The Thyroid Gland
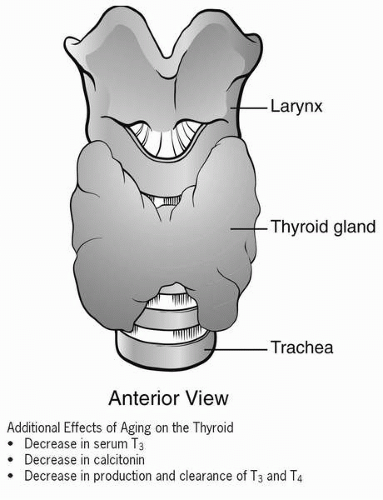
The thyroid gland, located anteriorly to the trachea at the lower part of the neck, is a highly vascular gland responsible for regulation of many physiological functions of the body. Any imbalance in the hormones produced by this gland can cause multiple system dysfunction. These imbalances can easily be corrected through the use of medications or surgery.
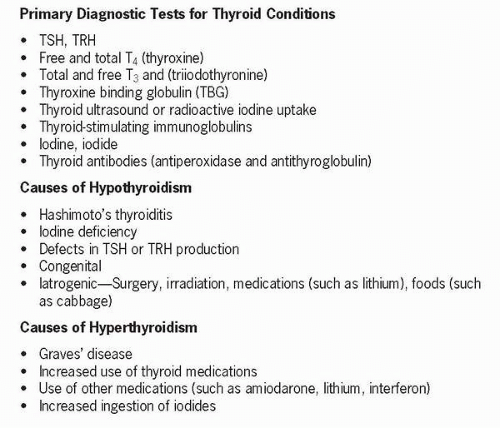
The thyroid gland is located in the anterior aspect of the neck just below the larynx and contains follicular and nonfollicular cells. The thyroid gland produces thyroxine (T4) and triiodothyronine (T3), which control metabolism, and calcitonin, which lowers serum calcium levels by opposing bone resorption (inhibition of osteoclastic activity) and promotes formation of osteoblasts. The follicular cells synthesize and secrete some of the thyroid hormones, and the nonfollicular cells (C cells) secrete various polypeptides including calcitonin, which is also called thyrocalcitonin. The follicular cells also contain a gelatinous substance called thyroglobulin. If iodine, which is necessary for the formation of T4 and T3, is deficient, inadequate amounts of T4 and T3 are produced. If the thyroid does not produce enough hormones to inhibit thyroid-stimulating hormone (TSH), the thyroid produces additional thyroglobulin, which is not affected by iodine, in an effort to increase circulating levels of thyroid hormone. This results in hypertrophy of the thyroid gland known as goiter. An enlarged thyroid gland can occur with either hypothyroidism or hyperthyroidism, although it is not necessarily indicative of thyroid dysfunction. If the thyroid is enlarged but not associated with identifiable clinical manifestations, it is referred to as a nontoxic goiter. Thyroid nodules may be malignant and are usually solitary nodules that are less than 1 cm or may be benign with multiple nodularities (multinodular goiter). Nodules may also be due to inflammation, as seen with Hashimoto thyroiditis, or may be cystic in nature. Nodules may be palpable or discovered on ultrasound.
Table 20-1 Manifestations of Thyroid Disease | ||||
|---|---|---|---|---|
|
TSH is synthesized and stored in the anterior pituitary. Once released, it binds to receptors located on cell membranes of the thyroid gland. This causes a release of stored thyroid hormones, increases iodine uptake and oxidation, increases thyroid hormone syntheses, and increases the synthesis and secretion of prostaglandins by the thyroid. Thyroid hormone is regulated through a negative feedback loop involving the hypothalamus, anterior pituitary, and thyroid gland. TRH is synthesized and stored in the hypothalamus. It is released and travels to the anterior pituitary through vascular channels where it stimulates the release of TSH. Thyroid hormones thus produced have a negative feedback effect and inhibit thyrotropin-releasing hormone (TRH) and TSH, which in turn decreases thyroid hormone synthesis and secretion. Normally, the thyroid gland produces 90% of T4 and 10% of T3. T4 is converted to T3 in body tissues. Of all the thyroid hormones, T3 has the greatest metabolic effect. Ninety percent of these hormones are bound to protein for transport to body tissue. T4 and T3 have a diurnal variation that peaks in the late evening. Their secretion is influenced by
gender, pregnancy, nutrition, and levels of selected hormones or chemicals. TRH is increased with exposure to cold, stress, and decreased levels of T4. T3 may be elevated in those taking oral contraceptives or who are pregnant.
gender, pregnancy, nutrition, and levels of selected hormones or chemicals. TRH is increased with exposure to cold, stress, and decreased levels of T4. T3 may be elevated in those taking oral contraceptives or who are pregnant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree