Treating Elevated Mood Without Medication
Treating elevated mood and upside symptomatology with medication is commonplace and is expected in most treatment settings. However, this does not negate the therapeutic advantages of a psychotherapeutic approach. Many mental health practitioners have not learned this, having been given the overt or covert message that therapy for patients with grandiose or elevated symptoms was either not possible or at best, minimally helpful. As with so many issues involving elevated mood mentioned previously, this message was based on full-blown manic symptoms in elevated mood. Manic patients, whether psychotic or not, are minimally accessible to verbal interventions. The practitioner rapidly recognizes that such patients cannot or will not attend
to instructions, education, limit setting, or interpretation. Although one needs to be mindful of the pitfalls listed in Chapter 5, specifically targeted verbal interventions can greatly help hypomanic patients (1). Psychotherapeutic interventions, either alone or in combination with medication, are useful in both the short and long terms and can be accomplished for individual patients or in a group setting.
to instructions, education, limit setting, or interpretation. Although one needs to be mindful of the pitfalls listed in Chapter 5, specifically targeted verbal interventions can greatly help hypomanic patients (1). Psychotherapeutic interventions, either alone or in combination with medication, are useful in both the short and long terms and can be accomplished for individual patients or in a group setting.
An additional consideration is that direct treatment of elevated mood may also, in the long run, protect against the emergence of depressive episodes. Therefore, modalities that treat elevated mood may indirectly decrease the emergence of depressed symptoms. Hypomanic and manic patients are frequently overactive and attempt to function on little or no sleep. This combination of excessive activity and little restorative rest can lead to periods of physical exhaustion that may also predispose the patient to slipping or “crashing” into depression. Therefore both medication and nonmedication treatments of hypomania listed in this chapter and the next should be vigorously advocated by the clinician.
This chapter is divided into two sections. The first covers various schools of psychotherapy applied in treating elevated mood and a brief review of the literature supporting their effectiveness. This is followed by sections devoted to specific elements of hypomania education and other psychotherapeutic techniques that can be employed by virtually any practitioner regardless of his/her therapeutic orientation.
Schools of psychotherapy effective in elevated mood states
There are five forms of research-based psychotherapy found useful in conditions, which include elevated mood. These are listed in Table 6.1.
Each of these techniques is somewhat different than traditional psychoanalytic methodology but each focuses on a constellation of treatment elements, which is shown in Table 6.2. As with most of the research on elevated mood disorders, subjects included a mixture of patients with a diagnosis of both
bipolar I and bipolar II disorders. There is virtually no specific research on psychotherapy in hypomania alone. It is therefore by extrapolation and clinical experience that we assume this research demonstrates that these modalities would be helpful in treating hypomania as well.
bipolar I and bipolar II disorders. There is virtually no specific research on psychotherapy in hypomania alone. It is therefore by extrapolation and clinical experience that we assume this research demonstrates that these modalities would be helpful in treating hypomania as well.
TABLE 6.1 Forms of psychotherapy useful in treating hypomania | |||||
|---|---|---|---|---|---|
|
TABLE 6.2 Common elements of psychotherapeutic techniques used in elevated mood | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Cognitive behavioral therapy (CBT) is a well-known and effective treatment for depression. There is also some evidence (3,4,5) of its usefulness in bipolar disorder. This evidence focuses particularly on early detection and intervention, medication adherence, stress management, and treatment of comorbid conditions and bipolar depression (6). As with all psychotherapeutic techniques mentioned in this section, CBT has the advantage of not inducing or precipitating mania and has essentially no side effects (7).
A study that specifically looked at the use of CBT in bipolar disorder and focused on the amount of long-term change was conducted by Ball et al. (8). In this study, 52 patients with bipolar I or bipolar II disorder were randomly allocated to a 6-month trial of CBT or treatment as usual. Both treatment groups were also receiving mood stabilizers. At post-treatment analysis, patients allocated to CBT had less severe Beck Depression and Montgomery-Asberg Depression scores and lower Young Mania Rating Scales scores when compared with controls. The differences were less strong with time but did persist for the succeeding 12 months.
Psychoeducation is useful in a wide variety of psychiatric conditions, including virtually all mood disorders. Although not often studied directly, Colom et al. researched a group of mixed bipolar I and bipolar II patients, adding 21 sessions of structured psychoeducation about bipolar disorder to their management. This was provided in a small group setting of approximately 10 patients, and then compared to a control group of unstructured meetings with the same therapists, which included minimal teaching about bipolar disorder. When compared to controls over a 2-year period, those patients given psychoeducation had a 67% decrease in psychiatric hospitalization (9).
Family-focused therapy. Miklowitz et al. applied a family management strategy in treating patients with bipolar I and bipolar II disorders that had been previously successful in the treatment of schizophrenics (10). In addition
to psychoeducation, patients and their families also learned communication techniques in anticipation of relapse. Therapists helped patients and their families develop a plan of action and communication techniques if symptoms of relapse occurred. Using 21 therapy sessions over 9 months, there was a significant reduction of relapse rate in patients who had been previously hospitalized for mania.
to psychoeducation, patients and their families also learned communication techniques in anticipation of relapse. Therapists helped patients and their families develop a plan of action and communication techniques if symptoms of relapse occurred. Using 21 therapy sessions over 9 months, there was a significant reduction of relapse rate in patients who had been previously hospitalized for mania.
Interpersonal and social rhythm therapy (IPSRT) was developed specifically for bipolar disorder. It had been noted that disruption of sleep and circadian rhythms often exacerbated or instigated affective symptoms. Using interpersonal principles, Frank et al. taught patients self-monitoring techniques as well as regular routines for daily activities, such as sleeping and eating. When used in conjunction with medication, this form of therapy was shown to increase lifestyle regularity and decrease manic episodes (6). When IPSRT was withdrawn, higher relapse rates occurred (10,11). IPSRT could not, however, be correlated with faster recovery from mania (12)
Prodrome detection is a strategy in which a therapist meets with an individual patient and discusses the signs and symptoms of manic and depressive relapse for this specific patient. In concert with the therapist, the patient rehearses a plan of action should relapse occur. Perry, et al. (13) devised an individualized plan written on a laminated card, which was to be carried by the patient. A symptom diary kept on a daily or weekly basis helped the patient to monitor symptoms. Studying a group of primarily bipolar I patients, those using prodrome detection treatment suffered a 20% relapse rate after 1 year, whereas the control group not using prodrome detection suffered a 50% relapse rate.
Other useful psychotherapeutic strategies
Although not associated with any one school of thought or treatment, the strategies and approaches outlined throughout the rest of this chapter can be utilized by any therapist, regardless of training. Some of these incorporate the same essential elements listed in Table 6.1.
Analogies
Analogies, especially ones using non-mental health subject matter that are easily recognizable by the patient, can be helpful in explaining diagnostic concepts, treatment goals, and the expectations of response. For the hypomanic patient with bipolar or cyclothymic disorder, analogizing their condition to sitting on a raft in the middle of an ocean storm is particularly illustrative.
THE OCEAN STORM
Your life has been a marked series of ups and downs as if you were sitting on a raft in the middle of an ocean gale. When the wind whips up, you are tossed from the peak of high waves to their trough. The strength of the weather, the length of the storm, and the turbulence of the waves can feel quite unpredictable. Although the ride may be exhilarating at times, it can
also be very frightening. At times, it may feel as if the raft will capsize, and you are hanging on for your very life. While at the bottom of the trough a large wave may splash over you and engulf the raft to the point that you may feel suffocated or as if you are going to drown. As terrifying as this situation may feel, without warning you may be taken back up to the peak of a wave and feel as if you are again riding the crest, on top of the wave, only to crash again.
also be very frightening. At times, it may feel as if the raft will capsize, and you are hanging on for your very life. While at the bottom of the trough a large wave may splash over you and engulf the raft to the point that you may feel suffocated or as if you are going to drown. As terrifying as this situation may feel, without warning you may be taken back up to the peak of a wave and feel as if you are again riding the crest, on top of the wave, only to crash again.
Our treatment will attempt to smooth out the waves to a gentle swell, such that you will remain comfortable sitting on the raft without fear of being tossed overboard or drowning. By working together, we will minimize the likelihood that you will be unpredictably taken to heights, which you cannot control, only to fall again. As you adjust to calmer seas, you will be better able to clearly view your surroundings and assess what course of action and direction you wish to take. Do you wish to paddle toward a ship in the distance? Paddle to a nearby island? Or rest comfortably in the sun? In any case, it will feel much more under your control. No one’s life is ever a totally calm sea; however, an increased sense of control will feel empowering.
Another analogy, which can be useful when using mood stabilizers and antidepressant medication as well as explaining the risks of administering antidepressants alone, is that of a seesaw or a teeter-totter.
THE TEETER-TOTTER
Using medication in elevated mood or mood swings is like balancing a teeter-totter. When in a depression, the left end of the seesaw is down. When in the midst of unstable mood episodes, the teeter-totter often moves up and down with seeming unpredictability. When the seesaw is in the down position and an antidepressant alone is added, the lower end may rise. It may help transiently, making you feel better but often this positive effect is unpredictable. Either the seesaw falls again (you revert to the depressed state), balances briefly (your mood is transiently even) or can zoom up off the ground in the high position (spiral into a hypomania or mania). In this latter state, you may feel elated for a period of time, but this is not likely to last, as you crash to the ground again. At other times, the frequency of the oscillations increases. Therefore we use medications to stabilize mood and keep the seesaw level. When mood stabilizers alone are insufficient to eliminate or reduce depressed periods, a specific mood elevating medication may also be carefully added.
“Re-viewing” history
Many patients with elevated mood have lived with their condition for years, even a lifetime, without a diagnosis. Some may have the sense that they have a condition, which could never be positively affected by treatment. When periods of depression and low functioning are intermingled with periods of hypomania, patients (and those around them) may develop inaccurate explanations for their erratic behavior and lack of consistency. Impulsive business
and social decisions, overspending, and other money mismanagement and poor judgment may be attributed to lack of discipline, personality weakness, or simply “not caring.” These evaluations may be made by the patient himself or by the patient’s family, and invariably lead to decreased self-esteem and negative assessments by others.
and social decisions, overspending, and other money mismanagement and poor judgment may be attributed to lack of discipline, personality weakness, or simply “not caring.” These evaluations may be made by the patient himself or by the patient’s family, and invariably lead to decreased self-esteem and negative assessments by others.
When the diagnosis of hypomania or cycling is made and mood is sufficiently stable, it can be extraordinarily helpful to “re-view,” that is, view the patient’s history again in light of the new diagnosis. In doing so, it may be clearer to patients that some of their erratic and excessive behaviors—personally, financially, sexually, or otherwise—are symptoms of their illness. It can be quite relieving to understand that such behavior does not automatically mean the patient is a “bad person” or has a fundamentally flawed personality. They have had the behavioral symptoms of an illness that can be treated. This is not to say that all negative behaviors can be ascribed to hypomania or illness. On a person-by-person basis, it is necessary to sort out what may be illness-related behavior and what may be referable to other personality characteristics and/or other causes. It may be similarly helpful to invite the spouse, children, parents, or other family members for a session and explain directly the relationship between hypomania and problematic behaviors. A meeting such as this may provide a useful context for the patient’s family to understand their loved one and assess these problematic activities in a less negative way.
“Re-viewing” family history
It is not uncommon when identifying a patient’s cycling mood disorder to find other close biologic relatives who have been similarly diagnosed or have a presumptive diagnosis based on their behavior. Therefore, a similar analysis of the patient’s close blood relatives may be useful in helping the patient understand negative behaviors as part of an illness instead of viewing the relatives as being “mean”, “weird” or “thoughtless”. It would be an advantage to evaluate a patient’s relative in person to establish a cycling mood diagnosis. Even when this is not possible however, patterns of family behavior may be sufficiently classic or similar to the patient’s own behavior to classify them as symptomatic of manic/hypomanic episodes. Excessive anger and irritability, sexual acting out, poor financial decisions, or inability to hold a job in the context of major mood swings may be interpreted for the patient as relating to that relative’s own cycling mood episodes. Even abusive behavior may be partially “re-viewed” and reinterpreted in light of an absence of anger control that can often occur in the context of hypomania or mania. Although not removing the necessity of psychotherapy for the patient, it may be quite helpful to understand that an abusive parent, for example, was ill and not just “mean.”
“Re-viewing” from a new perspective
A third way of “re-viewing” is to help the patient see his/her own mood state and actions from “the outside” rather than from his own internal perspective.
Patients may see the world solely from their own perspective, unable to absorb feedback from others and act “with blinders on.” Helping patients to get a more balanced view of themselves can be helpful in changing this view and modulating behavior. When hypomanic, patients with elevated mood often believe that their ideas are “meant to be,” “perfect,” “sharply focused,” or ideal. Although valid at times, the more hypomanic an individual becomes, the higher the likelihood that such notions are unique to the hypomanic person but viewed differently by others. When re-viewed later, behaviors or ideas that “seemed right at the time” are often viewed as overly impulsive, or frankly impossible.
Patients may see the world solely from their own perspective, unable to absorb feedback from others and act “with blinders on.” Helping patients to get a more balanced view of themselves can be helpful in changing this view and modulating behavior. When hypomanic, patients with elevated mood often believe that their ideas are “meant to be,” “perfect,” “sharply focused,” or ideal. Although valid at times, the more hypomanic an individual becomes, the higher the likelihood that such notions are unique to the hypomanic person but viewed differently by others. When re-viewed later, behaviors or ideas that “seemed right at the time” are often viewed as overly impulsive, or frankly impossible.
Although it would be optimal if such perspective could be achieved when the patient is most hypomanic and therefore most at risk, this may be difficult. Obtaining a more accurate perspective may only occur after the lowering of mood with medication. One psychotherapeutic technique useful in obtaining perspective is drawn from the field of psychodrama. A “two-chair technique” involves having the patient sit in a second chair, not the usual chair where the patient sits. The patient and the therapist together then view the patient’s behavior as if he or she was a third person in the room sitting in the empty chair. Comments and dialogue are conducted in the third person; for example, “How would you characterize his (patient’s name) behavior?” “What risks is Jill taking?” “Let’s compare the benefits of how Frank is acting with the risks he is taking.” “What would Jennifer’s husband think of what she’s doing?” “How would you advise Matthew if you were his best friend?” “Let’s assume that you were Anna’s supervisor. What if any corrective action is necessary and how would you tell that to her?”
After such a series of questions, the patient then reverts to his usual chair and the therapist and the patient discuss possible changes in perspective as a result of this exercise. With new insights, a specific behavioral plan can be put in place with a higher potential for success.
Mood recognition and charting
One might assume from all that has been written about elevated and depressed mood in this book that patients are acutely aware of their mood state. This is hardly the case. Some individuals may be aware of their behavior, energy level, and mood, whereas many are oblivious to these parameters. Although unrecognized mood/behavior states are more prevalent at the elevated end of the spectrum, they can also apply to depression, particularly dysthymia. During a hypomanic episode, patients often do not recognize marked changes in activities, moods, and routines that are readily apparent to others. One goal of therapy is to help individuals recognize specific mood-related behavioral cues, especially those that serve as “red flag” warnings of incipient mania or depression. A particularly effective technique in this recognition is the use of graphic charting.
Lifetime mood charting in patients with a cycling disorder is extremely useful. These charts can be self-completed or constructed during a therapy session by therapist and patient together. Such charts depict a long-term
picture of the patient’s mood history, focusing on significant mood episodes, whether depressed or elevated. Periods of psychiatric treatment or hospitalizations are noted. In addition to significant dysfunctional moods, it is useful to indicate milder deviations including periods of euthymia, temperamental hyperthymia, dysthymia, or subsyndromal traits. This graphic information is helpful in diagnosis and treatment planning, especially in determining a medication regimen (see Chapter 7). Lifetime charting can illustrate long patterns of mood swings and, therefore, is useful in the “re-viewing” of the patient’s life as noted earlier in this chapter.
picture of the patient’s mood history, focusing on significant mood episodes, whether depressed or elevated. Periods of psychiatric treatment or hospitalizations are noted. In addition to significant dysfunctional moods, it is useful to indicate milder deviations including periods of euthymia, temperamental hyperthymia, dysthymia, or subsyndromal traits. This graphic information is helpful in diagnosis and treatment planning, especially in determining a medication regimen (see Chapter 7). Lifetime charting can illustrate long patterns of mood swings and, therefore, is useful in the “re-viewing” of the patient’s life as noted earlier in this chapter.
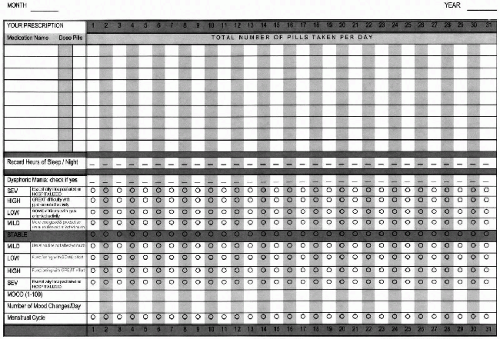
Shorter-term graphic charts, completed by the patient between therapy and medication management appointments, can be organized by the day, week, or month. Although many formats have been used for graphic charting, the most typical chart will be completed for a 1-month period during which the patient rates his mood on both a graphic and numeric scale, the number of hours of sleep, and the presence of any life events which might affect mood (see Figure 6.1). Women will include menstrual cycle data and observe for any correlation with mood changes. All medications taken are noted down, along with dosage and any side effects. Charts may be customized to track other target symptoms including irritability, binge/purge episodes, anxiety and panic attacks, headaches, or other specific physical pain. These too are rated on a numeric scale.
Yearly charting is helpful in highlighting any seasonal changes in elevated or depressed mood. Even with significant mood stabilization, when followed over time, seasonal changes may clearly emerge. A very common seasonal pattern is a progressive elevation of mood in the spring, reaching an apex in the summer, and then falling in autumn to a depression in winter. Other seasonally related patterns show depressions regularly appearing in the summer or mood elevations each spring and fall.
Most patients find the opportunity to self-chart as a way of becoming actively involved in their own care. Charting can be an especially helpful graphic tool for patients who are not particularly sensitive to their mood and activity changes. Additionally, medication management and compliance can be enhanced by these graphic and objective reports of changes in the patient’s mood state and activity.
Occasionally, there may be resistance to mood charting. Patients may worry that they do not know what constitutes “normal” and are concerned that they will give a false impression of their condition. Reinforcing that learning and recognizing one’s moods is a gradually learned skill, and the fact that there is no “right or wrong” to charting can be reassuring. Other patients, especially those newly diagnosed, may decide that attempting to recognize, analyze, and rate their feelings is a waste of time. Such patients would not complete their charts or would have “forgotten” to bring them. Gentle persuasion and the therapist’s skill in utilizing these charts will help most patients to eventually comply.
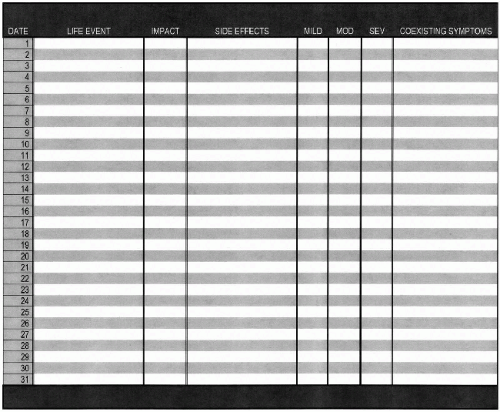 Figure 6.1 (continued)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|