Scope of Neuroscience Nursing Practice
Definitions and Distinguishing Characteristics of Neuroscience Nursing Practice
Definitions
Nursing is defined as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations” (ANA, 2010a, p. 1; ANA, 2010b, p. 10).
Neuroscience nursing is defined as a nursing specialty that addresses the needs and care of individuals with biological, psychological, social, and spiritual alterations as a result of nervous system dysfunction (Webb, 2000). This encompasses all levels of human existence, from basic bodily functions to advanced processes of the human mind. Neuroscience nurses identify and treat human responses to actual or potential health problems related to phenomena affected by nervous system dysfunction. Phenomena addressed within the context of neuroscience nursing practice include: consciousness and cognition, communication, affiliate relationships, mobility, rest and sleep, sensation, elimination, sexuality, self-care, and integrated regulation. Potential recipients of neuroscience nursing care are individuals with nervous system dysfunction, their families and significant others, and the society in which they live.
Distinguishing Characteristics
The American Nurses Association (ANA) identifies the following essential features of nursing practice:
A caring relationship that facilitates health and healing. In neuroscience nursing, this relationship is critically important when individuals are unable to speak for themselves due to an altered level of responsiveness.
Attention to a range of human experiences and responses to health, disease, and illness in the physical and social environments. In neuroscience nursing, this might include assessing the home environment to which a person with quadriplegia will return.
Integration of objective data with knowledge gained from an appreciation of the patient’s or group’s subjective experience. An example is planning an educational program for caregivers of persons with Alzheimer’s disease based on assessment of their needs.
Application of scientific knowledge to diagnosis and treatment through the use of judgment and critical thinking. Neuroscience nurses are adept at critically distinguishing the significance of findings from the neurologic exams they conduct.
Advancement of professional nursing knowledge through scholarly inquiry. For example, neuroscience nurses have increased compliance with seizure medication regimens by evaluating factors that enhance compliance.
Influence on social and public policy to promote social justice. For example, neuroscience nurses have participated in efforts to require seat belt and helmet use in order to prevent neurologic injury.
Assurance of safe, quality, and evidence-based practice. For example, neuroscience nurses incorporate quality measures, such as swallow evaluations, into care of the patient with stroke.
These essential features are applied in neuroscience nursing practice to address the phenomena unique to the specialty.
Specific phenomena defined by the American Association of Neuroscience Nurses (AANN) that comprise the unique domain of neuroscience nursing include:
Consciousness and cognition—The awareness of and interaction with the surrounding environment as well as the higher thought processes; alterations include problems such as coma, memory impairment, and seizures.
Communication—The language interaction with others; alterations include language impairments secondary to the aphasias or dysarthria.
Affiliate relationships—The ability to form and maintain social support relationships; alterations include social isolation and role changes secondary to nervous system disease.
Mobility—The ability to move freely within the environment; alterations include various forms of paralysis.
Rest and sleep—Phenomena necessary for restorative function; alterations include the spectrum of sleep disorders.
Sensation—The ability to sense and distinguish internal and external stimuli; alterations include decreased sensation and pain.
Elimination—Bodily excretion of waste products; alterations include bowel and bladder dysfunction secondary to nervous system disease.
Sexuality—The ability to interact and maintain a sexual relationship; alterations include sexual dysfunction secondary to nervous system disease.
Self-care—The ability to provide for one’s basic needs; alterations include the inability to care for oneself.
Integrated regulation—The interrelationship between the nervous system and other body systems; alterations include loss of regulatory control.
Historical Perspective on Neuroscience Nursing Standards and Evolution of Practice
In the mid-20th century and beyond, advances in medical treatment and healthcare technology led to the evolution of nursing specialties. Specialized education, training, and certification ensued in both traditional and newer areas of clinical practice, including neuroscience nursing. Neuroscience nursing was formalized as a specialty in 1968 with the formation of the American Association of Neurosurgical Nurses (AANN). In 1985, the organization’s name was changed to the American Association of Neuroscience Nurses to better reflect the practice diversity of its members.
A statement of the standards of neurologic and neurosurgical nursing practice was first completed in 1977, and was approved by the executive
committee of the ANA’s division of medical-surgical nursing practice and AANN. A statement of neuroscience nursing’s scope of practice was first completed in 1986 by the AANN Nursing Practice Committee. This document described the parameters of nursing practice for the specialty, identified the population served and practice settings, and distinguished qualifications of nurses in the specialty and the type of care rendered to patients. This description was useful to the neuroscience nurse in defining goals, and to the public for clarifying expectations.
committee of the ANA’s division of medical-surgical nursing practice and AANN. A statement of neuroscience nursing’s scope of practice was first completed in 1986 by the AANN Nursing Practice Committee. This document described the parameters of nursing practice for the specialty, identified the population served and practice settings, and distinguished qualifications of nurses in the specialty and the type of care rendered to patients. This description was useful to the neuroscience nurse in defining goals, and to the public for clarifying expectations.
In 1993, the standards and scope of practice statements were combined into a single document and updated, addressing the expanded options for neuroscience nursing in the 1990s. The third revision, Scope and Standards of Neuroscience Nursing Practice, issued in 2002, reflected practice evolution at the beginning of the new millennium. The borders of nursing practice have grown in recent years, with potential for continued change as healthcare reforms take shape. A renewed emphasis is placed on care of patients across the lifespan and a spectrum of health states rather than focusing on episodes of illness.
Neuroscience nursing practice has evolved along with clinical advances. Previously, neuroscience nursing care focused on symptom management and prevention of secondary complications. Although these approaches continue to be necessary, advances have offered new hope for persons with neurologic dysfunction. In recent decades, care of the patient with multiple sclerosis has evolved from symptomatic care to educating patients about administration of immunomodulating drugs. Neuroscience nurses can now help reduce deficits in stroke patients through the use of thrombolytic therapy and education geared toward early recognition of stroke symptoms. Advances in clinical monitoring, including intracranial pressure monitoring and brain tissue oxygenation monitoring, have allowed neuroscience nurses to become more skilled in applying data about neurologic function to the plan of care. Neuroscience nursing research findings have contributed to improved outcomes for children with seizures and for families of persons with brain tumors.
As neuroscience nursing evolved as a specialty, so did practice opportunities for APRNs. Increased availability of advanced education, combined with the shortage of primary care providers, need to improve quality of care, restricted residency hours, and promotion of cost-effective care, have led to increasing use of advanced practice nurses. The number of APRNs in neuroscience nursing has grown in recent decades, reflecting the complexity and diversity of the field. In 2009, work began on a scope of practice and standards document
for advanced neuroscience nursing practice, which was published in 2010 (Stewart-Amidei et al., 2010). This fourth revision of Neuroscience Nursing: Scope and Standards of Practice is a collaboration of AANN and ANA, reflects an update to the 2002 neuroscience nursing scope and standards resource, and incorporates neuroscience advanced practice registered nursing scope and standards content.
for advanced neuroscience nursing practice, which was published in 2010 (Stewart-Amidei et al., 2010). This fourth revision of Neuroscience Nursing: Scope and Standards of Practice is a collaboration of AANN and ANA, reflects an update to the 2002 neuroscience nursing scope and standards resource, and incorporates neuroscience advanced practice registered nursing scope and standards content.
Neuroscience Nursing’s Scope and Standards of Practice
Description of the Scope of Neuroscience Nursing Practice
The specialty of neuroscience nursing has one scope of practice that encompasses a broad range of nursing practice and settings. This scope of practice statement describes who neuroscience nurses are and how they practice.
A neuroscience nurse is a registered nurse who provides care to individuals at risk for or with actual problems due to neurologic dysfunction, their families, and the communities in which they live. Neuroscience nurses provide care across the lifespan, from birth through death. Major categories of conditions that produce alterations of concern to neuroscience nurses include degenerative diseases (such as multiple sclerosis and Alzheimer’s disease), tumors of the nervous system, neuromuscular diseases (such as myasthenia gravis), traumatic injury to the brain and spine, stroke and other cerebrovascular diseases, seizures, pain, diseases of the spine, movement disorders (such as Parkinson’s disease and dystonia), and developmental problems of the nervous system. Neuroscience nurses also focus on prevention of nervous system dysfunction through health promotion, community education, and research.
No other specialty specifically addresses persons with neurologic dysfunction. The depth and breadth in which individual neuroscience nurses engage in the total scope of neuroscience nursing practice depends on their education, experience, role, and work environment, and is addressed in greater detail later in this document. Neuroscience nursing is a learned specialty built on a core body of knowledge that reflects its dual components of science and art (Bader & Littlejohns, 2010).
Neuroscience nursing requires judgment and skill based on principles of the biological, physical, psychological, behavioral, and social sciences with specific focus on neurologic function. Neuroscience nurses employ critical thinking to integrate objective data with knowledge gained from an assessment of the
subjective experiences of patients. Neuroscience nurses use critical thinking to apply the best available evidence and research data to diagnosis and treatment. Neuroscience nurses continually evaluate quality and effectiveness of nursing practice and seek to optimize outcomes.
subjective experiences of patients. Neuroscience nurses use critical thinking to apply the best available evidence and research data to diagnosis and treatment. Neuroscience nurses continually evaluate quality and effectiveness of nursing practice and seek to optimize outcomes.
The Science of Neuroscience Nursing
The science of neuroscience nursing is based on an analytical framework of critical thinking comprised of assessment, diagnosis, identification of outcomes, planning, implementation, and evaluation, collectively known as the nursing process. These steps serve as the foundation of clinical decision-making and support evidence-based practice. Wherever they practice, neuroscience nurses use the nursing process and other types of critical thinking to respond to the needs of the populations they serve, and use strategies that support optimal outcomes most appropriate to the patient or situation, being mindful of resource utilization.
Neuroscience nurses as scientists rely on evidence to guide their policies and practices, but also as a way of quantifying the nurses’ impact on the health outcomes of patients. An example of AANN leadership in this area is the development of the AANN Clinical Practice Guidelines series, which provides evidence-based directives for nurses caring for patients with problems such as traumatic brain injury or brain tumor.
Neuroscience nurses also generate new knowledge in their field through systematic research. In 1993, AANN established the Neuroscience Nursing Foundation, with the primary purpose of advancing the science and practice of neuroscience nursing. In 2011, updated strategies were proposed to meet this purpose (Di Iorio et al., 2011):
Promote evidence-based practice to inform clinical decision-making
Select strong research designs based on current research practices
Develop and test nursing interventions
Test theoretical or conceptual models for neuroscience nursing practice
Build programs of research involving interdisciplinary teams
Research priorities identified include acute care outcomes, health promotion, end-of-life nursing care, quality-of-life improvements, and special population needs. Research in these areas is necessary to inform, distinguish, and advance neuroscience nursing practice.
The Art of Neuroscience Nursing
The art of neuroscience nursing is based on caring and respect for human dignity. A compassionate approach to patient care carries a mandate to provide that care competently. Competent care is provided and accomplished through both independent practice and partnerships. Collaboration may be with other colleagues or with the individuals seeking support or assistance with their healthcare needs. Central to neuroscience nursing practice is the art of caring, which is represented in the personal relationship that the nurse enters with the patient. The art of caring goes beyond the emotional connections of humans to the ability to respond to the human aspects of health and illness within the critical moment to promote healing within the context of social justice (Watson, 2008).
The art of neuroscience nursing embraces dynamic processes that affect the human person, including, for example, spirituality, healing, empathy, mutual respect, and compassion. These intangible aspects foster health. Neuroscience nursing embraces healing. Healing is fostered by compassion, helping, listening, mentoring, coaching, teaching, exploring, being present, supporting, touching, intuition, empathy, service, cultural competence, tolerance, acceptance, nurturing, mutually creating, and conflict resolution.
Neuroscience nursing focuses on the promotion and maintenance of health and the prevention or resolution of disease, illness, or disability. The nursing needs of human beings are identified from a holistic perspective and are met in the context of a culturally sensitive, caring, personal relationship. Neuroscience nursing includes the diagnosis and treatment of human responses to actual or potential health problems. Neuroscience nurses employ practices that are restorative, supportive, and promotive in nature.
Restorative practices modify the impact of neurologic illness or disease.
Supportive practices are oriented toward modification of relationships or the environment to support health.
Promotive practices mobilize healthy patterns of living, foster personal and family development, and support self-defined goals of individuals, families, communities, and populations.
Development and Function of Nursing Standards
The standards of neuroscience nursing practice are authoritative statements of the duties that neuroscience nurses—regardless of role, population, or
subspecialty served—are expected to competently perform (adapted from ANA, 2010a, p. 2). The standards published herein may be utilized as evidence of a legal standard of care and govern neuroscience nurses practicing within the role, population, and specialty governed by this document. The standards are subject to change with the dynamics of the neuroscience nursing specialty; as new patterns of professional practice are developed and accepted by neuroscience nurses, the education community, and the public; and as changes in societal trends occur. “Standards are subject to formal, periodic review and revision” (ANA, 2010a, p. 31).
subspecialty served—are expected to competently perform (adapted from ANA, 2010a, p. 2). The standards published herein may be utilized as evidence of a legal standard of care and govern neuroscience nurses practicing within the role, population, and specialty governed by this document. The standards are subject to change with the dynamics of the neuroscience nursing specialty; as new patterns of professional practice are developed and accepted by neuroscience nurses, the education community, and the public; and as changes in societal trends occur. “Standards are subject to formal, periodic review and revision” (ANA, 2010a, p. 31).
This document includes 16 standards statements that provide the neuroscience nurse with a framework for outlining an expansive scope of practice. The language is intentionally broad and serves to paint an overall picture of practice. The standards statements become more effective, however, when viewed as a comprehensive and refined listing of expectations essential to practice without further development and explication. The roles and activities in which the neuroscience nurse is involved may be specific to the setting, and directed by state, institutional, or group practice requirements. Standard statements optimally inform nursing practice or the recipients of nursing care when tailored to the specifics of the focus or setting (ANA, 2010a).
Each standard statement is accompanied by several basic competencies. The competency statements in turn may be further specified according to the practice setting. Competencies are specific, measurable elements that interpret, explain, and facilitate practical use of a standard (ANA, 2010a). The competencies may be evidence of compliance with the individual standard but are not exhaustive, and depend on the circumstances. For example, the nurse may not be able to develop the plan of care (Standard 4, Planning) with or communicate it to the unresponsive patient who has no identified family caregiver.
Competencies may be used by neuroscience nursing professionals to appraise professional performance and identify content for academic and continuing education curricula. Neuroscience nurses can also use the competencies to inform others as to practice expectations.
The Nursing Process
Neuroscience nurses use the nursing process to deliver care. The nursing process is often conceptualized as having linear direction from assessment to diagnosis, outcomes identification, planning, implementation, and evaluation. However, these steps are often necessarily interrelated, as one step may inform another (Figure 1; ANA, 2010a).
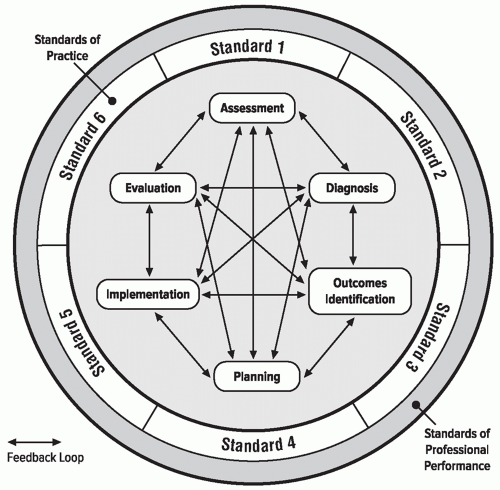 FIGURE 1. The Relationship of the Nursing Process to Practice Standards (ANA, 2010a). |
The Neuroscience Nursing Standards of Practice coincide with the steps of the nursing process. The nursing process begins with assessment, with specific attention focused on neurologic assessment. Data gathered from the neurologic assessment are used to plan and implement nursing interventions specific to the patient’s neurologic dysfunction. Interventions may support bodily functions and promote healing and recovery of the acutely ill; enhance adaptation to persistent neurologic deficits for the chronically ill; facilitate patient, family, and significant other coping; and teach patients, families, and significant others about disease processes, adaptation techniques, and therapies. The neuroscience nurse evaluates the outcomes of nursing care on an ongoing basis, and revises the plan as necessary. Further, application of clinically relevant research
promotes evidence-based care and development of creative therapeutic nursing interventions to improve outcomes for patients with neurologic dysfunction.
promotes evidence-based care and development of creative therapeutic nursing interventions to improve outcomes for patients with neurologic dysfunction.
Ethical principles are applied in any care rendered. Similarly, the Neuroscience Nursing Standards of Professional Performance relate to how the professional nurse adheres to the Neuroscience Nursing Standards of Practice, completes the nursing process, and addresses other practice issues and concerns (ANA, 2010a).
Tenets of Neuroscience Nursing Practice
Five tenets characterize contemporary neuroscience nursing practice, and are reflective of nursing practice as a whole:
1. Neuroscience nursing practice is individualized.
Neuroscience nursing practice respects diversity and is individualized to meet the unique needs of the patient. The patient is defined as the individual with or at risk for neurologic dysfunction, that individual’s family, or a group, community, or population who is the focus of attention and to whom the neuroscience nurse is providing services as sanctioned by the state regulatory bodies. For example, the neuroscience nurse recognizes that each person with a brain tumor or stroke will present different signs, and care must be individualized according to identified needs.
2. Neuroscience nurses coordinate care by establishing partnerships.
Neuroscience registered nurses and APRNs establish partnerships with persons, families, communities, support systems, and other providers, utilizing in-person and electronic communication methods, to reach a shared goal of delivering health care. Collaborative, interprofessional team planning is based on recognition of each discipline’s value and contributions, mutual trust, respect, open discussion, and shared decision-making. Neuroscience nurses frequently partner with other disciplines, such as physical therapy, occupational therapy, and speech therapy, to provide optimum care. Care may also be coordinated with other specialties, including pediatrics, psychiatry, or geriatrics. Knowledge gains in the genetics and immunology fields also require that neuroscience nurses work with these specialists.
3. Caring is central to the practice of neuroscience nursing.
Professional nursing promotes healing and health in a way that builds a relationship between the neuroscience nurse and patients (adapted from Watson, 2008). “Caring is a conscious judgment that manifests itself in concrete acts, interpersonally, verbally, and non-verbally” (Gallagher-Lepak & Kubsch, 2009, p. 171). Although caring for individuals, families, and populations is the key focus of neuroscience nursing, neuroscience registered nurses and APRNs additionally promote self-care, as well as care of the environment and society (Hagerty, Lynch-Sauer, Patusky, & Bouwsema, 1993). Neuroscience nurses communicate caring through touch, verbal communication, and their non-verbal behaviors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
