Thalassemia, Sickle Cell Anemia, and Pernicious Anemia
Each of these anemias is due to some type of genetic disorder affecting the production of red blood cells (RBCs). Thalassemias may be of the α or β or major or minor types. Thalassemia comes from the Greek word thalassa meaning “sea” and Haima meaning “blood” because of the prevalence of this disorder in people of Greek and Italian descent (Mediterranean area).
Sickle cell anemias are found in 1 in 400 African-Americans, with 8% having the sickle cell trait. Both have asymptomatic carrier states and active states that can be fatal. Pernicious anemia is actually an autoimmune disorder found in adults over 60 with a strong familial tendency for developing it.
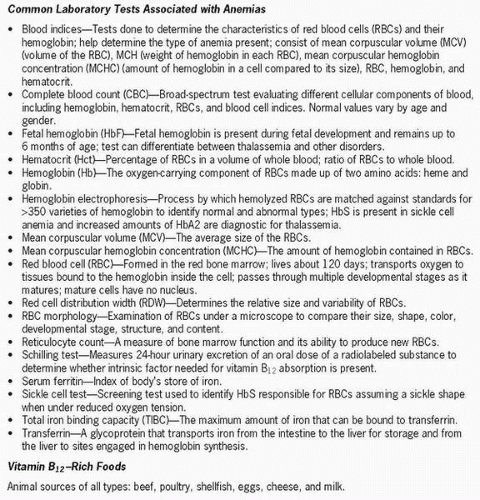 Figure 12-1 Common laboratory tests associated with anemias. |
Pathophysiology
Thalassemia is a hereditary disorder leading to anemia because of defective hemoglobin synthesis. α Thalassemia is more common in southeast Asia and China, whereas β thalassemia is more common in the Mediterranean area (Italy and Greece) and is also seen in people of Chinese, Asian, or black heritage. Hemoglobin A is normally synthesized by a combination of two α chains located on chromosome 16 and two β chains found on chromosome 11. α Thalassemias are due to a genetic defect that causes the α chains to be too short. β Thalassemias are due to a mutation of chromosome 11, resulting in reduced or absent β chain synthesis. An individual heterozygous for the thalassemia gene has a condition called thalassemia minor, which produces a mild, chronic, hemolytic anemia with microcytic and hypochromic RBCs. A person with thalassemia minor tends to produce extra RBCs to compensate for the anemia.
If two people, each having thalassemia minor, pass the defective gene on to their offspring, the child will have thalassemia major (Cooley’s anemia). In β thalassemia, excess α chains are produced, but these chains tend to become attached to the RBC membrane, damaging them and forming toxic substances. Some chromosome 11 mutations result in no β chain formation, while other mutations allow for a limited number of β chain formations. Approximately 5% of children with thalassemia major continue to produce fetal hemoglobin, and when given the drug hydroxyurea the amount of fetal hemoglobin produced is increased. Children born with this disorder are usually normal at birth but develop a severe anemia after 6 months of age when hemoglobin F synthesis declines and hemoglobin A synthesis increases. They then require blood transfusions. They experience growth failure, developmental problems,
hepatosplenomegaly, jaundice, and bony deformities. The numerous transfusions produce an overload of iron, which causes heart failure, cirrhosis, and endocrinopathies that, in turn, cause the child’s death by age 20 to 30.
hepatosplenomegaly, jaundice, and bony deformities. The numerous transfusions produce an overload of iron, which causes heart failure, cirrhosis, and endocrinopathies that, in turn, cause the child’s death by age 20 to 30.
 Approximately 5% of children with thalassemia major continue to produce fetal hemoglobin, and when given the drug hydroxyurea the amount of fetal hemoglobin produced is increased.
Approximately 5% of children with thalassemia major continue to produce fetal hemoglobin, and when given the drug hydroxyurea the amount of fetal hemoglobin produced is increased. Children born with this disorder are usually normal at birth but develop a severe anemia after 6 months of age when hemoglobin F synthesis declines and hemoglobin A synthesis increases.
Children born with this disorder are usually normal at birth but develop a severe anemia after 6 months of age when hemoglobin F synthesis declines and hemoglobin A synthesis increases.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access


