Process of Normal Labor
Objectives
2. Explain labor, lightening, vaginal show, effacement, and cervical dilation.
3. Recognize spontaneous rupture of membranes.
4. Interpret the events that signal approaching labor.
5. List the four main variables in the birth process.
6. Describe the ability of the uterine muscles to contract and relax.
7. Differentiate three distinctive characteristics of labor contractions.
8. Differentiate between false and true labor.
9. Illustrate how frequency, duration, and intensity of contractions are monitored.
10. Describe fetal attitude, fetal lie, and fetal presentation.
12. Describe the term station as it relates to the maternal pelvis.
13. Distinguish six factors that influence the course of labor.
14. Interpret what is accomplished in each of the four stages of labor.
15. Summarize the response of each body system to the labor process.
Key Terms
acme (p. 96)
Braxton Hicks contractions (p. 98)
crowning (p. 95)
decrement (DĔK-rē-mĕnt, p. 96)
dilation (dī-LĀ-shŭn, p. 96)
duration of contraction (p. 98)
effacement (ĕ-FĀS-mĕnt, p. 96)
engagement (p. 95)
episiotomy (p. 102)
extension (p. 100)
external rotation (p. 100)
false labor (p. 99)
fetal attitude (p. 92)
fetal lie (p. 92)
fetal position (p. 93)
fetal presentation (p. 92)
floating (p. 95)
frequency of contraction (p. 96)
increment (ĬN-krĕ-mĕnt, p. 96)
intensity of contraction (p. 98)
internal rotation (p. 99)
labor (p. 91)
lightening (p. 98)
molding (p. 92)
show (p. 98)
station (p. 93)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
The time of labor and birth, though short compared with the length of pregnancy, is perhaps the most dramatic and significant period of pregnancy for the expectant mother, newborn, and family. The process of labor and birth is a fairly predictable sequence of events that usually occurs in a manner that results in a healthy mother and baby.
The Process of Labor
The process by which the fetus, placenta, and amniotic membranes are expelled from the uterus is called labor. What initially causes labor to begin is not known, but it is thought to be a cascade of events. Changes in maternal hormone levels; stretching of the uterus by the growing fetus; and an interaction between the placenta and the fetal pituitary, hypothalamus, and adrenal glands all contribute to the onset of labor. Although many people focus on the uterine contractions when they define labor, the process of labor is actually an interaction of four important variables, known as the “four Ps”: the Passageway, Passenger, Powers, and Psyche. These variables are discussed in this chapter. Other factors can influence the process of labor, including (Vande Vusse, 1999):
Major Variables in the Birth Process
The four factors most significant in the process of labor include (1) passageway or pelvis (its size and shape), (2) passenger (fetus) size and position, (3) powers (effectiveness of contractions), and (4) psyche (preparation and previous experience). An ideal labor is one in which the woman’s bony pelvis is adequate, the fetus is of average size, and the strength of the uterine contractions increases sufficiently to cause the cervix to fully efface and dilate. The woman’s psyche—her ability to relax and concentrate on muscle groups and to maintain a low level of anxiety—also plays a role in the normal progress of her labor.
Pelvis
The anatomy of the pelvis and uterus is discussed in Chapter 2. The angles of the birth canal are downward, forward, and upward, somewhat similar to the letter J. The pelvic curve must be negotiated by the fetus during the birth process. If the pelvic anteroposterior (AP) diameter is shortened by the sacral promontory or narrowed by the transverse diameter from the protrusion of the ischial spines or by the presence of a narrow pubic arch, the fetus will have difficulty coming through the birth canal. A clinical estimation of the pelvic measurements is an important part of prenatal care to determine adequacy for the birth process. An x-ray pelvimetry (measurement of the pelvis) is rarely performed. Other methods of estimating pelvic size such as a vaginal examination are discussed in Chapter 2 (Gabbe, Niebyl, & Simpson, 2007).
Passenger
The passenger includes the fetus along with the placenta, membranes, and amniotic fluid.
Fetal Head
The fetal head is engineered to withstand the pressure of uterine contractions and descent through the birth canal. Great pressure is exerted on the fetal head during labor, and even stronger pressure is applied to the head after the rupture of membranes because the amniotic fluid no longer serves as a cushion between the fetal head and the bony pelvis.
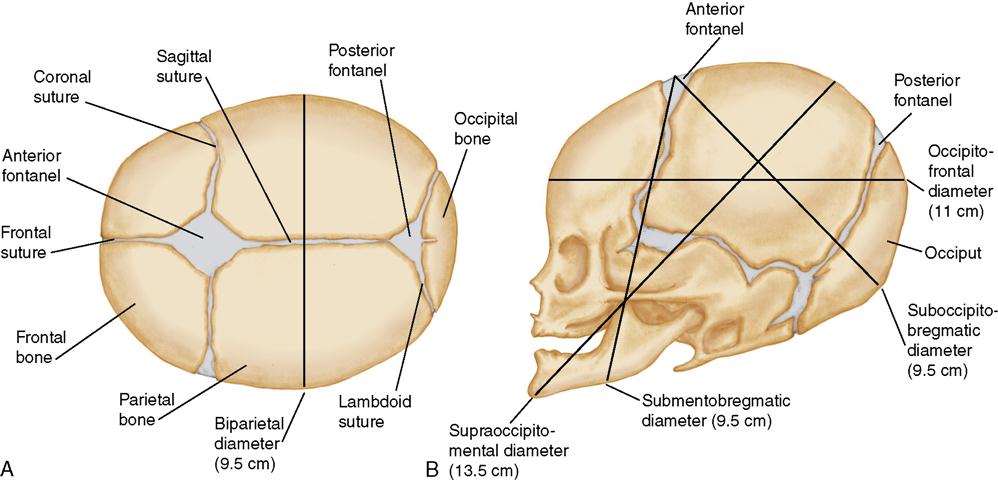
Bony Skull of the Fetal Head
The fetal head is composed of several bones separated by strong connective tissue, called sutures. A wider area, called a fontanelle, is formed where the sutures meet. The following two fontanelles are important in obstetrics:
The sutures and fontanelles of the fetal head allow it to change shape as it passes through the pelvis (molding). The fontanelles are important landmarks in determining how the fetus is oriented within the mother’s pelvis during birth.
The main transverse diameter of the fetal head is the biparietal diameter, which is measured between the points of the two parietal bones on each side of the head. The AP diameter of the fetal head can vary, depending on how much the head is flexed or extended (Figure 6-1).
Fetopelvic Relationship: Terminology
Some common terms are used in a special way to describe the fetopelvic relationship. It is important to know each term to understand the course of labor and birth.
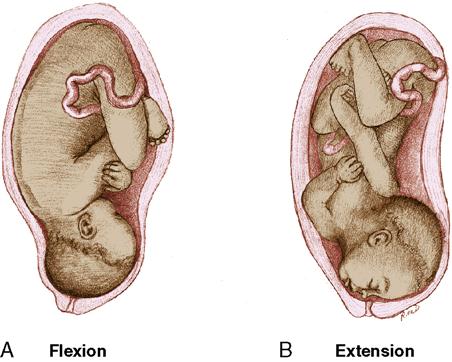
Fetal Attitude
Fetal attitude is the relation of the fetal parts to one another. The normal attitude of the fetus is one of flexion. The fetus is flexed with head on chest, arms and legs folded, and legs drawn up onto the abdomen. Changes in fetal attitude, particularly in the extension of the head, cause the fetus to present a larger diameter of the fetal head to the maternal pelvis. Extension of the fetal head, especially full extension in which the chin or face presents, makes vaginal birth difficult and sometimes impossible (Figure 6-2).
Fetal Lie
Fetal lie is the relation of the longitudinal axis of the fetus to the longitudinal axis of the mother. The ideal is a parallel relation in which the long axes of the fetus and mother are the same. In rare instances the fetus lies crosswise in the uterus (transverse lie), which necessitates a cesarean birth.
Fetal Presentation
Fetal presentation is determined by the body part of the fetus that is lowest in the mother’s pelvis (Figure 6-3). A cephalic, breech, or shoulder presentation may occur. Cephalic (head first) presentation is the most common, occurring in approximately 95% of all births, and labor most often proceeds normally. If the head is flexed, the position is referred to as a vertex presentation. Breech presentation occurs in approximately 3% of all births. In the breech presentation, the presenting parts may be either the buttocks (complete or frank breech) or one or both feet (footling breech) (see Chapter 14). The rarest type of presentation is the transverse (or oblique), which occurs in approximately 1% of births. These are referred to as malpresentations and do not proceed normally.
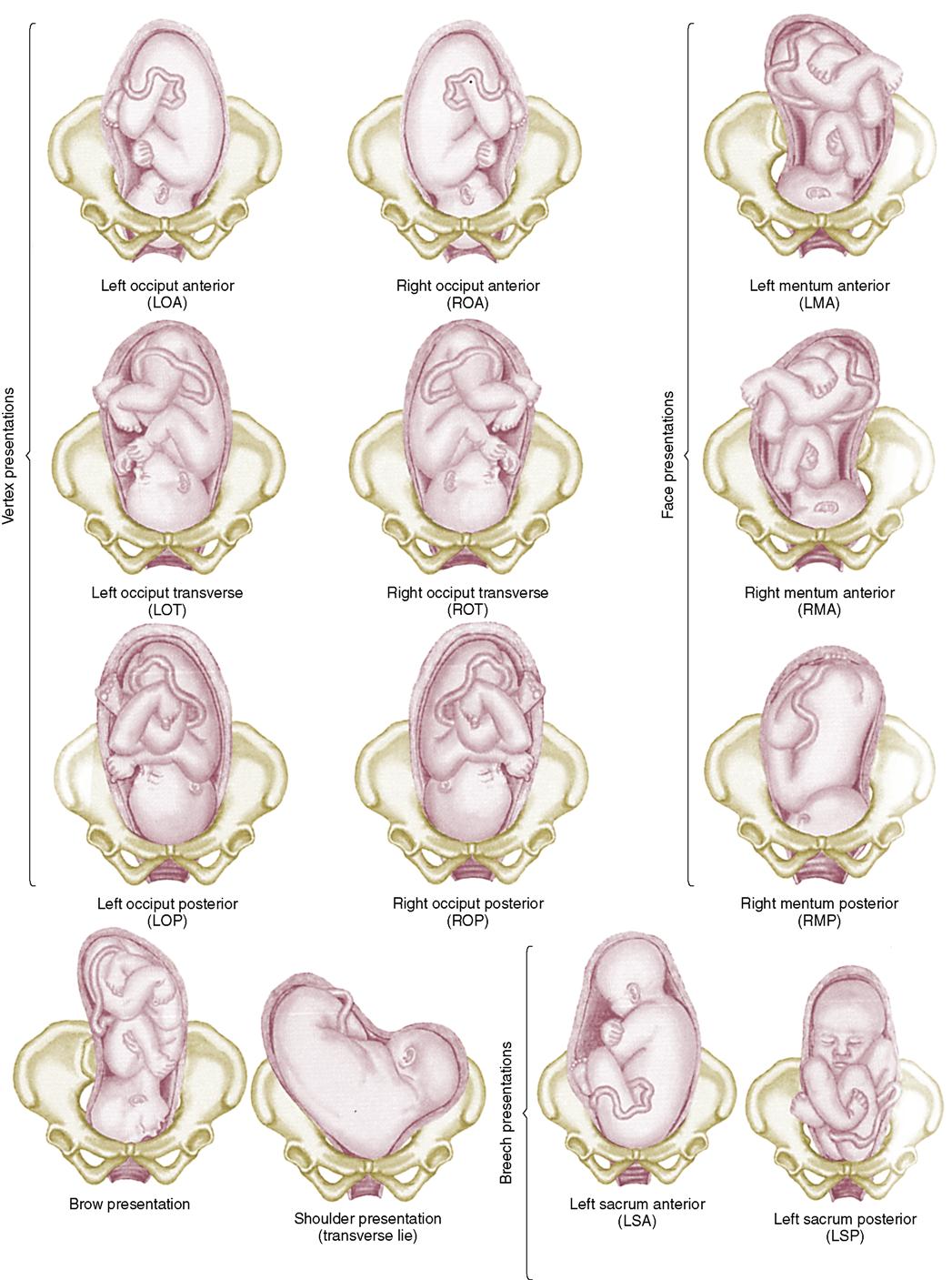
Fetal Position
Fetal position, a more specific indication of the fetopelvic relationship, is the relation of some designated point on the presenting part to the four quadrants of the maternal pelvis: anterior, posterior, left side, and right side. If the reference point is directed toward the transverse diameter of the maternal pelvis, it is referred to as a transverse position. The notations used to describe the fetal position are:
Anterior is recorded as A, posterior is recorded as P, and transverse is recorded as T. The abbreviations (notations) help the caregivers communicate the fetal position. If the back of the fetal head (occiput) is directed to the left of the woman’s body and anteriorly toward the pubis, it is described as LOA (left occiput anterior). When the occiput is directed to the left of the woman’s body and to the back toward the sacrum, it is LOP, and the labor is often longer with the woman experiencing more backache, which is often referred to as back labor. The left occiput anterior and right occiput anterior positions are the most common and facilitate a normal progression of labor. Abbreviations for fetal presentations are shown in Box 6-1.
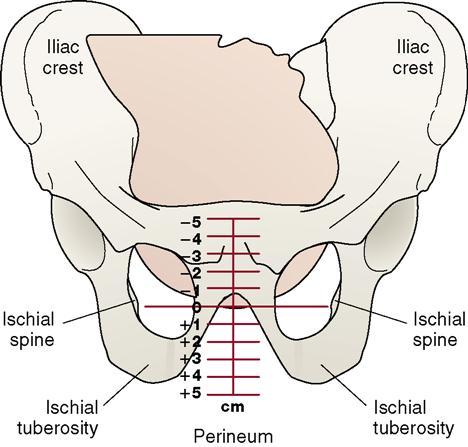
Station
Station is the relation of the presenting part of the fetus to an imaginary line drawn between the ischial spines of the maternal pelvis (Figure 6-4). To put it simply, the station is how far the fetal presenting part has descended into the mother’s pelvis. Station defines the progression of (usually) the fetal head down toward the pelvic floor. It is measured in centimeters above or below the ischial spines. When the presenting part is above the ischial spines, it is at minus station, with −5 at the inlet. When the presenting part is 1 or 2 cm below the spines, it is at the +1 or +2 station. Station +5 is at the outlet. When the presenting part is level with the spines, it is said to be at the 0 (zero) station, and the head is referred to as engaged. This progress is significant because when engagement occurs, the widest biparietal diameter of the baby’s head has entered the inlet (middle of pelvis). Before the head becomes engaged, it is said to be floating. When the station is +2 or +3, the mother’s perineum begins to bulge.
Crowning takes place when the fetal head is forced against the pelvic floor and can be seen at the vaginal opening during contractions. During labor, the presenting part moves from the negative into the positive stations. Failure of the presenting part to descend in the presence of strong contractions may be caused by a disproportion between the maternal pelvis and the fetal presenting part. The movement of the presenting part downward toward the outlet of the pelvis occurs in the ninth month and is known as lightening. Engagement takes place when lightening occurs.
Powers: Uterine Contractions
Understanding labor requires an understanding of the dramatic and unique physiology of the uterus. The uterine muscle (myometrium) is a smooth muscle that possesses the same properties as other smooth muscles in the body. Each muscle can contract and relax in a coordinated manner. Uterine contractions occur when uterine cells are stimulated to contract, and the stimulation spreads throughout the uterus. During labor, the contractions begin in the top of the uterus (fundus) and spread throughout the uterus in approximately 15 seconds. Because each contraction starts at the top, the nurse is able to ascertain the beginning of the contraction by placing her or his hands on the fundus.
A unique property of the uterine muscle is its ability to retain some of the shortening achieved during the contraction. This ability is called retraction or brachystasis. When the myometrium cells contract, the fibers of both the fundus and the body of the uterus shorten. When the contraction ends and the muscles relax, the fibers do not return to their original size but remain shorter than before the contraction. This continued shortening of the muscle fibers in the upper portion of the uterus results in a progressive decrease in the size of the uterine cavity and a thickening of the muscle tissue of the upper portion. These changes supply the force needed to advance the fetus. With less room at the top of the uterus, the fetus is forced to descend.
Uterine contractions are referred to as the source of power that brings about the birth of the fetus. Because these contractions cause discomfort, they are commonly called labor pains. The amount of discomfort produced by the contractions varies with the intensity of the contraction and the woman’s tolerance of discomfort (her psyche). During labor, the woman may first perceive the contractions as back discomfort. The discomfort then radiates to the front of the abdomen.
The Uterine (Labor) Contraction
Each contraction is followed by a period of relaxation, the interval between contractions. This period is significant to the mother and fetus. During the contraction, there is decreased blood flow through the uterine arteries and intervillous spaces. This decline in blood flow lowers the fetal heart rate. If the mother is being observed by electronic fetal monitor, the decrease in fetal heart rate during contractions is carefully assessed (see Chapter 7). If the contractions become more frequent and prolonged, the decrease in blood flow can be cumulative and compromise the fetus. In other words, the fetus receives a decreased oxygen supply and experiences stress during contractions. For this reason, it is important that the caregiver report to the physician if labor contractions are so close that there are no relaxation periods between them or if the intervals are progressively shortened, thereby causing significant patterns of fetal bradycardia.
Labor contractions are affected by maternal position. When a woman lies on her back, the contractions are likely to be more frequent but of lower intensity. When she lies on her side, the contractions are likely to be less frequent but of greater intensity. Therefore, a side-lying position improves the progress of labor and improves oxygenation to the fetus.
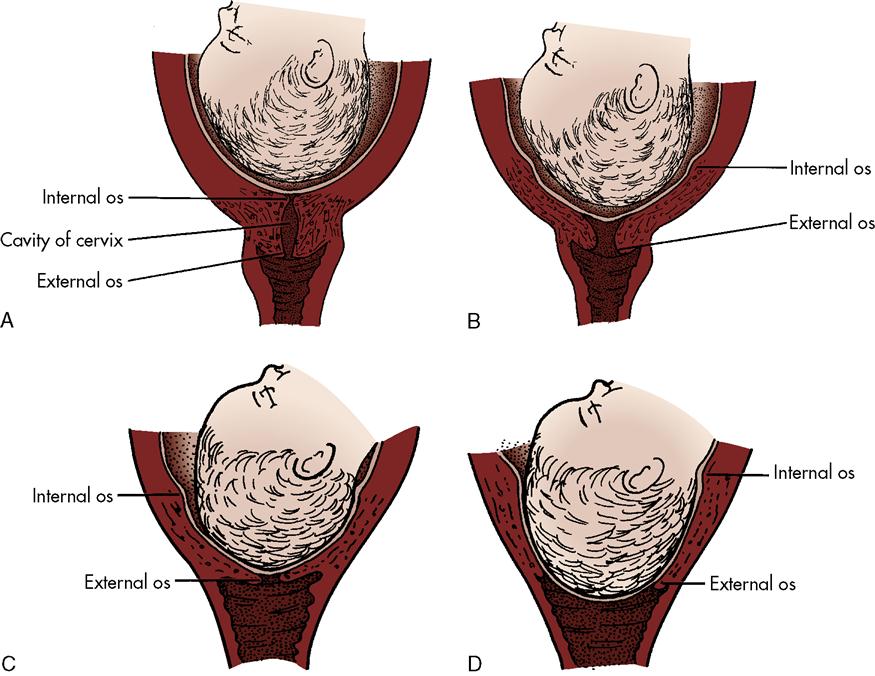
Effect of Contractions on the Cervix
Cervical changes include cervical effacement and dilation. Cervical effacement is the shortening and thinning of the cervix. Normally, the cervix is 2 cm (0.8 inches) in length. When effacement is complete (100%), the cervix has almost disappeared (Figure 6-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree