Technical and Clinical Application
Mary Alexander MA, RN, CRNI®, CAE, FAAN
Lisa A. Gorski MS, HHCNS-BC, CRNI®, FAAN
Ann Corrigan MS, BSN, RN, CRNI®
Melody Bullock MS, BSN, RN, CRNI®
Alicia Dickenson RN, CRNI®
Ann Earhart MSN, RN, ACNS-BC, CRNI®
Part I: Anatomy and Physiology
 I. Vascular System
I. Vascular SystemA. Cardiac Circulation
1. Heart
a. A hollow muscular organ made of four chambers that functions as a two-sided pump
1) Right side is a low-pressure system pumping venous or deoxygenated blood to the lung
2) Left side is a high-pressure system pumping arterial or oxygenated blood to systemic circulation
b. Right atrium (RA) is a thin-walled muscle that acts as a receiving chamber
1) It receives systemic venous blood from the superior vena cava (SVC), which drains blood from the upper part of the body, and from the inferior vena cava (IVC), which drains blood from the lower extremities
2) It receives blood from myocardial circulation by the coronary sinus
3) Blood flow to RA occurs during inspiration
a) RA pressure drops below the pressure in veins outside the chest cavity
b) Blood flows from the area of high pressure to the area of low pressure
c. Right ventricle (RV) is the most anterior chamber of the heart, lying directly beneath the sternum
1) Functions as both an inflow and an outflow tract
2) During diastole, blood enters the RV through the tricuspid valve and is ejected into pulmonary circulation through the pulmonic valve
3) Systolic or ejection pressures of the RV may be low because of pulmonary resistance
d. Left atrium (LA) is the most posterior chamber of the heart
1) It receives oxygenated blood from lungs via the right and left pulmonary veins
2) Its wall is slightly thicker than that of the RA and exerts a pressure of 5 to 10 mm Hg with little breathing variation
e. Left ventricle (LV) is the chamber that lies posterior to and to the left of the RV
1) Its wall is made of thick, muscular tissue; two to three times thicker than that of the RV
2) Increased muscular mass is necessary to generate pressure to move blood into circulation
2. Cardiac valves
a. The heart’s efficiency as a pump depends on the integrity of the cardiac valves, whose sole purpose is to ensure one-way forward blood flow
b. Atrioventricular (AV) valves: positioned along the AV groove separating the atria from the ventricles
c. Tricuspid valve: located between the RA and the RV
1) Larger and thinner than the mitral valve, with three separate leaflets: anterior, posterior, and septal
2) Anterior and posterior leaflets associated with RV lateral wall function
3) Septal leaflet attached to portions of the interventricular septum sitting in close proximity to the AV node
d. Mitral valve: located between the LA and the LV; composed of two cusps
1) Anterior leaflet descends deep into the LV during diastole and rises quickly during systole to meet the posterior leaflet
2) Posterior leaflet is smaller and more restricted in its motion
e. Semilunar valves: smaller than the AV valves
1) Aortic semilunar valves
a) Located above the outflow tract of the LV
b) Composed of a fibrous supporting ring called the annulus and three-valve leaflet cusps that are thicker than those of the AV valves
2) Pulmonic semilunar valve
a) Located above the outflow tract of the RV at the junction of the pulmonary artery and the RV
b) Composed of a fibrous supporting ring called the annulus and three-valve leaflet cusps
3. Nerve conduction
a. Involves a special system consisting of atypical muscle fibers that transmit and coordinate electrical impulses throughout the heart
b. Sinoatrial (SA) or sinus node: located at the border of the SVC and the RA
1) Gives rise to a self-generating impulse known as the heartbeat
2) Primary pacemaker of the heart, generating impulses at a rate of 60 to 100 beats per minute (bpm)
3) Innervated by sympathetic and parasympathetic nerve fibers
c. AV node: located in the RA
1) Forms the conduction system of the heart
2) Filters atrial impulses as they pass through the ventricles
3) Innervated by the autonomic nervous system
d. Bundle of His: located along the two sides of the intraventricular system, dividing into the right and left bundle branches and providing infranodal conduction
e. Right and left bundle branches: located in the outer walls of the ventricles
1) Conduction system of the heart working with the bundle of His and the Purkinje fibers to produce contraction of the ventricles
2) Terminate in a fine network of conductive tissue called Purkinje fibers
f. Purkinje fibers: fibers extending to the papillary muscles and lateral walls of the ventricles; located in the upper outer walls of the ventricles
B. Pulmonary Circulation
1. Blood flows from the RV to the lungs via pulmonary arteries and from the lungs to the LA via pulmonary veins
2. Major purpose is to deliver blood to the alveoli where oxygen is taken into the cells and carbon dioxide is removed
C. Systemic Circulation
1. Blood flows from the LV through the aorta and all its branches (arteries) to the capillaries of the tissues
2. Blood returns to the heart through veins and the vena cavae, which empties into the RA
3. Arteries
a. Layers
1) Tunica intima: inner elastic endothelial lining consisting of smooth layers of flat cells
2) Tunica media: middle layer consisting of muscular and elastic tissue
a) Strong layer that withstands pressure, preventing the collapse of vessels
b) Location of nerve fibers for vasoconstriction and vasodilation
c) Responsive to stimulation of chemical irritation by producing spasms that may cause a contraction, cutting off blood flow to surrounding tissues, and resulting in necrosis and gangrene
3) Tunica adventitia: thick outer layer consisting of areolar connective tissue that provides vessel protection
b. Characteristics
1) Contains bright red blood
2) Pulsates
3) Valves not present
4) Usually located deep in tissue protected by muscle
5) Branches terminate in arterioles, which form arterial capillaries
6) Aberrant arteries—located superficially in an unusual place
c. Nerve conduction
1) Sympathetic innervation: direct effect on arteries
a) Control of contraction and relaxation of muscle fibers within the vessels; vasoconstrictor fibers constrict vascular smooth muscle; vasodilator fibers relax vascular smooth muscle
b) Vascular reflexes are aided by chemical actions in regulating the diameter of the vessels to distribute the blood properly to tissues
2) Parasympathetic innervation: indirect effect on arteries
a) Baroreceptors located in the carotid sinus and the aortic arch
b) Activated by impulses to heart, stimulating parasympathetic fibers causing a decrease in heart rate and dilation of arterioles
d. Arteries appropriate for vascular access
1) Radial artery
a) Direct continuation of the brachial artery beginning 1 cm distal to the bend of the elbow, descending along the lateral side of the forearm to the wrist
b) Usually considered site of choice for arterial line placement
2) Ulnar artery
a) Large terminal branch of the brachial artery beginning just distal to the elbow and reaching the medial side of the forearm midway between the elbow and the wrist, and passing vertically, crossing the flexor retinaculum lateral to the ulnar bone
b) Larger, much deeper, and more difficult to stabilize than the radial artery
3) Femoral artery
a) Artery located midway between the anterior superior spine of the ilium and the symphysis pubis
b) Largest accessible artery; easily palpated, stabilized, and entered
4) Pulmonary arteries
a) Arteries leading away from the heart to the lungs
b) The left pulmonary artery is shorter and smaller than the right and runs horizontally in front of the descending aorta and the left principal bronchus to the left hilum, dividing into upper and lower lobar branches
c) The right pulmonary artery is longer and larger and runs horizontally to the right behind the ascending aorta, SVC, and upper right pulmonary vein, and then in front of the plexus
e. Advantages of use
1) Diagnosis
a) Measurement of carbon dioxide and oxygen levels
b) Measurement of bicarbonate blood levels
2) Continuous arterial monitoring
a) Systolic, diastolic, and mean arterial pressure readings
b) Assessment of cardiovascular effects of vasopressor and/or vasodilator drugs during the treatment of shock
c) Simultaneous drawing of arterial blood for arterial blood gases (ABGs)
f. Disadvantages of use
1) Arterial spasms with resultant loss of circulation to an extremity
2) Thrombosis with resultant loss of limb or life
3) Threat of infection and septicemia
4) Cardiac arrhythmias if catheter is placed in the RA
4. Veins
a. Layers
1) Tunica intima: inner elastic endothelial lining consisting of smooth layers of flat cells
a) Semilunar folds of endothelium form valves
b) Trauma during venipuncture encourages thrombosis, whereby cells and platelets adhere to vessel wall
2) Tunica media: middle layer consisting of muscular and elastic tissue
a) Not as strong as in arteries; tends to collapse or distend as the pressure within vein falls or rises
b) Location of nerve fibers for vasoconstriction and vasodilation: cold solutions result in spasms, impeding blood flow and causing pain; heat promotes vasodilation, relieving spasm, improving blood flow, and relieving pain; heat promotes dilation of vessels, reducing inflammation of vessel wall by increasing blood flow and diluting irritating medications or solutions
3) Tunica adventitia: outer layer consisting of areolar connective tissue providing vessel protection; not as thick as in the artery
b. Characteristics
1) Contains dark blood
2) Does not pulsate
3) Valves are present
4) Located superficially
5) Venous capillaries unite to form venules, which unite to form veins
c. Nerve conduction
1) Sympathetic innervation: direct effect on veins
a) Innervation by postganglionic efferent and primary afferent nerves
b) Controls contraction and relaxation of muscle fibers within vessel walls; vasoconstrictor fibers constrict vascular smooth muscle; vasodilator fibers relax vascular smooth muscle
2) Parasympathetic innervation: indirect effect on veins
a) Baroreceptors located in carotid sinus and aortic arch
b) Activated by impulses to heart, stimulating parasympathetic fibers and causing a decrease in heart rate and dilation of venules
d. Veins appropriate for peripheral infusion therapy
1) Digital veins
a) Flow along the lateral portions of the fingers
b) From adjacent sides of digits unite to form three metacarpal veins
c) Last resort for therapy
2) Metacarpal veins
a) Formed by the union of digital veins found on the dorsal aspect of the hand
b) Usually well adapted for infusion therapy
c) Occasionally contraindicated in the elderly because of inadequate tissue and thin skin in the area
d) Use in initial therapy enables successive venipunctures above previous sites, promoting availability of veins without inflammation and pain
3) Cephalic vein
a) A large vein formed by metacarpal veins and located in the radial part of the dorsal venous network, flowing upward along the radial border of the forearm
b) Provides a natural splint for the placement of catheter
4) Basilic vein
a) Originates in the ulnar part of the dorsal venous network, ascending along the ulnar portion of the forearm
b) Visualization is promoted by flexing elbow and bending arm upward
5) Median antebrachial vein
a) Arises from venous plexus on the palm of the hand and extends upward along the ulnar side of in front of the forearm
b) Varies as to size and visibility
6) Intermediate (median) cephalic vein
a) A large vein located in the antecubital fossa
b) Typically used for blood withdrawal
c) Cautious use is necessary because the vessel crosses in front of the brachial artery
7) Intermediate (median) basilic vein
a) Located outside the antecubital fossa on the ulnar curve of the arm
b) Difficult to access for venipuncture
e. Peripheral veins appropriate for central infusion therapy
1) Basilic vein
a) Passes upward in a smooth path along the inner side of the biceps muscle and terminates in the axillary vein
2) Brachial vein
a) Located between the basilic and cephalic vein
b) Runs close with the brachial nerve complex
c) Confluences with the basilic vein below the axillary vein
3) Cephalic vein
a) Ascends along the outer border of the biceps muscle to upper third of the arm, passing in the space between pectoralis major and deltoid muscles, terminating in the axillary vein with a descending curve just below the clavicle
b) Occasional connection with external jugular or subclavian vein by a branch that passes from it upward in front of the clavicle
4) External jugular vein
a) Easily recognized on the side of the neck; formed by the union of the posterior retromandibular and posterior auricular veins near the mandibular angle just below or in the parotid gland, descends to the midclavicle joining the subclavian vein
b) Threat of air being pulled into the vascular system if the administration set is accidentally disconnected
f. Central veins appropriate for central infusion therapy
1) Internal jugular vein
a) Begins at the cranial base in the posterior compartment of the jugular foramen and descends in the carotid sheath uniting with the subclavian, posterior to the sternal end of the clavicle to form the brachiocephalic vein
b) Often used when anomalies of the subclavian vein prevent use or in emergency situations when needed to administer large volumes of fluid quickly
c) Threat of air being pulled into the vascular system if the administration set is accidentally disconnected
d) Preferred as the site of insertion when the risk of thrombosis is higher than the risk of infection
2) Subclavian vein
a) Continuation of the axillary vein extending from the outer border of the first rib to medial border of the scalenus anterior muscle, where it joins the internal jugular to form the innominate (brachiocephalic) vein
b) Clavicle and subclavius muscles lie anterior to the subclavian vein; subclavian artery lies posterosuperior, separated by the scalenus anterior muscle and the phrenic nerve; first rib and pleura lie inferior
c) Vein of choice for the placement of central vascular access devices (CVADs) because of its easy accessibility in emergency situations and lower risk of infection
3) Femoral vein
a) Continuation of the popliteal vein, ending posterior to the inguinal ligament at the external iliac and posterolateral to the femoral artery
b) Usually has four to five valves
c) Least favorable site for the placement of catheters
g. Scalp veins used for infusion therapy
1) Superficial temporal vein
a) Begins in a widespread network joined across the scalp to the contralateral vein and to the ipsilateral, supratrochlear, supraorbital, posterior auricular, and occipital veins
b) Ease in visualizing and has minimal risk
2) Parietal vein
a) A branch of superficial temporal vein located in front of the ear
b) Usually not a vein of choice because of close proximity to the ear
3) Occipital vein
a) A branch of temporal vein located behind the ear
b) Usually the last choice because of its location behind the ear
4) Frontal (supratrochlear) vein
a) Originates on the forehead from a venous network connected to the frontal tributaries of the superficial temporal vein; metopic vein forms the section of frontal vein that runs down the center of the forehead
b) Most frequently used scalp vein
h. Other veins used for infusion therapy
1) Umbilical vein
a) Located within the umbilical cord through umbilicus to liver and ductus venous
b) Frequently used for administering infusion therapy in newborns
c) Its use is limited because of the high risk of sepsis
2) Great saphenous vein
a) Runs along the medial aspect of the leg from ankle upward across knee and thigh to enter femoral ring
b) Lower division above the ankle is frequently used in infants and toddlers
c) Not recommended for use in adults
d) Its use may require a licensed independent practitioner’s (LIP’s) written order
e) Originates with capillaries of superficial tissues of the foot; can lead to complications when used for infusion therapy
f) Thrombosis occurs more readily than when veins in upper extremities are used, leading to pulmonary emboli
g) More valves are present, creating the potential for medication to pool behind valves and creating irregular drug absorption
h) Patient immobilization potentiates pooling of blood in extremities
5. Capillaries
a. Minute blood vessels connecting the smallest arteries (arterioles) to the smallest veins (venules)
b. Exchange of nutrients and oxygen from the blood to the tissues with waste and carbon dioxide from the tissues into the blood (exchange vessels)
 II. Integumentary System
II. Integumentary SystemA. Epidermis
1. Outer layer forms a protective covering
2. Thickness varies, depending on the body part and age
3. Provides support for an intravenous catheter
B. Dermis
1. Connective tissue layer supporting the epidermis
2. Highly vascular, providing nutrition for the epidermis
3. Contains capillaries and nerve fibers that react to temperature, touch, pressure, and pain
C. Superficial Fascia (Hypodermis)
1. A layer of loose connective tissue
2. Contains same collagen and elastin fibers as the dermis
3. Adipose tissue and fat cells are also found here and serve as energy stores and thermal insulators
III. Nervous System
A. Central Nervous System
1. Brain
a. A large mass of nerve tissue filling the cranium
b. Three connective tissue layers called meninges cover the brain and provide protection
1) Dura mater: outermost double fibrous layer that separates the skull into compartments by its various folds or processes
2) Arachnoid: middle layer made up of a two-layered fibrous elastic membrane that crosses over the folds and fissures of the brain, creating the spongy arachnoid space
3) Pia mater: innermost layer rich in small blood vessels, supplying the brain with a large volume of blood
c. Anatomically divided into four components: cerebrum, cerebellum, brain stem, and ventricles
d. Cerebrum is the largest portion of the brain
1) Comprised of gray cells and white matter
2) Divided into hemispheres or lobes that are named according to overlying cranial bones
a) Frontal lobe
Located in the anterior fossa, extending from the anterior portion of each hemisphere to the central sulcus posteriorly
Controls psychic and higher intellectual functions and higher level centers for autonomic functioning, such as cardiovascular responses and gastrointestinal activity
b) Parietal lobe
Located in the middle fossa in the area between the fissure of Rolando and the parieto-occipital fissure
Major functions are position, sense, touch, and motor movement
c) Occipital lobe
Pyramidal structure located in the middle fossa behind the parieto-occipital fissure just above the cerebellum
Contains the centers for vision
d) Temporal lobe
Located in the middle fossa inferior to the lateral cerebral fissure and extends posteriorly to the parieto-occipital fissure
Responsible for primary functions of memory and hearing
e. Cerebellum is approximately one-fifth the size of the cerebrum
1) Functions primarily in coordinating movement, equilibrium, muscle tone, and position sense
2) Consists of two lateral hemispheres and a middle portion, the vermis
a) Lateral hemispheres control the movement coordination for the same side of the body
b) Midbrain connects the cerebellum to the cerebral cortex
f. Brain stem consists of the midbrain, the pons, and the medulla oblongata
1) Midbrain (mesencephalon)
a) Forms a junction between diencephalon and pons
b) Functions to relay stimuli dealing with muscle movement, visual reflexes, and auditory reflexes from the spinal cord, medulla oblongata, and cerebellum to the cerebrum
2) Pons
a) Connects the midbrain to the medulla oblongata
b) Relays impulses to brain centers and to lower spinal centers of the nervous system
c) Origin for sensory and motor nuclei of the trigeminal, abducens, facial, and acoustic nerves
3) Medulla oblongata
a) Contains reflex centers for controlling involuntary functions such as breathing, sneezing, swallowing, coughing, salivating, vomiting, and vasoconstriction
b) Provides points of origin for the glossopharyngeal, vagus, spinal accessory, and hypoglossal nerves
g. Ventricles are cavities located deep within the brain
1) Filled with cerebrospinal fluid (CSF), which is produced mostly by lateral ventricles
2) Connect with each other and with fluid spaces in the spinal cord through small openings
3) Lateral ventricles serve as a site for the placement of Ommaya reservoir
2. Spinal cord
a. Ovoid column of nervous tissue extending through the spinal canal
1) Originates at the foramen magnum and ends at the superior border of L2
2) Tapers in the lower thoracic area into a cone-shaped structure called the conus medullaris
3) Anchored to the coccyx by the filum terminale, a thin prolongation of the conus medullaris
b. Serves as a center for spinal reflexes and a conducting pathway of impulses to and from the brain
c. Consists of gray (unmyelinated) and white (myelinated) matter
1) Gray matter integrates the cord reflexes
a) Has an internal core resembling a butterfly on cross section
b) Has a pair of projections forming the back wings—posterior or dorsal horns—consisting of multipolar neuron structures that form the motor efferent neurons of the ventral roots or spinal nerves
c) Contains cell bodies and dendrites of sensory neurons and sensory receptors from the periphery
2) White matter surrounds the gray matter
a) Consists of long ascending and descending tracts
b) Serves as the pathway between spinal cord and brain for afferent and efferent impulses, which are grouped into anatomical and functional bundles called fasciuli
d. Divided into lateral halves, with each lateral half divided into three sections that run the length of the spinal cord: dorsal, lateral, and ventral
e. Contains distinct fiber tracts
1) Ascending fibers bring sensory information to the central nervous system
2) Descending fibers carry impulses from the brain to motor neurons of the brain stem, spinal cord, and internuncial (association) neurons, which form short ascending and descending tracts that travel between spinal segments
f. Protected by other structures
1) Vertebral column
a) Runs from foramen magnum to sacral hiatus, with bony arches of the vertebrae posterior to the vertebral bodies forming a continuum to make up the spinal canal, with spaces between the vertebrae being taken up by spinal ligaments
b) Consists of 7 cervical, 12 thoracic, and 5 lumbar vertebrae with the sacrum and coccyx inferiorly
2) Spinous processes
a) Prominent at the posterior part of each vertebra
b) Angulation varies and is an important consideration when inserting a needle into the epidural space
Processes almost horizontal in the cervical, lower thoracic, and lumbar regions; may require needle to be inserted at right angles to the sagittal plane
Processes directly caudal in the midthoracic region with maximal angulation between T7 and T8; may require needle to be inserted at varying degrees from the horizontal
3) Spinal ligaments
a) Supporting structures that hold vertebrae together posteriorly
b) Provide access to the spinal canal
c) Supraspinous ligament runs superficial to tips of spinous processes
d) Interspinous ligament connects posterior spinous processes
e) Ligamentum flavum connects laminae of the vertebra
Tougher than other ligaments and easily identified by its increased resistance to needle insertion
Not present in the sacrum, where the laminae are fused together except at the fifth sacral vertebra, which has no laminae and thus forms the sacral hiatus through which the spinal canal may be entered when performing a caudal (sacral) block
4) Other spinal ligaments
a) Anterior longitudinal ligament
Runs from skull to sacrum
Firmly attached to the discs and adjacent margins of vertebral bodies
b) Posterior longitudinal ligament
Connects posterior aspects of the vertebral bodies
Forms anterior wall of the vertebral column
5) Meninges (three-layered membrane coverings)
a) Pia mater: membrane covering, closely attached to spinal cord and spinal nerves
Laterally attached to spinal nerve roots, eventually joining arachnoid and dura mater to become the connective tissue surrounding and investing the spinal nerves
Separated from arachnoid mater by the subarachnoid space, which contains CSF produced by the choroid plexuses in the brain ventricles
b) Arachnoid mater: thin membrane lying close to the dura mater but separated by the subdural space, which contains lymph
c) Dura mater: thick band of tissue covering spinal cord and its two coverings
Space between dura mater and vertebral column called the epidural space contains areolar tissue, fat, and a number of venous plexuses
g. Supplied by numerous blood vessels throughout the epidural space that supply and drain blood from the vertebrae, the spinal cord, its coverings, and the spinal nerves
B. Peripheral Nervous System
1. Cranial nerves form the peripheral nerves of the brain
a. Divided according to function
1) Five pairs have only motor fibers
2) Three pairs have only sensory fibers
3) Four pairs have both sensory and motor fibers
b. Correspond to the spinal nerves serving common sensation, voluntary control of muscles, and autonomic functions in the head, including the mechanism for the special senses of vision, hearing, smell, and taste
2. Spinal nerves: 31 pairs arise from different segments of the spinal cord
a. Each pair is formed by the union of anterior and posterior roots attached to the spinal column
b. Each pair with its corresponding part of the spinal cord constitutes a spinal segment
1) Cervical nerves: four pairs join at anterior rami to form a complex network of nerve fibers called a plexus
a) Cervical plexus: first four pairs supply sensory and motor impulses to back of head, in front of neck, and upper part of shoulder to numerous neck muscles
b) Brachial plexus: latter four pairs supply sensory and motor impulses to scapula and muscles of upper extremities
2) Thoracic nerves: 12 pairs with branches running directly to intercostal muscles and skin of thorax
a) Provide both sensory and motor impulses
3) Lumbar nerves: five pairs extend obliquely and inferiorly, making up the lumbosacral plexus
a) Innervate lower extremities
b) Carry both sensory and motor impulses
4) Sacral nerves: five pairs
a) Four pairs emerge through the posterior sacral foramina
b) Fifth pair emerges through the sacral hiatus, carrying both sensory and motor impulses
5) Coccygeal nerves: one pair
a) Part of the lumbosacral plexus
b) Carry both sensory and motor impulses to the lower extremities
C. Autonomic Nervous System
1. Part of the peripheral nervous system that regulates the body’s internal environment in close conjunction with the endocrine system
2. Responsible for the unconscious moment-to-moment functions of all internal systems, including visceral organs, involuntary fibers, and glandular functions
3. Activated by centers in the hypothalamus, brain stem, and spinal cord
a. Sympathetic nerves
1) Consist of pre- and postganglionic nerve fibers arising from nerve cells in lateral column of gray matter of spinal cord
2) Transmit impulses that cause an increase in blood pressure and heart rate and vasoconstriction of peripheral blood vessels when external stress situations occur
a) Most frequently termed the fight or flight reaction
b) Transmitter substance, norepinephrine, is secreted by postganglionic nerve terminals
b. Parasympathetic nerves
1) Consist of preganglionic fibers arising from cell bodies in cranial nerves III, VII, IX, and X and spinal nerves II through VII
2) Activated when the body is at rest or relaxed, and also protect and restore the body’s resources
 IV. Skeletal System
IV. Skeletal SystemA. Functions
1. Bones collectively form the framework that supports the body; skeletal system enables the body to stand erect
2. Protects internal organs and other soft tissues
3. Assists movement by leverage and in coordination with muscles
4. Manufactures blood cells
5. Acts as reserves of minerals, particularly calcium and phosphorus
B. Bone Shapes
1. Short bones make up wrist and ankle
2. Flat bones make up sternum and scapula
3. Long bones comprise arm and leg
a. Consist of three parts
1) Shaft, or long part of the bone
2) Metaphysis, or flared part at the end of the shaft
3) Epiphysis, or rounded end
b. Epiphyseal cartilage
1) Plate of soft tissue between epiphysis and metaphysis
2) Provides growth
4. Irregular bones make up vertebrae and patella
C. Periosteum
1. All bones are covered with a double-layered connective tissue called periosteum
2. The outer layer of the periosteum
a. Contains blood vessels and nerves
b. Some penetrate into the inner structures of the bone through channels called Volkmann canals
3. The inner layer of the periosteum
a. Anchored to the bone by collagenous fibers (Sharpey fibers) that penetrate the bone
b. Sharpey fibers help hold or attach tendons and ligaments to the periosteum of bones
D. Intraosseous Space
1. Bone is made up of two types of bone tissue (osseous tissue)
a. Compact (cortical); makes up 85% of skeleton
b. Spongy (cancellous); makes up 15% of skeleton
2. Compact bone is highly organized, solid, and extremely strong
a. Basic structural unit in the compact bone is the Haversian system
b. Each Haversian system contains
1) A central canal called the Haversian canal
2) Concentric layers of bone matrix called lamellae
3) Tiny spaces (lacunae) between the lamellae
4) Bone cells (osteocytes) within the lacunae
5) Small channels or canals called canaliculi
c. Each Haversian is a separate cylindric entity
d. The Haversian canal runs through the long axis of the bone
1) Contains one or two blood vessels and nerve fibers
2) The blood vessels in the canal communicate with blood vessels in the periosteum (surface cover) and marrow cavity to transport nutrition and wastes to and from the osteocytes contained within the lacunae
3) Surrounding each Haversian canal are the concentric lamellae
4) Between the lamellae are the lacunae; each contains one osteocyte
5) The lacunae are connected to each other and to the Haversian canal by the canaliculi; run parallel to the horizontal axis of the bone
3. Spongy bone is less complex and lacks Haversian systems
a. The lamellae are arranged in plates or bars called trabeculae
b. Trabeculae branch and unite with one another to form an irregular meshwork. The pattern of meshwork is determined by the direction of stress on the bone
c. The space between the trabeculae is filled with red bone marrow
d. Osteocyte-containing lacunae are distributed between the trabeculae and interconnected by canaliculi
e. Capillaries pass through the marrow to nourish the osteocytes
Part II: Equipment
 I. Solution Containers
I. Solution ContainersA. Material
1. Glass
a. Necessary for certain solutions that are incompatible with or will leach through plastic
b. Easily broken when transported if caution is not taken to prevent breakage
c. Assess container in light before use; it is necessary to detect fine cracks through which microorganisms can enter
2. Plastic
a. Suitable for most solutions
b. Easily transported with minimal risk
c. Squeeze before use to detect punctures because bags are susceptible to punctures that may go undetected and allow microorganisms to enter
B. Volume Sizes
1. Containers for premixed solutions range from 50 to 1,000 mL
2. Plastic containers for use in preparing solutions are available that will hold as much as 4,000 mL (frequently used for parenteral nutrition [PN] solutions)
C. Types of Systems
1. Air-dependent (open system)
a. Refers to glass bottles that do not collapse as the solution leaves the bottle
b. Requires venting (air within system) for the solution to flow
1) Air must enter the solution container through vented administration set or vented spike adapter
2) The use of needles to vent solution containers is inappropriate because needles allow microorganisms to enter the solution increasing the risk for a bloodstream infection
2. Nonair-dependent (closed system)
a. Refers to plastic bags that collapse as the solution empties
b. Does not require air for the solution to flow
c. Reduces risk of air embolism and airborne contamination because of closed system
D. Nursing Considerations
1. Perform hand hygiene before opening or spiking solution containers
2. Inspect bags and bottles before use for cracks, leaks, damaged ports or seals, expiration date, clarity, discoloration, turbidity, and particulate matter; discard and report
3. Label bags and bottles with date and time when the solution container was opened
4. Cover solutions containing medications that are light-sensitive to prevent degradation of medication
5. Discard solution containers removed from the infusion system; do not save for later use; cover or remove label if it contains patient information
 II. Administration Sets
II. Administration SetsA. Materials
1. Polyvinyl chloride (PVC) with di-2-ethylhexyl (DEHP)
a. Used for majority of administration sets
b. Not compatible with lipids and some medications
2. PVC without DEHP
a. Used for administration of lipids
b. DEHP is lipophilic and is extracted into the lipid solution
c. DEHP is considered a toxin
3. Non-PVC lined (polyethylene-lined)
a. Used for nitroglycerin administration
B. Types
1. Primary continuous administration set
a. Provides for administration of a primary solution
b. Does not provide measured volumes
c. May or may not have injection ports
d. Injection ports do not have a check valve, therefore, do not prevent solutions or medications from flowing back up the administration set and mixing with the primary solution
2. Secondary administration set
a. Typically shorter in length than the primary administration set
b. Used for the administration of piggyback medications
c. Attaches to the primary administration set at the Y-port above the back-check valve
1) Flow-control slide clamp is an on–off clamp only
2) Clamp is never used to regulate the flow of medication
3. Primary Y set
a. Allows alternate or simultaneous infusion of two solutions
b. May contain a filter or an in-line hand pump for the administration of blood
c. Use involves a hazard of air embolism because large quantities of air can be drawn into the administration set if one container is allowed to empty
4. Metered-volume chamber set
a. Contains a vented, calibrated chamber
b. May contain a microporous filter to block the passage of air when the chamber empties
c. Used frequently to measure solutions administered at a microdrip rate
d. Allows medications to be added directly into the chamber through the medication port
5. Specialty sets
a. Retrograde set
1) Placed proximal to the infusion site
2) Allows solution displacement within the set into a syringe as medication is injected into the set
3) Allows administration of medication proximal to the site, eliminating loss of medication from adherence to the administration set
4) Used to administer medications to neonates and pediatric patients
b. Dedicated set
1) Contains a specific segment that adapts to use with a specific infusion device
2) Used only with devices for which it is designed
3) May or may not allow priming outside of the infusion device
C. Characteristics and Features
1. Vented sets
a. Allows air to enter the system through a filtered vent
b. Required for glass containers
2. Nonvented sets
a. Do not allow air to enter the system
b. Used with plastic systems
3. Universal sets
a. Can be used with both glass bottles and plastic systems
b. Has a capped, filtered vent
1) Opening the cap allows air to enter the solution container
2) Keeping the cap closed prevents air from entering the solution container
4. Back-check valves
a. Allows the solution to flow in one direction only
b. Used to administer secondary (“piggyback”) medications/solutions
c. Prevents mixing of primary and secondary solutions, or mixing of primary solution and medications administered through injection ports
1) Primary solution is lowered on a wire or plastic hanger, creating greater head-height pressure for secondary solution
a) Secondary solution flows and primary solution stops
b) When the secondary solution is complete, primary solution flows automatically
2) Risk of air entering the tubing between infusion of primary and secondary infusions is eliminated; occlusion due to interruption of infusion is prevented
3) Rate of administration remains the same for both primary and secondary solutions when used without an infusion device because the flow rate is regulated by one clamp
5. Drop factor
a. Number of drops delivered in one milliliter (mL)
b. Macrodrip
1) Set that delivers from 10 to 20 drops/mL
2) Used to deliver solutions when critical measurement or small volumes are not required
c. Microdrip
1) Set that delivers 50 to 60 drops/mL
2) Used to deliver solutions when critical measurement or small volumes are required
d. Calculation of flow rate
1) Determined by the use of a quick, easy formula:
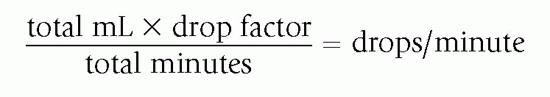
2) Consideration is given to the height of the solution container, blockage of or change in the position of the catheter, venous spasms, and viscosity of fluids because each has a direct impact on the drop size or the rate at which the drop may fall
6. Internal administration set diameter
a. Dictates the required priming volume of the set and is manufacturer-specific
b. Standard administration set
1) Allows for infusion flow at a standard rate; have common inner lumen size with very little variation from manufacturer to manufacturer
2) Routinely used for the administration of medications and solutions when critical measurement or small volumes are not necessary
c. Microbore administration set
1) Inner lumen smaller than the standard set
2) Used for administering infusions to neonates, pediatric patients, and volume-restricted adults
3) Considered for use when small amounts are infused or a slow rate is desired
4) Solution viscosity may decrease the flow rate
d. Macrobore administration set
1) Inner lumen larger than the standard set
2) The increased size of the lumen and drop size of the infusion allows for a rapid infusion flow
3) Indicated when large amounts of fluid or blood are needed quickly, such as with trauma patients
7. Manual flow control devices: clamps
a. Device on administration set that allows the user to affect the flow rate of the solution by increasing or decreasing the diameter of the tubing
b. Roller clamp
1) Uses a plastic roller to adjust the tubing diameter by applying pressure on the tubing, allowing regulation of the flow rate
2) Used on most administration sets
3) Requires time-consuming adjustments to establish and maintain the rate because changes in drop rate can occur after the rate has been regulated
c. Slide clamp
1) Clamp that slides across the tubing to open or close the administration set
2) On-off clamp only; should not be used to regulate the flow
8. Injection ports
a. Purpose
1) To allow for the infusion of secondary solutions or medications; piggyback administrations
2) To administer medications proximal to the site, such as with an “IV push” or bolus medication
b. Location
1) Distal to drip chamber
2) Proximal to the distal end of the administration set
c. Configuration and number vary with type and purpose of the administration set
d. Configured as a needleless port
1) Needles are not used for the administration of medications/solutions
2) Provides a built-in safety feature or mechanism that effectively reduces the risk of an exposure incident when using the port
9. Connections
a. Luer
1) Recommended method of connection
2) Allows connection of administration set with an add-on device or a catheter by screwing together two compatible ends
3) Deliberate twisting motion required to disconnect luer connection
4) Prevents leaking at connections and accidental disconnections that place the patient at risk of infection, air embolus, and loss of blood through the catheter
b. Slip
1) Allows connection of administration set with an add-on device or catheter by providing fittings that slide into each other and a tight connection when twisted
2) Not recommended for use because it can be easily pulled apart, opening the system to airborne contaminants and possible free flow of blood externally
D. Nursing Considerations
1. Assess product and package integrity before use; do not use if violated
2. Assess patient for latex sensitivity; some administration sets contain parts with latex
3. Determine the appropriateness of the administration set based on medication/solution to be administered
a. Certain medications, such as Paclitaxel (Taxol), must be given through administration sets not made of PVC
b. Administration sets used to administer other medications such as propofol should be replaced every 12 hours, when vial is changed, or according to manufacturer’s recommendations
4. Change primary and secondary administration sets in accordance with the Infusion Nursing Standards of Practice and organizational policies and procedures
5. Change administration sets at the time of the peripheral catheter change or when a new CVAD is placed
6. Treat secondary administration sets detached from a primary administration set as primary intermittent administration sets and change in accordance with the Infusion Nursing Standards of Practice and organizational policies and procedures
7. Place a sterile, compatible covering device to the male end of the primary intermittent administration set after each use
8. To administer lipid emulsions use sets free of DEHP
9. Label administration sets with the date and time of initiation
10. Maintain administration sets as closed systems
11. Disinfect injection ports prior to every use
12. Never flush or irrigate administration sets to improve flow rate
13. Change all administration sets with the catheter and solution container, if phlebitis, thrombophlebitis, cellulitis, or intravenous-related bacteremia is suspected
14. Use a needleless system when accessing the administration set
 III. Add-on Devices and Needleless Connectors (NCs)
III. Add-on Devices and Needleless Connectors (NCs)A. Purpose
1. To add length, filtering capabilities, or increase the overall function of the infusion system
2. Limiting their use reduces the incidence of contamination and accidental disconnection, minimizes the manipulation of the sterile pathway, maintains a closed system, and reduces costs associated with their use
B. Types of Add-on Devices
1. Extension sets
a. Features
1) Used to add length to administration sets or to provide additional entry into the system
2) May or may not have an on-off clamp
3) May or may not have one or more Y ports for use when administering medications or solutions
b. Types
1) Straight extension set
a) Frequently used to add length to administration sets or catheter
b) Extends catheter length to facilitate self-care for home infusion patients
2) Y connector extension set
a) Forms a “Y”
b) Provides two entry points into system
c) Usually has a clamp on both segments of the Y, allowing solutions to run simultaneously or separately
d) May have injection ports or back-check valves in one or both segments to prevent solution backflow into either segment
3) Multi-entry extension set
a) Set with three or more “pigtails,” allowing three or more entries into the system
b) May have clamps, additional injection ports, or check valves in one, two, or all of the segments
2. Stopcocks
a. Used to provide multiple entries into infusion system when additional access is needed or to provide an alternate entry into the system if an emergency arises
b. Available with or without an extension set and with varying types of ports, including needleless ports
c. Use is discouraged due to contamination risks
3. Catheter connection devices
a. A device used to connect the administration set to a catheter
b. Types
1) T connector: shaped like a T usually connected to a short extension set with a slide or pinch clamp attached; frequently used in neonates, infants, and small children; allows safe disconnection of administration set without fear of backflow of blood or air emboli
2) J loops and U connectors: same intended use as T connectors; are rigid and hold their shape when attached to the catheter; predetermined shape creates a disadvantage if the insertion site is in an awkward location
4. Solid caps
a. Closed plastic casings used to cover injection ports, catheter hubs such as dialysis catheters, and the end of syringes filled with medications
b. Disinfection cap
1) Impregnated with a sponge coated with an antiseptic solution; 70% isopropyl alcohol
2) Designed to bathe the connection between accesses
3) Protects the catheter hub from touch and airborne contamination
5. Needleless Connectors (NCs)
a. An add-on device designed to accommodate needleless devices for infusion administration
b. Types by design
1) Simple NC group
a) Simple design with no internal mechanisms; straight fluid pathway
b) Prepierced septum with a blunt cannula or luer-lock design
2) Complex NC group
a) A variety of luer-lock mechanical valves with internal mechanism designs and fluid pathways
b) Allows both injection and aspiration of fluids
c. Types by function
1) Negative displacement: blood reflux into catheter lumen upon disconnection with movement of valve mechanism
2) Positive displacement: small amount of fluid pushed out of the end of the catheter lumen, clearing any blood reflux resulting from disconnection of the administration set or syringe
3) Neutral displacement: internal mechanism prevents blood reflux upon connection or disconnection
C. Nursing Considerations
1. Limit use due to the risk of contamination from manipulation, accidental disconnection, or misconnection
2. Connections should be of luer-lock design and compatible with the administration system
3. Change in accordance with the Infusion Nursing Standards of Practice and organizational policies and procedures
a. When the administration set is changed
b. Immediately suspected contamination or break in integrity
c. If blood or debris visible
4. When removed from a catheter or administration set, the device is discarded and a new device is attached
5. Assess compatibility of solutions/medications administered through each connection to prevent admixing of incompatible solutions/medications in the VAD
6. Ports should be capped when not in use; port cap is considered contaminated once removed; replace with a new sterile cover
7. Before accessing, disinfect ports with an appropriate disinfectant using friction
IV. Catheter Stabilization Devices
A. A device/system designed and engineered to control the movement at the catheter hub, decreasing catheter movement within the vessel and risk of catheter malposition
B. Purposes
1. To preserve the integrity of the access device
2. To minimize the catheter movement at hub
3. To prevent catheter dislodgment and loss of access
C. The method should not interfere with assessing and monitoring of access sites or impede vascular circulation or delivery of prescribed therapy
D. Preferred Alternative to Tape or Sutures to Secure Catheters
E. Protocols for use should be established in organizational policies and procedures and in accordance with manufacturer’s guidelines
 V. Filters
V. FiltersA. Features
1. A device that prevents the passage of air or undesired particulates
2. Product design determines the size of the particulates retained
3. Characteristics vary with the filter used; optimal characteristics include
a. Retention of particulates, bacteria, fungi, and endotoxin
b. Removal of air from system and vents to atmosphere
c. Nonbinding ability with drugs, allowing dosage to pass
d. Allowance for high-gravity flow rates
e. Pressure tolerance to withstand pounds per square inch (psi) of an electronic infusion device (EID)
4. Should not be used as a routine measure for prevention of infection
B. Types
1. In-line filter (filter that forms an integral part of the administration set)
a. Advantages
1) Associated with less risk of contamination because filter is an integral part of administration set design
2) No risk of separation
b. Disadvantages
1) When placed in the upper part of the administration set, instead of at the distal end, retains only those substances that enter the set above the filter
2) Entire set must be changed if filter becomes clogged
2. Add-on filter (filter added to an administration set)
a. Advantages
1) Easily changed when filter becomes clogged or defective without removing the entire administration set
2) Placed at the distal end of the administration set, removing all substances that enter the set above the filter
b. Disadvantages
1) May be accidentally separated from the administration set or catheter, potentiating the risk of infection or possible hemorrhage
3. Filter needle/straw
a. Retains particulate matter >5 microns in size
b. Frequently used when preparing intravenous medications
c. Recommended when withdrawing medications from glass ampoules or multidose vials, particularly if the medication is to be administered as a bolus and cannot be administered through a bacteria-retentive filter
C. Structural Configuration
1. Depth filter: consists of fibers or fragmented material that has been bonded or pressed to form a tortuous maze
a. Cannot be given an absolute rating because the pore size is not uniform; assigned a nominal rating, the particle size above which 98% of the contaminants will be retained
b. Removes particulates only; does not remove air
2. Membrane filter: screen-type filter with uniformly sized pores that provide an absolute rating, retaining all particles on the membrane greater than its size
a. May retain bacteria and fungus, depending on the pore size
b. May have a unique membrane that removes endotoxins, microbial contaminants, particulate matter, and air; bacteria retained may break down after 24 hours and release bacterial toxin confined within the body of a bacterium
3. Hollow fiber filter: contains fibers that trap undesired substances
a. Provides a large filtering area that makes for easy priming and prevents clogging and binding of medications
b. Withstands pressures to 45 psi
D. Surface Area
1. Refers to area with which the solution or medication comes in contact
2. Affects flow rate
a. The larger the surface area, the greater the area through which fluid or medication can flow, increasing the flow rate
b. The smaller the area, the slower the rate
E. Pressure Limitations
1. Rated according to psi of pressure that can be exerted on the filter membrane without rupturing it
2. Consideration necessary before applying a positive-pressure EID; pressure of the infusion device should not exceed the psi of the filter
F. Indications for Use
1. Available in a variety of pore sizes, forms, and materials; pore size determines what substances are retained
2. 0.2-micron filter
a. Absolute bacteria-retentive, air-eliminating filter that removes particulates of 0.2 micron or larger
b. For nonlipid solutions that require filtration
c. Contraindicated for administration of blood/blood components; lipid emulsions; low-dose (<5 microns/mL), low-volume medications (total amount, <5 mg during 24 hours); IV push medications; medications in which the pharmacologic properties are altered by the filter membrane or bind to the filter membrane
d. Air-venting filters automatically vent air through a nonwettable (hydrophobic) membrane and permit uniform high-gravity flow rates through large wettable (hydrophilic) membranes, overcoming flow resistance
3. 1.0 micron filter
a. Removes particulates >1.0 micron; often termed a particulate matter filter
b. May be designed as an integral part of the administration set, as a membrane filter in a metered-volume chamber set, as an add-on device, or as a needle
c. May have air-eliminating properties
d. Recommended use
1) Administration of infusions that contain medications with a pore size >1.0 micron
2) Preparation or administration of solutions or medications to remove particulates that have the potential for obstructing vascular or pulmonary systems
4. 1.2-micron filter
a. Recommended for administering total nutrient admixtures
b. Usually has air-eliminating properties
5. 5 microns filter
a. Particulate matter filter removing particles >5 microns
b. Recommended for use when infusing or admixing medications or solutions with a pore size >5 microns
G. Nursing Considerations
1. Filters should be placed as close to catheter insertion site as possible to achieve final filtration
2. Application and placement should coincide with administration set change, and immediately if contamination is suspected or product integrity is compromised
3. Use should comply with manufacturer’s directions for use
4. When using an EID, the psi rating of the filter should not exceed the psi exerted by the EID
 VI. Vascular Access Devices (VADs)
VI. Vascular Access Devices (VADs)A. Peripheral VADs
1. Needles
a. Stainless steel needle: hollow tube made of stainless steel, may have plastic wings to aid insertion
b. Used for single-dose medications and drawing of blood samples; not left in place as an indwelling device
c. Less thrombogenic than catheters as a result of decreased formation of fibrin sheath around the needle
d. Increased risk of infiltration, a concern if administering vesicant medications or solutions
2. Peripheral catheter
a. A term used to refer to a hollow tube made of plastic that is used for accessing the vascular system
b. Vary in gauge, length, composition, and design
c. Tip of a peripheral catheter terminates in a peripheral vein
d. Types
1) Over-the-needle catheter: catheter with an internal needle stylet to facilitate venipuncture
a) The catheter is threaded into the vessel once venipuncture is made and stylet is then removed and discarded
b) The catheter of choice for peripheral infusion therapy anticipated to last 7 or fewer days
2) Midline catheter: catheter between 3 inches (7.5 cm) and 8 inches (20 cm) in length
a) For intermediate-term therapies of 1 to 4 weeks
b) Inserted above or below antecubital fossa through basilic, cephalic, or median veins, with the tip residing below axilla in the larger vessels of upper arm, providing greater hemodilution
c) Catheter tip does not enter the central vasculature
e. Composition
1) Teflon, PVC, polyurethane, or silicone
2) Varies with regard to thrombogenicity or potential for producing vein inflammation
a) Teflon considered most thrombogenic
b) Silicone considered least thrombogenic
f. Properties
1) Only radiopaque catheters are used so that in the event of a fragmented catheter, the catheter fragment can be visualized by radiography
2) May be entirely radiopaque or may be clear with a radiopaque strip; radiopaque strips may promote insertion because of visibility of blood flow when the vein has been entered
3) Has safety engineered mechanism to reduce the potential for exposure to blood-borne pathogens
a) Passive activation occurs without any action by the inserter to initiate the safety mechanism; preferred choice
b) Active activation requires the inserter to do something to initiate the safety mechanism
4) Double-lumen catheter: a catheter that provides two entries into the vascular system with one venipuncture
a) Provides two separate lumens, one through which the needle stylet resides and a second that appears as a side port with a short extension, which allows exit of solution or medication through an outlet or “eye” above the distal end of the catheter
b) Each port provides independent flow of medications or solutions so that they never mix while infusing through the catheter
g. Gauge and length
1) Gauge refers to the actual lumen size or interior space of the catheter
a) Gauges range from 24 to 12 gauge
b) The larger the number, the smaller the lumen
2) Lengths of short peripheral catheters range 5/8 to 3 inches
3. Nursing considerations
a. Choice of a needle/catheter depends on vein accessibility, type and duration of therapy, and patient preference
b. Use smallest gauge, shortest length catheter that will accommodate the prescribed therapy
c. Assess patient’s vasculature and estimate blood flow around the device to prevent potential complications
B. Central Vascular Access Devices (CVADs)
1. When placed in the upper extremity, the catheter tip resides within the SVC near its junction with the RA; for femoral placement, the tip resides in the IVC above the level of the diaphragm
2. Types
a. Nontunneled percutaneous catheter: a catheter inserted percutaneously through a needle or an introducer, or over a guidewire that has been threaded through the needle or introducer
1) Risk of catheter puncture or shearing when inserting the catheter directly into vein through a needle; the catheter should never be retracted through needle at any time during the procedure
2) The selection of a catheter depends on the duration of the therapy and patient need
3) Used for continuous or intermittent infusions of short duration
4) Includes peripherally inserted central catheter (PICC)
5) Multilumen configuration available
b. Tunneled catheter: a catheter surgically placed by a LIP by tunneling the catheter under the skin from the vein entry point to an exit point on the chest wall; a Dacron cuff encircling catheter provides catheter stability and serves as a barrier to prevent infection
1) Patient’s vascular status, length of therapy, and patient’s preference and ability to care for the catheter considered before placement
2) Dual- and triple-lumen configurations are available to accommodate multiple therapeutic and diagnostic procedures
3) Used for long-term therapies
c. Implanted ports
1) Implanted VAD: plastic, stainless steel, or titanium housing (i.e. port) attached to a catheter surgically implanted under the skin by a LIP
2) Noncoring needles: steel needles with angled and deflected points used to access implanted ports
a) Available in variety of gauge sizes and lengths
b) The length of the needle may be determined by the depth at which implanted port is placed or size of a patient; generally range from ½ to 1½ inch
c) The needle point slices the septum of the port on entry and during removal, preventing coring
d) Available in straight and 90° angle configurations, with or without extension sets
3) Catheter insertion sites
a) Jugular or subclavian veins are used for ports placed on the chest wall and threaded into the SVC
b) Cephalic or basilic veins are used for ports placed on an upper extremity and threaded into the SVC
4) Considerations
a) Available venous access
b) Duration of therapy
c) Patient preference and ability to care for port
d) Catheter of choice by many patients because of the need for minimal care since it is implanted under skin
5) Used for long-term therapies
6) May be of single- or dual-lumen configuration
7) Placement and removal is a medical act
3. Composition
a. Made of polyurethane or silicone
b. Vary as to thrombogenicity or potential for producing vein inflammation
c. Silicone considered least thrombogenic and most preferred
4. Properties
a. Radiopaque so that catheter tip placement can be verified by radiography
b. Short-term nontunneled catheters may be impregnated or coated with chlorhexidine acetate, chlorhexidine/silver sulfadiazine, minocycline/rifampin, or silver ion to help reduce central line-associated blood stream infections (CLABSI)
c. Some CVADs are specifically designed to tolerate the high pressure required for rapid injection used in some CT scans
5. Size and length
a. Dependent on catheter type and insertion site
b. Central catheters are referred to by French size; ranging from 5 to 12 French
c. Central catheters range in length from 5 to 25 cm
d. Catheter length should allow for tip placement in the vena cava
6. Configuration
a. Lumens
1) Single-lumen catheters: provide one port of entry into the vascular system
a) Less risk of CLABSI due to less manipulation with single lumen
b) Use is restricted because of only one entry point
2) Multilumen catheters: provide two or more catheter lumens for multiple entries into the vascular system
a) Accommodate multiple therapeutic or diagnostic procedures
b) May increase the risk of CLABSI secondary to increased access/manipulations
b. Safety mechanisms: to reduce the potential for exposure to blood-borne pathogens
7. Insertion techniques
a. Direct venipuncture: associated with insertion of central catheters directly into the vein, usually subclavian or jugular
b. Tunneled: associated with tunneling of the catheter from the entry point into the vein to an exit point on the chest wall
c. Implanted: associated with port implantation under the skin, usually on the chest wall, with the catheter being placed in the subclavian or internal jugular vein
d. Peripherally inserted: insertion of a catheter usually into the basilic or cephalic vein at the antecubital fossa, with threading of the catheter into the SVC
8. Nursing considerations
a. Before use, tip location must be confirmed by chest radiograph
b. Remove upon unresolved complication, therapy discontinuation, or if deemed unnecessary
 VII. Local Anesthesia
VII. Local AnesthesiaA. Purpose: to alleviate pain associated with procedure-related pain
B. Types
1. Transdermal analgesic cream or patch
2. Intradermal injection of 1% lidocaine hydrochloride solution
3. Iontophoresis technology: delivers drugs through the skin by using an electric current
4. Pressure-accelerated lidocaine
C. Nursing Considerations
1. Select the local anesthetic agent or a method that is the least invasive and carries the least risk for allergic reaction
2. Base selection on the patient’s condition, needs, risks, and benefits associated with cannulation or port access
 VIII. Navigational and Visualization Devices
VIII. Navigational and Visualization DevicesA. Ultrasound Devices
1. Provide real-time imaging of the vein
2. Use requires special training and an understanding of the vascular system
3. Used for the placement of central catheters including PICCs; growing trend to use for the placement of midline and short peripheral catheters
4. Uses sound waves to locate structures in the human body
a. Two major components: the transducer and the imaging instrument
b. The transducer can be positioned to obtain a transverse or cross-sectional view of the vein or a longitudinal view
B. Catheter Location Systems
1. Electromagnetic tracking
a. Detects electromagnetic signal from guidewire transmitted to a monitor
b. Visible or audible alarm indicates the vicinity of the catheter tip
c. Limitation: confirms catheter is in the right direction, but no information about the correct location
2. Electrocardiogram (ECG) tracings
a. Uses intravascular ECG for real-time tip location; indicated for guidance and positioning
b. Change in P wave indicates the catheter tip
1) As the catheter passes the SA node, P wave increases in voltage, and upward spike indicates RA
c. May be considered as an alternative to chest radiograph and fluoroscopy
d. Disadvantages
1) P wave not present (AF, atrial flutter, marked tachycardia)
2) Close-ended PICCs (e.g., Groshong); valves may not open c onsistently leading to intermittent ECG reading
3. Vascular-positioning system
a. Uses a combination of intravascular ECG and Doppler ultrasound to provide real-time navigation as catheter advances through the vasculature
b. As the catheter tip approaches the heart, the use of an algorithm identifies its location
c. May be considered as an alternative to chest radiograph and fluoroscopy.
C. Light Devices
1. Visible light
a. Designed to find peripheral veins from high-intensity light source
b. Requires darkened room to eliminate competing light sources
c. Area of illumination depends on skin color
2. Transillumination
a. Used when the near-infrared light source is placed against the opposite side of the extremity
b. Hemoglobin absorbs the light and identifies arteries and veins as dark areas on the skin
c. Viewing scope, similar to night vision goggle is used to see the veins
 IX. Flow Control Devices
IX. Flow Control DevicesA. Overview
1. Regulate the administration of parenteral solutions and medications
2. Considerations for appropriate device selection
a. Patient age, condition, and mobility
b. Prescribed therapy and type of VAD
c. Setting in which therapy is delivered
B. Mechanisms of Delivery
1. Volumetric pump
a. Calculates solution delivery by measuring the solution volume as it is displaced into a reservoir attached to the administration set
b. Types of action
1) Syringe: piston withdraws and pushes the solution through the administration set
2) Linear peristaltic: peristaltic fingers compress tubing in a wavelike motion, pushing solution through the administration set
3) Filling and emptying of microreservoirs: filled and emptied in sequence and measured in hundredths of a milliliter
2. Syringe pump: syringe driven by a piston to deliver solutions
a. Rate set to deliver solution continuously, intermittently, or continuously and intermittently simultaneously
b. Rate is controlled by the drive speed of the piston attached to the syringe plunger
c. For patient-controlled analgesia (PCA) or intermittent medication delivery, such as antibiotics
d. Delivery of minute amounts (as little as 0.01 mL/hour) of medications or solutions; ideal for use with infants and for maintaining patency of arterial lines
e. Volume is limited to the size of the syringe used in the device, usually a 60-mL syringe, but can be as small as 5 mL
3. Piston pump: piston action controls the flow of the solution
a. Usually requires a special dedicated administration set
b. Allows rates to be set to deliver fluids continuously, intermittently, or continuously and intermittently simultaneously
c. May operate by battery or electricity; compact and portable
4. Drop sensor: a device used with an infusion device designed to count drops as they fall and thus calculate the volume of solution being administered
a. Confirms only the presence or absence of flow
b. Variation in the drop size may cause flow rate errors
C. Electronic Infusion Devices
1. Programmable device powered by electricity or battery used to regulate infusion rate and volume
2. Controller
a. Electronically controlled drop sensor device that delivers solutions with the aid of gravity; does not exert positive pressure greater than the head height of the infusion container
b. Regulates flow rate by counting the drops and transmitting the rate to the device that controls the tubing pressure, increasing or decreasing the tubing diameter to deliver the rate set on the controller
c. Has alarms that are activated when established flow rates are violated or when resistance is detected; useful for detecting infiltrations
d. Requires solution container be placed approximately 36 inches above the catheter insertion site to overcome venous resistance and operate properly
e. Reduces the potential for “runaways” and empty bottles and for repeated venipunctures associated with gravity feed systems
f. Maintains constant, accurate flow rate without pressure
3. Positive-pressure infusion pump
a. Infusion device that exerts pressure to overcome vascular resistance to administer medications or solutions
b. Average pressure is 10 psi, with up to 15 psi considered to be safe
1) Pumps with pressures >15 to 20 psi should be used with extreme caution
2) Ability to set variable pressure limits must be a consideration in choosing a device for the pediatric population and frail elderly patients
c. Used to deliver high or very low volumes; in high acuity situations and complex therapies
d. Delivers accurately as programmed in accordance with industry standard of ±5%
e. Features vary with device
4. PCA pump
a. PCA is a method of pain control designed to allow the patient the ability to administer bolus doses of an analgesic as needed
b. Ability to deliver doses on demand; responds by delivering or denying the dose as determined by preset limits
c. Mode of therapy
1) Continuous
a) For the patient who needs maximum pain relief without the option of demand dosing
b) Used for epidural narcotic infusions, neonatal infusions, pain-control administration to patients unable to use the demand function
2) Basal
a) Can be accompanied by intermittent doses requested by the patient
b) Designed to achieve pain relief with minimal medication, allowing the patient to remain alert and active without sedation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
