Rh Incompatibility and ABO Incompatibility
QUICK LOOK AT THE CHAPTER AHEAD
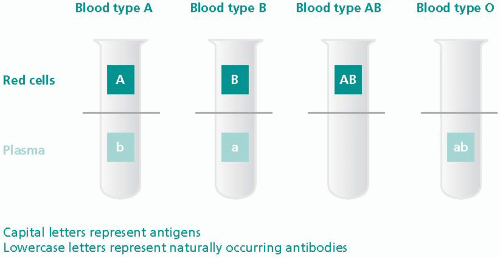
In the United States the population with Rh-negative type blood [missing the Rh (D) factor] is 15% in white couples and 10% in African-American couples; it is rarely found in Asian couples. This hemolytic disease is caused by the excessive destruction of red blood cells in the newborn and is caused by maternal antigens responding to Rh or ABO blood incompatibilities. Hemolytic disorders occur when the blood groups of the mother and the fetus differ. The most common of these are Rh factor and ABO incompatibilities.
Maternal antibodies are present naturally (blood groups O, A, B, and AB) or form in response to an antigen from the fetal blood (Rh-positive factor) crossing the placenta and entering the maternal circulation. The maternal antibodies cross the placenta, causing hemolysis (destruction) of the fetal red blood cells, resulting in hyperbilirubinemia and jaundice. This disease can have severe effects on the fetus, whereas there are little or no risks to the mother. As early as the 1900s, severe fetal hemolytic disease was described in the literature, but the exact problem or cause was not known until the discovery of the Rh factor in 1940. This disease has been decreasing in the United States for the last 30 years due to the availability of Rh antibody prevention. In 1969 Rh (anti-D) globulin became commercially available (RhoGAM), and the ability to prevent Rh sensitization occurred. RhoGAM prevents sensitization by clearing the fetal cells from the maternal circulation and depressing the mothers’ immune response.
Rh incompatibility is defined as a sensitization that occurs when an Rh-negative (blood type) mother delivers an Rh-positive (blood type) baby. This sensitization occurs when fetal blood (Rh positive) enters the maternal circulation (Rh negative) and stimulates the formation of antibodies in the mother’s blood (Figure 14-1). Once the formation of antibodies occurs (in the mother’s blood), these antibodies have the capability to cross the placental barrier into the fetal circulation and attack (destroy) fetal red blood cells. Rh-negative blood lacks the Rh (D) antigen as compared with Rh-positive blood. Because this antigen only exists in someone who is Rh positive, problems arise during pregnancy when a woman with Rh-negative blood is pregnant with a fetus with Rh-positive blood.
 Rh incompatibility is defined as a sensitization that occurs when an Rh-negative (blood type) mother delivers an Rh-positive (blood type) baby.
Rh incompatibility is defined as a sensitization that occurs when an Rh-negative (blood type) mother delivers an Rh-positive (blood type) baby.Although there is no direct connection between maternal blood and fetal blood in the placenta, this blood is separated by a single cell membrane. Anytime during pregnancy there is the possibility that a (small leak) tear in this membrane could occur. It only takes a very small amount of Rh-positive fetal blood to enter the maternal bloodstream and actively stimulate maternal antibodies to form against the Rh-positive blood. Usually, the mixing of fetal blood cells and maternal blood cells takes place at the time of placental separation (third stage of labor). However, the danger exists during pregnancy as well as after delivery (28 weeks’ gestation and 3 days after delivery).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree