alveoli in the lungs expand and maintain this expansion with the assistance of surfactant. A functional residual capacity (FRC) is created following the first few breaths. Pulmonary blood flow dramatically increases which assists in the reversal of blood flow through the ductus arteriosus and the closure of the foramen ovale. Negative pressures as high as −80 cm H2O can be generated by the baby with the first breaths, with lower pressures required for subsequent breaths. Lung expansion occurs in conjunction with an increase in the alveolar oxygen tension which results in decreased pulmonary vascular resistance and increased pulmonary blood flow. Oxygen saturation levels increase slowly over the first 5–10 minutes. There is a significant difference in pre- and post-ductal oxygen saturation levels during the first 15 minutes of life. At this point, Beşkardeş et al (2012) suggest it is possible the transfer of blood from right to left along the ductus arteriosus has stopped, increasing saturation levels in the extremities.
Babies who cannot produce adequate alveolar expansion develop respiratory failure and the change in pulmonary vascular resistance does not occur, resulting in persistent pulmonary hypertension, decreased pulmonary blood flow, and hypoxaemia.
Very preterm babies can quickly develop surfactant deficiency preventing the alveoli from maintaining their expansion. They also may have weaker lung muscles, underdeveloped airway protective reflexes and a reduced drive to breathe. Post-mature babies may pass meconium into the amniotic fluid which can be inhaled before or during labour causing inflammation of the lungs and airway obstruction.
Pathophysiology of asphyxia
Asphyxia refers to inadequate tissue perfusion that does not meet the metabolic demands of the tissues for oxygen and removal of waste (Niermeyer & Clarke 2011) resulting in increasing hypoxia, hypercapnia and acidosis. This will cause a change in metabolism from aerobic to anaerobic creating a metabolic acidosis, initially buffered by bicarbonate. As the bicarbonate is depleted, acidosis worsens. The initial response to asphyxia is an increased heart rate followed by decreased cardiac output and peripheral vasoconstriction in an attempt to maintain the blood pressure so that perfusion of the vital organs occurs. As acidosis worsens, cardiac failure can ensue with a decrease in heart rate and blood pressure.
Anticipation
There may be known maternal, fetal or intrapartum factors that increase the likelihood of the need for neonatal resuscitation. In these cases it is advisable for the woman to birth in a hospital where resuscitative equipment and personnel are at hand. These include:
• maternal disease, e.g. pre-eclampsia
• maternal infection, e.g. chorioamnionitis
• fetal abnormality, e.g. diaphragmatic hernia
• intrauterine growth restriction
• ante- or intrapartum haemorrhage
• prolonged rupture of membranes
• malposition or malpresentation, e.g. breech
• abnormalities of the fetal heart rate indicative of fetal compromise
• induction and augmentation of labour
• significant meconium within the amniotic fluid
• instrumental and operative delivery
• obstetric emergency, e.g. cord prolapse, shoulder dystocia.
However, there will always be the unexpected situation in a low-risk setting that reminds the midwife of the importance of ensuring there is access to resuscitation equipment available for every birth, even the homebirth environment, highlighting the requirement that all midwives are trained in and practice neonatal resuscitation on at least a yearly basis so that there is at least one person at the delivery who is trained in newborn life support (Kattwinkel et al 2010, Richmond & Wyllie 2010). Ideally, two midwives are present at each birth allowing one to attend to the immediate needs of the baby and the other to call for emergency assistance. In the hospital environment this may be through the use of the emergency bell or emergency phone number, while in the community the paramedic service should be accessed through ringing 999 or 112.
Training in neonatal resuscitation should occur in the environment and with the equipment with which the midwife works. Multidisciplinary training is ideal as good teamwork behaviours are correlated with higher quality of care during resuscitation (Sawyer et al 2013). Cusack & Fawke (2012) suggest significant decay in psychomotor skills occurs as soon as 3 months following training in resuscitation and advise refresher training and assessment should occur 6 months after attending a resuscitation course to increase retention of knowledge and psychomotor skills.
Equipment
The majority of babies require minimal support with resuscitation necessitating only a small amount of equipment. In the hospital environment it is likely that a standard resuscitaire with additional equipment will be available. The advantage of the resuscitaire is that it comes equipped with a flat surface, good heat and light source, and generally a clock, in addition to equipment for ventilation such as a neopuff/self-inflating bag and the ability to blend air and oxygen. The resuscitaire can be switched on in preparation for the birth so that the environment is prewarmed. All of the equipment should be checked to ensure it is working correctly and the clock started when the baby is born. Some hospitals are fortunate to have a resuscitation table that can be placed next to the bed to allow resuscitation to occur at the bedside with an unclamped umbilical cord so the baby has the benefit of delayed cord clamping (see Chapter 32).
In the home environment the equipment should be laid out ready next to a flat surface and away from draughts with a supply of warm towels available when needed. This may be close to the mother so that if resuscitation is required, it can be undertaken with the cord still attached and unclamped.
Ideal requirements for basic resuscitation in hospital include:
• towels and non-sterile gloves (somewhere to wash and dry hands if time permits)
• pulse oximeter and neonatal probe
• T-piece resuscitator, e.g. neopuff or a self-inflating bag–valve–mask (BVM)
• assorted size facemasks, 00, 01
• Guedel airways, sizes 0, 00, 000
• suction apparatus with tubing and catheters
• polyethylene wrap or food-grade plastic wrapping (for preterm babies <28 weeks).
And for more advanced resuscitation:
Principles of neonatal resuscitation
While these follow ABCD – airway, breathing, circulation, and drugs – there are important steps to be taken beforehand which may result in the baby breathing spontaneously without having to resort to these. The baby is born wet and into a cooler environment which means heat loss can occur quickly. It is therefore important to dry the baby as soon as possible, this will also stimulate the baby and encourage him to breathe spontaneously. It allows the midwife to assess the response of the baby, particularly the tone. A quick assessment is made to determine if respiration is being established and whether the heart rate is above 100 bpm. If not, prompt action is taken, the cord is clamped and cut (if the resuscitation area is not by the bedside), and the baby taken to the resuscitation area. Resuscitation takes priority over delayed cord clamping as there is insufficient evidence to recommend a time for clamping in babies who require resuscitation (Finan et al 2011) and positive pressure ventilation should begin within the first minute of life, sometimes referred to as ‘the golden minute’ (Kattwinkel et al 2010).
It is important to ensure the wet towel is removed and the baby wrapped in a warm, dry towel. Some resuscitaires heat the baby more quickly if the baby is uncovered – it is essential the midwife is aware of how the resuscitaire she is using works to avoid inadvertently preventing the baby from warming up. A cold baby is harder to resuscitate.
There are two exceptions to drying the baby at birth:
1. If the baby is preterm baby <28 weeks’ gestation: The baby should be loosely wrapped in a polyethylene bag/sheet from neck to toe without drying the baby – this should ideally be prewarmed by placing under the radiant heater (not on the radiator as it may melt). The wrapping should take place as close to the time of birth as possible. Once the baby is wrapped, the head should be dried, a hat applied, and the baby stimulated. This will help maintain the baby’s temperature by reducing evaporative heat loss but allowing radiant heat to be transmitted to the baby (O’Donnell 2012). It significantly reduces the risk of hypothermia which has an increased risk of morbidity and mortality for the preterm baby (Rohana et al 2011).
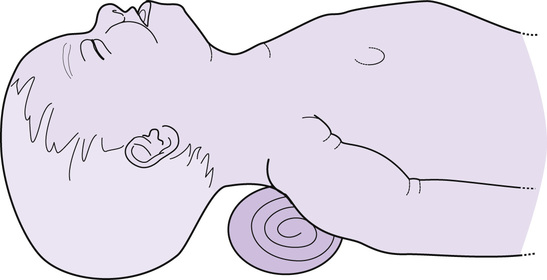
The baby should be positioned so that his head is in a neutral position, neither flexed nor extended, to ensure the airway is open to facilitate air entry into the lungs. This is particularly important with the floppy baby as the loss of pharyngeal tone causes the tongue to fall back and occlude the airway. At birth the prominent occiput (often associated with moulding) of some babies can cause the neck to flex, resulting in airway occlusion. Placing a folded towel/blanket, approximately 2 cm in depth, under the baby’s shoulders will bring the head and neck in alignment and keep the trachea straight (Fig. 56.1).
Assessment of the baby
The baby should now be assessed – breathing, heart rate, and tone:
Heart rate: The gold standard has been to auscultate the apex beat with a stethoscope. Initially the base of the umbilical cord can be palpated but may be unreliable. If the rate is above 100 bpm, Richmond & Wyllie (2010) consider this to be reliable; however, if it is below 100, the apex should always be auscultated. Katheria et al (2012) found both auscultation and palpation of the cord are unreliable in very low birthweight babies, underestimating the heart rate by 14–21 bpm. They recommend attaching electrocardiograph (ECG) leads at birth for more accurate results. Mizumoto et al (2012) also recommend the use of ECG leads over pulse oximetry for determining heart rate, particularly for bradycardic babies with poor perfusion. van Vonderen et al (2015) suggest that ECG is now the gold standard for assessing the heart rate. They found that the heart rate measured by pulse oximetry was significantly lower than that measured by ECG during the first 7 minutes of life for both term and preterm babies particularly during the first 2 minutes (van Vonderen et al 2015). However, Kamlin et al (2008) acknowledge the difficulty in applying the ECG electrodes to wet skin and that they may damage the skin of an extremely preterm baby. They found pulse oximetry provided an accurate display of the baby’s heart rate; pulse oximetry and ECG measure the heart rate differently, particularly in relation to averaging intervals; thus small differences may be seen when both are used (Kamlin et al 2008). When the heart rate changes, the measurement on the pulse oximetry may lag behind the ECG for a few seconds but Kamlin et al (2008) suggest this is not clinically significant. The New Zealand Resuscitation Council (NZRC 2010a) advise that the heart rate should be consistently above 100 bpm within the first minute of life for the uncompromised baby, although Dawson et al (2010) suggest the median heart rate of both the term and preterm babies is <100 bpm (99 bpm and 96 bpm, respectively). These were babies who did not require any resuscitation even though at 1 minute 17% had a heart rate <100 bpm and 7% had a heart rate <60 bpm and all had good tone and normal respiratory effort (Dawson et al 2010). An increasing heart rate is the most reliable sign that the baby’s condition is improving, with a decreasing heart rate associated with a deterioration in the baby’s condition. Assisted ventilation should be given if the heart rate is persistently <100 bpm (NZRC 2010a).
1. Breathing: established, crying
2. Breathing: inadequate or absent and/or
3. Breathing: inadequate or absent
Heart rate: low or undetectable
In the UK, breathing, heart rate and tone should be re-assessed following the first five inflation breaths, then every 30 seconds during resuscitation, as the condition of the baby and the degree of resuscitation required will change. The heart rate should increase in response to adequate ventilation. A pulse oximeter probe should be applied if the baby requires more than a few inflation breaths and then the oxygen saturation reading also becomes part of the 30-second assessment. Note that in some countries, e.g. New Zealand, re-assessment does not occur until 30 seconds of effective ventilation has occurred.
Note that colour is not part of the formal assessment at present, as it can be misleading. It is not unusual for babies to have blue hands and feet and this should not be mistaken for cyanosis. Kattwinkel et al (2010) advise that skin colour is a very poor indicator of oxyhaemoglobin saturation following birth and the lack of cyanosis is also a poor indicator of oxygenation of an uncompromised baby. Additionally, the determination of colour is prone to substantial interobserver variability (O’Donnell 2012). Central cyanosis is noted by observing the mucous membranes inside the lips and gums. If there are concerns regarding the oxygenation of the baby a pulse oximeter should be used to assess the baby’s oxygen saturation level.
Airway
If the baby cannot maintain his own airway, assistance must be given to keep the head in the neutral position.
Chin support
This is achieved by placing a finger under the tip of the chin, on the bone to support the chin upwards. Care must be taken to avoid pressure on the soft tissues as this may occlude the airway.
Jaw thrust
This is particularly helpful when the baby has little or no tone. The midwife places a finger at the angle of the jaw to push the lower jaw outwards and forwards. This may be undertaken as a double jaw thrust using a finger on both sides of the jaw. Two fingers can also be placed on the jaw and below the tip of the chin to assist with maintaining the forward, outward thrust of the jaw.
Use of oropharyngeal (Guedel) airway
If there continues to be difficulty maintaining the airway during resuscitation despite the use of chin support/jaw thrust, the baby has a facial or oral abnormality which makes this difficult (e.g. micrognathia) or the midwife is resuscitating the baby with no assistance, an oropharyngeal airway can be used which will maintain airway patency by keeping the tongue forwards.
It important to use the correct size of airway (0, 00, 000); size is assessed by placing the flange of the airway against the baby’s philtrum and positioning the airway horizontally so the curved part of the airway curves around the baby’s jaw. The correct size will end at the angle of the jaw. Alternatively, measure from the edge of the lips to the bottom of the earlobe. An airway that is too large may cause laryngospasm; one that is too small is ineffective and may worsen the airway obstruction (Johansen et al 2012).
The airway is inserted by opening the baby’s mouth by depressing the chin and sliding the airway over the baby’s tongue without pushing the tongue backwards. It should slide easily into position. If the tongue is obstructing insertion, use a laryngoscope or tongue depressor to gently press down on the tongue while inserting the airway.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


