Urinary Diversion Stoma Care
Urinary diversions provide an alternative route for urine flow when a disorder, such as an invasive bladder tumor, impedes normal drainage. A permanent urinary diversion is indicated in any condition that requires a total cystectomy. In conditions requiring temporary urinary drainage or diversion, a suprapubic or urethral catheter is usually inserted to divert the flow of urine temporarily. The catheter remains in place until the incision heals.
Urinary diversions may also be indicated for patients with neurogenic bladder, congenital anomaly, traumatic injury to the lower urinary tract, or severe chronic urinary tract infection.
Ileal conduit and continent urinary diversion are the two types of permanent urinary diversions with stomas. (See Types of permanent urinary diversion, page 770.) These procedures usually require the patient to wear a urine-collection appliance and to care for the stoma created during surgery. Evaluation by a wound ostomy continence nurse will facilitate site selection and postoperative stoma care.
Equipment
Soap and warm water ▪ gloves ▪ waste receptacle (such as an impervious or wax-coated bag) ▪ linen-saver pad ▪ hypoallergenic paper tape ▪ antiseptic swab ▪ urine collection container ▪ rubber catheter (usually #14 or #16 French) ▪ stoma measuring guide ▪ scissors ▪ urine-collection appliance (with or without antireflux valve) ▪ graduated cylinder ▪ cottonless gauze pads (some rolled, some flat) ▪ washcloth ▪ skin barrier in liquid, paste, wafer, or sheet form ▪ stoma covering (nonadherent gauze pad or panty liner) ▪ two pairs of gloves ▪ Optional: liquid skin sealant, adhesive remover pads, irrigating syringe, tampon, hair dryer, hair clipper, regular gauze pads, vinegar, deodorant tablets.
Commercially packaged stoma care kits are available. In place of soap and water, you can use adhesive remover pads, if available.
Some appliances come with a semipermeable skin barrier (impermeable to liquid but permeable to vapor and oxygen, which is essential for maintaining skin integrity). Wafer-type barriers may offer more protection against irritation than adhesive appliances. For example, a carbon-zinc barrier is economical and easy to apply. Its puttylike consistency allows it to be rolled between the palms to form a “washer” that can encircle the base of the stoma. This barrier can withstand enzymes, acids, and other damaging discharge material. All semipermeable barriers are easily removed along with the adhesive, causing less damage to the skin.
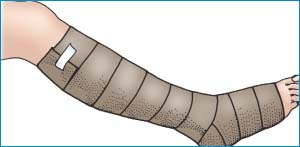
How to Wrap Unna’s Boot
After cleaning and drying the patient’s skin thoroughly, flex his knee. Then, starting with the foot positioned at a right angle to the leg, wrap the medicated gauze bandage firmly—not tightly—around the patient’s foot. Wrap the bandage twice around the patient’s toes without tension. Make sure the dressing covers the heel. Continue wrapping upward, overlapping the dressing 50% or more with each turn. Smooth the boot with your free hand as you go (as shown below).
 |
Stop wrapping about 1″ (2.5 cm) below the knee. If necessary, make a 2″ (5-cm) slit in the boot just below the knee to relieve constriction that may develop as the dressing hardens.
If drainage is excessive, you may wrap a roller gauze dressing over the Unna’s boot. As the final layer, wrap an elastic bandage in a figure-eight pattern.
 |
Preparation of Equipment
Gather all the equipment on the patient’s overbed table. Tape the waste receptacle to the table for ready access. Provide privacy for the patient, perform hand hygiene1,2,3 and follow standard precautions. Measure the diameter of the stoma with the measuring guide. Cut the opening of the appliance with the scissors—it shouldn’t be more than 1/8″ to 1/6″ (0.3 to 0.4 cm) larger than the diameter of the stoma. Moisten the faceplate of the appliance with a small amount of water or liquid skin sealant to prepare it
for adhesion. Performing these preliminary steps at the bedside allows you to demonstrate the procedure and show the patient that it isn’t difficult, which will help him relax.
for adhesion. Performing these preliminary steps at the bedside allows you to demonstrate the procedure and show the patient that it isn’t difficult, which will help him relax.
Types of Permanent Urinary Diversion
The steps involved in creating an ileal conduit or a continent urinary diversion are described below.
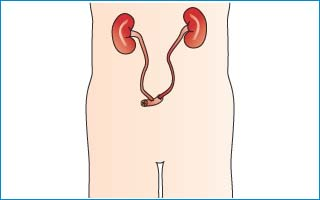
Ileal Conduit
A segment of the ileum is excised, and the two ends of the ileum that result from excision of the segment are sutured closed. Then the ureters are dissected from the bladder and anastomosed to the ileal segment. One end of the ileal segment is closed with sutures; the opposite end is brought through the abdominal wall, forming a stoma.
 |
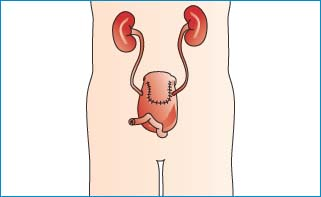
Continent Urinary Diversion (Indiana Pouch)
The surgeon introduces the ureters into a segment of ileum and cecum. Urine is drained periodically by inserting a catheter into the stoma.
Another type of continent urinary diversion (Kock pouch) is “hooked” back to the male urethra, making a stoma unnecessary.
 |
Implementation
Check the doctor’s order.
Gather the equipment.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.4
Explain the procedure to the patient as you go along, and offer constant reinforcement and reassurance to counteract negative reactions that may be elicited by stoma care.
Place the bed in low Fowler’s position so the patient’s abdomen is flat. This position eliminates skin folds that could cause the appliance to slip or irritate the skin and allows the patient to observe or participate.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
