Types of Shock
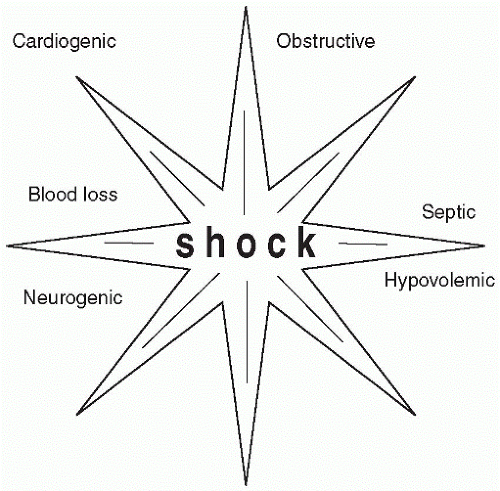
Shock is generally classified into three categories (Table 51-1). Cardiogenic shock is the inability of the heart to pump blood throughout the body. Circulatory shock is the loss of intravascular volume and has two subclassifications, hypovolemic and obstructive. The third main classification is distributive shock, which includes subclassifications of neurogenic, anaphylactic, and septic shock. Regardless of the type of shock, the stages the patient goes through remain the same. The compensatory mechanisms do not change because the outcome for all types, if uncorrected, is a decreased perfusion resulting in a lack of cellular oxygenation, multiple organ dysfunction, and death.
 Regardless of the type of shock, the stages the patient goes through remain the same. The compensatory mechanisms do not change because the outcome for all types, if uncorrected, is a decreased perfusion resulting in a lack of cellular oxygenation, multiple organ dysfunction, and death.
Regardless of the type of shock, the stages the patient goes through remain the same. The compensatory mechanisms do not change because the outcome for all types, if uncorrected, is a decreased perfusion resulting in a lack of cellular oxygenation, multiple organ dysfunction, and death.Table 51-1 Categories of Shock | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Cardiogenic Shock
Cardiogenic shock is most commonly caused by myocardial infarction. The development of shock depends on the amount of muscle wall damage that results from this insult. Other types of shock causing an inadequate circulation of blood may also lead to cardiogenic shock. When other types of shock are responsible, a myocardial depressant factor is released that causes a severe depression of the heart’s muscle ability to contract, resulting in a dilation of the left ventricle and leading to an inability for the heart to eject a sufficient amount of blood into the circulation.
 Cardiogenic shock is the inability of the heart to pump blood throughout the body and is most commonly caused by myocardial infarction.
Cardiogenic shock is the inability of the heart to pump blood throughout the body and is most commonly caused by myocardial infarction.Treatment
An intraaortic balloon pump is most likely needed to assist the heart in propelling blood through the aorta. Fluid volume walks a tight rope between too much and too little. Hemodynamic monitoring is essential to regulate the intravenous fluids given to the patient. Enough fluid must be administered to keep the preload (ventricular filling pressure) sufficient and yet not too much to overburden an already taxed system. Correction of dysrhythmias and the use of inotropic agents (e.g., dopamine) may be necessary for maintaining blood pressure; however, decreasing the workload of the heart by decreasing afterload (systemic vascular resistance) through vasodilators (e.g., nitroglycerin) is also important.
Circulatory Shock
A loss of circulating blood volume, whether actual or shifted among the fluid compartments, is the cause of circulatory shock. The result is a lack of cellular oxygenation and eventual tissue and organ failure. Two types of circulatory shock are hypovolemic shock and obstructive shock.
 A loss of circulating blood volume, whether actual or shifted among the fluid compartments, is the cause of circulatory shock.
A loss of circulating blood volume, whether actual or shifted among the fluid compartments, is the cause of circulatory shock.Hypovolemic Shock
Hypovolemic shock occurs when approximately 15-20% of the blood volume is lost. It may occur with trauma in which hemorrhaging and a loss of whole blood occurs, with burns and a loss of plasma, or with a loss of extracellular fluid such as with the gastrointestinal system fluid loss through excessive vomiting or diarrhea. Third spacing, the shifting of fluid from the vascular compartment to the interstitial or intracellular, or internal hemorrhaging also may cause hypovolemic shock.
 Hypovolemic shock occurs when approximately 15-20% of the blood volume is lost.
Hypovolemic shock occurs when approximately 15-20% of the blood volume is lost.Inadequate perfusion, the ultimate outcome of hypovolemic shock, starts with a decreased blood return to the heart and results in a decreased cardiac output and circulatory insufficiency. The compensatory mechanisms of sympathetic nervous system (SNS) stimulation, renin-angiotensin activation, and antidiuretic hormone stimulation attempt to maintain the blood pressure and cardiac output.
Treatment involves rapid fluid replacement. Surgical intervention may be needed if the insult is related to trauma. Success is achieved when blood pressure and cardiac output return to normal. A urine output of approximately 30 cc/hr indicates fluid balance has been achieved.
Obstructive Shock
Obstructive shock is related to some type of mechanical obstruction that interrupts blood flow through the circulation, heart, or lungs. Situations involving dissecting aortic aneurysm, cardiac tamponade, or pulmonary embolism are some of the more common factors causing obstructive shock. The
obstruction of blood flow causes the pressures of the right side of the heart to elevate and impairs the return of blood to the heart, resulting in jugular vein distention and an elevated central venous pressure.
obstruction of blood flow causes the pressures of the right side of the heart to elevate and impairs the return of blood to the heart, resulting in jugular vein distention and an elevated central venous pressure.
 Obstructive shock is related to some type of mechanical obstruction that interrupts blood flow through the circulation, heart, or lungs.
Obstructive shock is related to some type of mechanical obstruction that interrupts blood flow through the circulation, heart, or lungs.Treatment includes correcting the problem and returning blood flow to normal. Maintaining blood pressure and cardiac output during this type of shock is difficult because blood flow is obstructed. Thrombolytics may work with pulmonary embolism, although multiple contraindications such as age, cardiopulmonary resuscitation, and recent surgery may prevent use of this therapy. Surgical repair of an aneurysm or removing fluid from the pericardial sac with tamponade may help to alleviate the blockage.
Distributive Shock
Distributive shock occurs because of an increased vascular compartment related to loss of blood vessel tone. The blood volume then becomes redistributed, and a decreased volume is returned to the heart. This accounts for a decreased cardiac output and blood pressure. The important point to remember in distributive shock is that the blood volume is not diminished but redistributed. Three types of distributive shock exist: neurogenic shock, anaphylactic shock, and septic shock.
Neurogenic Shock
Neurogenic shock occurs secondary to a loss of vasomotor tone that brings about vasodilation. Neurogenic shock may be caused by brain or spinal cord injury from a diving accident or a bullet wound, lack of glucose to the brain, overdose of drugs, or anesthesia. In neurogenic shock the skin is warm and dry. Cervical spinal cord injuries, at or above the fifth thoracic vertebra, result in the loss of SNS vasoconstrictor tone, causing an uncompensated massive vasodilation. In addition, hypotension occurs because of an unopposed parasympathetic nervous system action, allowing for bradycardia, unlike other shock states where tachycardia is a compensatory mechanism. Often, the patient with spinal injury has hypothalamic dysfunction that causes a temperature dysfunction called
poikilothermia (temperature of the environment); when combined with the vasodilation, the patient’s temperature becomes even cooler.
poikilothermia (temperature of the environment); when combined with the vasodilation, the patient’s temperature becomes even cooler.
 Neurogenic shock occurs secondary to a loss of vasomotor tone that brings about vasodilation.
Neurogenic shock occurs secondary to a loss of vasomotor tone that brings about vasodilation.Neurogenic shock is rare, and if the cause is known the condition may be corrected; for example, neurogenic shock related to anesthesia can be reversed. Temporary administration of vasoconstrictors such as dopamine may be indicated. An insulin reaction causing decreased glucose availability for the brain can also be easily reversed through administration of glucose. Spinal cord injury is permanent, and treatment of the shock state is comprehensive. Neurogenic shock related to spinal cord injury can develop immediately after the injury and last for days to weeks. Treatment involves fluid resuscitation and vasopressors such as dopamine to maintain cardiac output and tissue perfusion, phenylephrine or norepinephrine to increase the systemic vascular resistance, and management of the hypothermia with heating blankets.
 The body responds to most shock states through vasoconstriction to help pull blood volume to the vital organs, thus leaving the skin cool and clammy. In neurogenic shock, secondary to spinal injuries at or above the fifth thoracic vertebra, the skin is warm and dry due to the loss of SNS, resulting in massive vasodilation.
The body responds to most shock states through vasoconstriction to help pull blood volume to the vital organs, thus leaving the skin cool and clammy. In neurogenic shock, secondary to spinal injuries at or above the fifth thoracic vertebra, the skin is warm and dry due to the loss of SNS, resulting in massive vasodilation.Anaphylactic Shock
Anaphylactic shock occurs when vasodilators such as histamine are released into the circulation as a result of an allergic reaction to drugs, foods, insect stings, or antitoxins. The release of vasoactive mediators causes the vasodilation of arterioles and venules and makes the capillary wall permeable, which results in the leaking of fluid from the vascular to the interstitial space.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access