An integrative approach to prostate cancer
INTRODUCTION AND OVERVIEW
Prostate cancer is a major health issue for men around the world, particularly in developed countries. In Australia, for example, over 18,000 men are diagnosed with it per year and it kills over 3000 patients each year.1 There were 679,000 new cases of prostate cancer worldwide in 2002, making it the fifth most common cancer in the world and the second most common in men (11.7% of new cancer cases overall; 19% in developed countries and 5.3% in developing countries).2 It is the most common cause of cancer-related death in men.3 It is the most common non-cutaneous malignancy and there are around 250,000 prostate cancer deaths each year worldwide.4
AETIOLOGY
The causes of prostate cancer are essentially unknown, although it is estimated that up to 40% of prostate cancers may have an inherited component, according to twin studies.5 Furthermore, there is approximately a 40-fold difference in the reported incidence and a 12-fold difference in mortality rate of prostate cancer between various geographic and ethnic populations.6 The highest reported incidence of prostate cancer is in Afro-American men.7 Men with a family history of prostate cancer also have an increased risk of developing prostate cancer.8 There is a two-fold risk with one first-degree relative and a five-fold risk with two first-degree relatives.8 Results from migrant studies provide strong evidence of the importance of environmental and lifestyle factors in the development of prostate cancer.9 Recently, there has been considerable interest in the role of diet and other lifestyle factors in the initiation, promotion and progression of prostate cancer.10
PREVENTION
A few studies have been undertaken to determine whether prostate cancer can be prevented by taking 5-alpha-reductase inhibitors (finasteride and dutasteride).11–13 The finasteride (Proscar®) trial showed a 25% reduction in the prevalence of prostate cancer over a 7-year period; however, there has been some concern that there may be a slight increase in the incidence of more aggressive tumours, but subsequent, more careful analyses have not supported this.12,14 Currently, chemo prevention with finasteride is therefore not recommended by most urologists.
Further major studies that have recently been reported include a prevention study using dutasteride (Avodart®) and another study, the SELECT trial, using selenium and vitamin E, and studying 30,000 men. The dutasteride study (REDUCE trial) reported a 20% decrease in the detection of prostate cancer after only 4 years of follow-up in a slightly higher-risk group of men without any increase in detection of high-grade disease. There was a 4% increased incidence of reduced libido, similarly to the finasteride study. The SELECT trial reported no benefit in taking selenium and vitamin E in the prevention of prostate cancer. It was, however, performed in a country not deficient in selenium.15–18
Other medications that have been implicated in possible prevention are the statins, for which there is currently low-level evidence of a possible risk reduction19–21 and toremifene, a selective oestrogen receptor modulator that has shown some experimental evidence in animals for a reduction in incidence.22
There is now some evidence-based dietary advice that GPs can give their patients on how to reduce their risk of prostate cancer (Box 50.1). Obesity, high saturated fat intake and high calorie intake may increase the risk of developing prostate cancer.23,24
BOX 50.1 Evidence-based dietary advice on how to reduce prostate cancer risk
In countries where the soil is deficient in selenium (e.g. Australia), 100–200 μg of selenium daily is considered safe and appears to reduce the incidence of prostate cancer.25,26 Lycopene, found in the red part of tomatoes, and, in the new world, red wines, also seem to be a possible factor.27,28 Adequate vitamin D intake is to be encouraged, usually by natural means, but possibly by supplementation.29 Vitamin E supplementation may help some patients if the dose is limited to < 400 IU per day, although the SELECT trial has raised doubt about this.30 A dosage higher than this may increase the risk of heart attack or stroke.
Vasectomy and sexual activity do not appear to be major factors in the aetiology of prostate cancer.31,32
Herb and plant extracts have also been implicated in some studies, but there is currently no evidence for the use of saw palmetto, pygeum, pumpkin or stinging nettle, all of which have traditionally been used for benign prostatic hyperplasia. There is, however, some experimental evidence that isoflavones, such as red clover, which has a phyto-oestrogenic effect, as well as milk thistle, may have some benefit, but this has only been shown in experimental models and has been extrapolated from low-risk Asian populations.33,34
DIET SUPPLEMENTS AND PROSTATE CANCER
There is now considerable evidence that environmental factors, particularly dietary factors, may have a profound influence on the incidence of, and effect on, the natural history of prostate cancer.35–37 Current research into prostate cancer suggests that changes in so-called modifiable risk factors, such as diet and supplements, may translate into very meaningful benefits.38–43 The level of evidence for each component of the diet and supplement varies, and is still evolving. Having said that, many of the dietary modifications also have a general benefit.
DIET
The information on diet currently suggests that a healthy heart diet, or Mediterranean diet, appears to be beneficial to prostate cancer patients.44–46 Limited caloric intake, as well as reduction in saturated fats and a high intake of fish, appear to be beneficial.39 A diet high in cruciferous vegetables and plant-based foods appears to be beneficial not only to the heart, but also to the prostate.43,47
SUPPLEMENTS
The recently published large randomised control trial (SELECT) looking at the effects of selenium and vitamin E in prostate cancer concluded that there was no statistically significant benefit in the use of either selenium or vitamin E (alone or in combination) in the prevention of prostate cancer in relatively healthy men.18 Excessive use of multivitamins has recently been shown to increase the rate of advanced and fatal disease.48 Fish oil appears to be a good source of omega-3, particularly if fish is not a common part of one’s diet. Pomegranate has recently also shown some potential benefit.49–52
PHYTOMEDICINE
Herbs and spices, such as garlic, turmeric, rosemary and lemongrass, have been variously recommended, but most evidence for any general benefit appears to come from studies of garlic.53 For most of these, however, there is no reliable evidence in humans in vivo at normal intake levels.
There has also been evidence for polyphenols, such as green tea and red wine. Again, results have been mixed. A Chinese control study showed a protective effect of green tea with synergy for lycopene, but no benefit for green tea in a Japanese study.54,55 There appeared to be a combined inhibitory effect of green tea and COX-2 inhibitors.56,57 The benefit of red wine appears to come from the polyphenol resveratrol, and a moderate intake (< 4 glasses of red wine per week) appeared to have some benefit in the healthcare professional follow-up studies.58,59 Other plant extracts, such as soy and red clover, appeared to induce their effect through their oestrogenic content. These have been shown, in some population and experimental studies, to have a benefit, but not in vivo.60
LIFESTYLE FACTORS
Other aspects of supportive care include stress management and regular exercise and, certainly, there is now a lot of evidence to suggest that regular moderate exercise has benefits in many of the stages of prostate cancer and, in particular, in the more advanced stages, when patients are on hormone therapy.61,62 For example, elderly men with prostate cancer are about a third as likely to progress to more aggressive prostate cancer if they exercise regularly.63 It is, however, important to avoid certain dietary and supplementary treatments and, in particular, an excessive intake of calcium and zinc; and dietary fat, particularly saturated dietary fat, is to be avoided.46,64
The data on diet, as they relate to prostate cancer, are incomplete. As a general principle it is currently recommended that a healthy-heart diet, low in saturated fat and rich in omega-3 fatty acids, as well as judicious use of supplements, such as lycopene, selenium, vitamin D3, soy isoflavones, limited vitamin E and, possibly, pomegranate, are potentially useful.30,41,46,52,65 This should always be combined with appropriate stress management as well as regular exercise. The further benefit of this is that it empowers the patient to do something for himself.
Since the data from the outcome studies have been reported there has also been interesting data on the possible mechanisms underlying the positive outcomes. Healthy lifestyle change along the lines of the Ornish program have been found to improve telomerase activity66—an indicator of improved genetic repair—and also down-regulation of prostate cancer gene expression.67 These studies indicate a number of things:
The extensive discussion on lifestyle change and cancer using the ESSENCE model should also be reviewed in Chapter 24, Cancer.
SCREENING
WHY?
There is increasing evidence that prostate cancer testing and early aggressive treatment of appropriately selected cases is likely to save lives.68–70 This evidence includes the European randomised trial (described below), which reported in 2009.69 Prostate-specific antigen (PSA) testing has been responsible for the earlier detection of prostate cancer, which has led to the increased success of curative treatment. There is increasing evidence that use of PSA testing leads to the detection of cancers at an earlier and more curable stage, and that the falling death rate from prostate cancer can, at least in part, be attributed to the efforts of testing and early treatment. Also, in countries with a high uptake of PSA testing, there has been a consistently lower death rate from prostate cancer.
Recently, the European Randomised Study of Screening for Prostate Cancer published its results in the New England Journal of Medicine.69 This landmark study demonstrated unequivocally that PSA screening saves lives. This enormous undertaking was carried out in seven European countries and involved about 162,000 men aged between 55 and 69 years, who were screened with PSA testing every 4 years (with a cut-off value of 3 ng/mL, indicating the need for biopsy) versus no screening. It was scheduled to report in 2 years’ time, but was published early because a statistically significant reduction in the death rate from prostate cancer was found in the screened group. The median follow-up in this group was 9 years, with up to 14 years of follow-up.
Patients who underwent screening experienced a 71% increase in the incidence of prostate cancer detected compared with patients who did not undergo screening, and a 41% reduction in advanced disease; and a 20% reduction in deaths from prostate cancer was seen in all men at study entry. If only men who actually underwent screening were included in the results, the reduction in deaths from prostate cancer was 27%. It is highly likely that, as this study matures, the mortality benefit will increase further. This result is very similar to the 30% reduction in mortality in patients with breast cancer following screening with mammography71 and the 33% reduction in prostate-cancer-specific mortality that occurred in the United States from 1994 to 2003, following the introduction of PSA screening.72
The controversy about PSA testing is further compounded by another trial, published in the same edition of the New England Journal of Medicine.73 The conclusion of this US study, after 7–10 years of follow-up, was that the rate of death from prostate cancer was very low in both groups of screened and unscreened patients and did not differ significantly between the two study groups. This study has been criticised because not only did it have a poor method of testing, but 52% of the controls were screened, follow-up was too short, it was compared with a background of a heavily screened population and very few people underwent biopsies.73
PSA testing, therefore, is not a perfect science, for the following reasons:
Furthermore, there is evidence to suggest that use of the PSA test leads to detection of cancers at an earlier, and more curable, stage.74 This is supported by a falling death rate from prostate cancer which can, at least in part, be attributed to the efforts of testing and early treatment, particularly in areas that have been testing for more than 15 years in a high proportion of the community (e.g. in Tyrol, Austria).75,76 A 10-year study comparing surgery for early prostate cancer versus watchful waiting showed a clear benefit in terms of prostate cancer survival and the incidence of metastatic disease.77
Even less-aggressive tumours have been shown, after 15–20 years, to metastasise and lead to prostate cancer death.78
There is now increased effort to avoid treating latent tumours by putting the patient on active surveillance to avoid over-treatment, particularly in older patients.79–82 With improved clinical judgment, these less-threatening cancers are more likely to be identified at the time of diagnosis and less likely to be treated.
The side-effect profiles of treatments have decreased markedly in recent times.83,84
HOW?
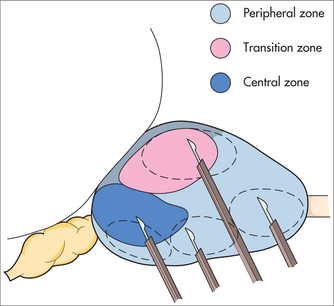
PSA testing and digital rectal examination currently form the cornerstone of prostate cancer testing. A raised PSA level can detect a non-palpable tumour, and an abnormal digital rectal examination can detect a non-PSA-producing tumour. Any older patient with haemospermia should also be tested for prostate cancer. Increasingly, PSA velocity is being used to detect cancer at an earlier stage by monitoring the PSA and recommending biopsy when the velocity increases (when the PSA goes up by > 0.75 ng/mL per year for two consecutive years).85,86 This is particularly useful in younger patients with a family history.
A biopsy should be performed if the digital rectal examination is abnormal or if the PSA reading is greater than the reference range for age on two consecutive occasions and there is no other explanation for the elevated PSA, such as severe prostatic enlargement, prostatitis, recent ejaculation or recent instrumentation. Biopsies should also be recommended if the PSA velocity starts to increase after a baseline of minimal PSA velocity.
WHEN?
Although advice varies in different countries and at different times,87 the current position of the Urological Society of Australasia is that individual men, aged between 50 and 70, with at least 10 years’ life expectancy, should be able to be screened by annual digital rectal examination and PSA testing, after appropriate counselling regarding the potential benefits of investigations and the controversy of treatment. The age at which screening commences should be reduced to 40 if there is a strong family history.69 The effectiveness of this screening in reducing mortality from prostate cancer is not entirely resolved.69
There is some evidence that an isolated PSA test at the age of 40 can predict the likelihood of a man developing prostate cancer in his lifetime.90 For example, a PSA level of > 0.6 ng/mL at 40 years of age suggests that the man is seven times more likely to develop prostate cancer than a man with a PSA level of < 0.3 ng/mL. This has useful implications for how frequently a PSA should be performed.
ACCURACY OF PSA SCREENING
Detection of prostate cancer in its curable stages therefore requires the use of relatively low PSA cut-off levels, which leads to unnecessary biopsies in approximately 70% of patients. This can be minimised by the use of age-specific reference ranges, free/total PSA ratio and PSA velocity and density.91 For example, if patients with a free/total PSA ratio of > 25% (for PSA range 4–10) are not biopsied, 8% of cancers will be missed but up to 30% of unnecessary biopsies will be avoided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree