Respiratory care
Diseases
Acute respiratory distress syndrome
Acute respiratory distress syndrome (ARDS), also called shock lung or adult respiratory distress syndrome, results from increased permeability of the alveolocapillary membrane. Fluid accumulates in the lung interstitium, alveolar spaces, and small airways, causing the lung to stiffen. Effective ventilation is thus impaired, prohibiting adequate oxygenation of pulmonary capillary blood. Severe ARDS can cause intractable and fatal hypoxemia. However, patients who recover may have little or no permanent lung damage.
ARDS results from a variety of respiratory and nonrespiratory insults, such as:
aspiration of gastric contents
massive blood transfusions
drug overdose (barbiturates, glutethimide, or opioids)
gestational hypertension
hydrocarbon and paraquat ingestion
increased intracranial pressure
microemboli (fat or air emboli or disseminated intravascular coagulation)
near drowning
oxygen toxicity
pancreatitis, uremia, or miliary tuberculosis (rare)
prolonged heart bypass surgery
radiation therapy
sepsis (primarily gram-negative)
shock
smoke or chemical inhalation (nitrous oxide, chlorine, or ammonia)
trauma
viral, bacterial, or fungal pneumonia
leukemia
thrombotic thrombocytopenic purpura.
 What happens in ARDS
What happens in ARDSShock, sepsis, and trauma are the most common causes of acute respiratory distress syndrome (ARDS). Trauma-related factors, such as fat emboli, pulmonary contusions, and multiple transfusions, may increase the likelihood that microemboli will develop.
Phase 1
In phase 1, injury reduces normal blood flow to the lungs. Platelets aggregate and release histamine (H), serotonin (S), and bradykinin (B).
 |
Phase 2
In phase 2, those substances—especially histamine—inflame and damage the alveolocapillary membrane, increasing capillary permeability. Fluids then shift into the interstitial space.
 |
Phase 3
In phase 3, as capillary permeability increases, proteins and fluids leak out, increasing interstitial osmotic pressure and causing pulmonary edema.
 |
Phase 4
In phase 4, decreased blood flow and fluids in the alveoli damage surfactant and impair the cell’s ability to produce more. As a result, alveoli collapse, impeding gas exchange and decreasing lung compliance.
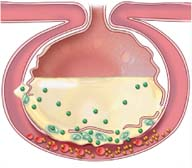 |
Phase 5
In phase 5, sufficient oxygen (O2) can’t cross the alveolocapillary membrane, but carbon dioxide (CO2) can and is lost with every exhalation. O2 and CO2 levels decrease in the blood.
 |
Signs and symptoms
Apprehension
Crackles
Dyspnea
Hypoxemia
Intercostal and suprasternal retractions
Cough
Confusion
Hypotension
Mental sluggishness
Motor dysfunction
Rapid, shallow breathing
Restlessness
Rhonchi
Tachycardia
Treatment
Correction of the underlying cause
Prevention of progression and the potentially fatal complications of hypoxemia and respiratory acidosis
Administration of humidified oxygen with continuous positive airway pressure
Possibly ventilatory support with intubation, volume ventilation, and positive end-expiratory pressure (PEEP)
Fluid restriction
Diuretics
Correction of electrolyte and acid-base abnormalities
Treatment to reverse severe metabolic acidosis with sodium bicarbonate may be necessary, although in severe cases, this may worsen the acidosis if carbon dioxide can’t be cleared adequately
Administration of fluids and vasopressors to maintain blood pressure
Antibiotic administration
Administration of prostaglandins
Nursing considerations
Frequently assess the patient’s respiratory status.
Check for clear, frothy sputum, which may indicate pulmonary edema.
Maintain a patent airway.
Closely monitor heart rate and blood pressure. Watch for arrhythmias that may result from hypoxemia, acid-base disturbances, or electrolyte imbalance.
Monitor serum electrolytes and correct imbalances.
Measure intake and output; weigh the patient daily.
Check ventilator settings frequently.
Monitor arterial blood gas studies and pulse oximetry.
Give sedatives, as needed, to reduce restlessness.
If the patient is receiving PEEP, check for hypotension, tachycardia, and decreased urine output.
Give tube feedings and parenteral nutrition, as ordered.
Perform passive range-of-motion exercises or help the patient perform active exercises, if possible, to help maintain joint mobility.
Provide meticulous skin care to prevent skin breakdown.
Plan patient care to allow periods of adequate rest.
Provide emotional support.
Place in prone position to improve chest wall compliance and drainage of bronchial secretions.
 Teaching about ARDS
Teaching about ARDS
Explain the disorder to the patient and his family. Tell them which signs and symptoms may occur, and review necessary treatment.
Orient the patient and his family to the unit and health care facility surroundings. Explain equipment needed to provide adequate oxygenation.
Tell a recuperating patient that recovery takes time and that he’ll feel weak for a while. Urge him to share his concerns with the staff.
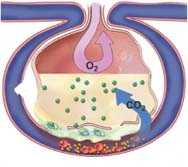
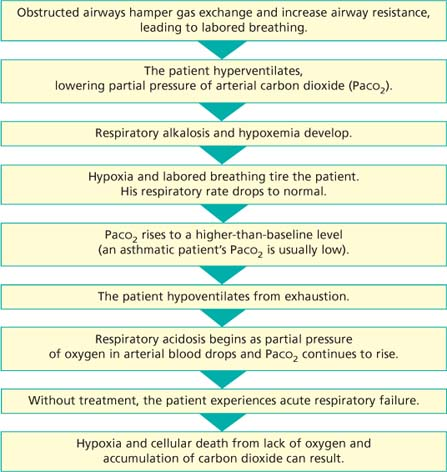
Asthma
Asthma is a reversible lung disease characterized by obstruction or narrowing of the airways, which are typically inflamed and hyperresponsive to a variety of stimuli. It may resolve spontaneously or with treatment. Its symptoms range from mild wheezing and dyspnea to life-threatening respiratory failure. Symptoms of bronchial airway obstruction may persist between acute episodes.
Signs and symptoms
Chest tightness
Coughing with thick, clear, or yellow mucus
Cyanosis (late sign)
Diaphoresis
Nasal flaring
Pursed-lip breathing
Sudden dyspnea
Tachycardia
Tachypnea
Use of accessory muscles for breathing
Wheezing accompanied by coarse rhonchi
Determining asthma’s severity
Current guidelines for classifying asthma severity for patients age 12 and older are listed here.
Intermittent
Attacks no more than twice per week
Nighttime attacks no more than twice per month
Rescue inhaler used no more than twice per week
Asthma doesn’t interfere with daily activities
Normal FEV1 (forced expiratory volume in 1 second)
Mild persistent
Attacks more than twice per week but not every day
Nighttime attacks three to four nights per month
Rescue inhaler used more than 2 days per week
Asthma minorly interferes with daily activities
FEV1 greater than 80% of normal lung function most of the time
Moderate persistent
Daily attacks
Nighttime attacks more than once per week
Rescue inhaler used daily
Asthma moderately interferes with daily activities
FEV1 greater than 60% but less than 80%
Severe persistent
Continual, severe daily attacks
nighttime attacks daily
Rescue inhaler used multiple times per day
Asthma severely interferes with daily activities
FEV1 less than 60%
Treatment
Identification and avoidance of precipitating factors
Desensitization to specific antigens
Low-flow humidified oxygen
Inhaled steroids such as triamcinolone acetonide (Azmacort)
Leukotriene inhibitors such as montelukast (Singulair)
Long-acting bronchodilators such as formoterol (Foradil Aerolizer)
Mast cell stabilizers, such as cromolyn sodium (Intal) or nedocromil (Alocril)
Aminophyllin (Truphylline) or theophylline (Slo-bid)
Short-acting bronchodilators, such as albuterol (Proventil) or levalbuterol (Xopenex)
Oral or I.V. corticosteroids
Mechanical ventilation
Nebulized atropine
Omalizumab (Xolair)
Bronchial thermoplasty
Nursing considerations
Administer the prescribed treatments and assess the patient’s response.
Place the patient in high Fowler’s position.
Monitor the patient’s vital signs, especially respiratory status.
Administer prescribed humidified oxygen.
Anticipate intubation and mechanical ventilation if the patient fails to maintain adequate oxygenation.
Monitor serum theophylline levels.
Observe for signs and symptoms of theophylline toxicity (vomiting, diarrhea, and headache).
Perform postural drainage and chest percussion.
Provide emotional support.
Anticipate the need for bronchoscopy or bronchial lavage when a lobe or larger area collapses.
Review arterial blood gas levels, pulmonary function test results, and SaO2 readings.
 Teaching about asthma
Teaching about asthma
Teach the patient to avoid known allergens and irritants.
Describe prescribed drugs, including their names, dosages, actions, adverse effects, and special instructions.
Teach the patient how to use a metered-dose inhaler.
If the patient has moderate to severe asthma, explain how to use a peak flowmeter and to keep a record of peak flow readings.
Tell the patient to seek immediate medical attention if he develops a fever above 100º F (37.8º C), chest pain, shortness of breath without coughing or exercising, or uncontrollable coughing.
Teach diaphragmatic and pursed-lip breathing and effective coughing techniques.
Urge the patient to drink at least 3 qt (3 L) of fluids daily to help loosen secretions and maintain hydration.
Explain the importance of seeking immediate medical attention if the peak flow drops suddenly.
Cystic fibrosis
Cystic fibrosis is a generalized dysfunction of the exocrine glands that affects multiple organ systems. Transmitted as an autosomal recessive trait, it’s the most common fatal genetic disease in white children. Affecting about 30,000 U.S. children and adults, cystic fibrosis is most common in Whites (1 in 3,300 births) and less common in Blacks (1 in 15,300 births), Native Americans, and Asians. It occurs equally in both sexes.
Most cases of cystic fibrosis arise from a mutation that affects the genetic coding for a single amino acid, resulting in a protein that doesn’t function properly. The abnormal protein resembles other transmembrane transport proteins. It lacks phenylalanine (an essential amino acid) that’s usually produced by normal genes. This abnormal protein may interfere with chloride transport by preventing adenosine triphosphate from binding to the protein and interfering with activation by protein kinase. The lack of essential amino acids leads to dehydration and mucosal thickening in the respiratory and intestinal tracts.
Signs and symptoms
Excessive salty taste to skin
Barrel chest
Clubbing of fingers and toes
Crackles and wheezing
Cyanosis
Dyspnea
Failure to thrive, poor weight gain, distended abdomen
Frequent bouts of pneumonia
Frequent bulky and foul-smelling stools (steatorrhea)
Frequent upper respiratory tract infections
Intestinal obstruction (meconium ileus in infants)
Persistent cough
Thick secretions
Treatment
Diet with increased fat and sodium
Salt supplements
Pancreatic enzyme replacement
Breathing exercises, chest percussion, and postural drainage
Inhaled beta-adrenergics
Broad-spectrum antimicrobials
Sodium channel blockers
Heart or lung transplant
Dornase alfa (Pulmozyme)
High-frequency chest compression vest
Oxygen therapy as needed
Bronchodilators
Mucolytic aerosols
Corticosteroids
Nursing considerations
Give medications as ordered. Administer pancreatic enzymes with meals and snacks.
Perform chest physiotherapy, including postural drainage and chest percussion several times per day.
Administer oxygen therapy as ordered. Check levels of arterial oxygen saturation using pulse oximetry.
Provide a well-balanced, high-calorie, high-protein diet. Include plenty of fats.
Administer vitamin A, D, E, and K supplements, if laboratory analysis indicates deficiencies.
Make sure the patient receives plenty of liquids to prevent dehydration, especially in warm weather.
Provide exercise and activity periods.
Encourage deep-breathing exercises.
Provide the young child with play periods and enlist the help of physical and play therapists.
Provide emotional support to the patient and parents. Encourage them to discuss their fears and concerns and answer questions as honestly as possible.
Include the family in all phases of patient care.
 Teaching about cystic fibrosis
Teaching about cystic fibrosis
Tell the patient and his family about the disease and thoroughly explain all treatments. Make sure they know about tests to determine whether family members carry the cystic fibrosis gene.
Explain aerosol therapy, including intermittent nebulizer treatments before postural drainage. Tell the patient and his family that these treatments help loosen secretions and dilate bronchi.
Instruct family members in proper methods of chest physiotherapy.
Teach the patient and his family signs of infection and sudden changes they should report to the physician, including increased coughing, decreased appetite, sputum that thickens or contains blood, shortness of breath, and chest pain.
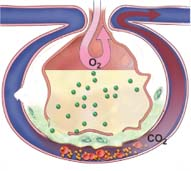
Emphysema
Emphysema is a form of chronic obstructive pulmonary disease characterized by the abnormal, permanent enlargement of the acini accompanied by destruction of alveolar walls without fibrosis. Obstruction results from tissue changes rather than mucus production, which occurs in asthma and chronic bronchitis. The distinguishing characteristic of emphysema is airflow limitation caused by thick elastic recoil in the lungs.
Senile emphysema results from degenerative changes that cause stretching without destruction of the smooth muscle. Connective tissue usually isn’t affected.
Signs and symptoms
Accessory muscle use for breathing
Anorexia with resultant weight loss
Barrel chest
Chronic cough with or without sputum production
Clubbed fingers and toes
Crackles and wheezing on inspiration
Decreased breath sounds
Decreased chest expansion
Decreased tactile fremitus
Dyspnea on exertion
Hyperresonance
Malaise
Mental status changes, if carbon dioxide retention worsens
Prolonged expiration and grunting
Tachypnea
Treatment
Avoidance of tobacco smoke and air pollution
Bronchodilators, such as beta-adrenergic blockers and albuterol (Proventil), aminophylline
Antibiotics
Flu vaccine to prevent influenza
Pneumovax to prevent pneumococcal pneumonia
Adequate hydration
Chest physiotherapy
Oxygen therapy
Mucolytics
Aerosolized or systemic corticosteroids
Lung volume reduction surgery
Lung transplantation
Nursing considerations
Provide incentive spirometry and encourage deep breathing.
Administer oxygen.
Give antibiotics as ordered.
Perform chest physiotherapy including postural drainage and chest percussion as ordered.
Make sure that the patient receives adequate hydration.
Provide high-calorie, protein-rich foods to promote health and healing.
Offer small, frequent meals to conserve energy.
Alternate rest and activity periods.
 Teaching about emphysema
Teaching about emphysema
Explain the disease process and its treatments.
Urge the patient to avoid inhaled irritants, such as cigarette smoke, automobile exhaust fumes, aerosol sprays, and industrial pollutants.
Advise the patient to avoid crowds and people with infections and to obtain pneumonia and annual flu vaccines.
Warn the patient that exposure to blasts of cold air may trigger bronchospasm; suggest that he avoid cold, windy weather and that he cover his mouth and nose with a scarf or mask if he must go outside in such conditions.
Explain all drugs, including their indications, dosages, adverse effects, and special considerations.
Inform the patient about signs and symptoms that suggest ruptured alveolar blebs and bullae, and urge him to seek immediate medical attention if they occur.
Demonstrate how to use a metered-dose inhaler.
Teach the safe use of home oxygen therapy.
Teach the patient and his family how to perform postural drainage and chest physiotherapy.
Discuss the importance of drinking plenty of fluids to liquefy secretions.
For family members of a patient with familial emphysema, recommend a blood test for alpha1-antitrypsin. If a deficiency is found, stress the importance of not smoking and avoiding areas (if possible) where smoking is permitted.
Promote smoking cessation, if appropriate.
Lung cancer
Even though it’s largely preventable, lung cancer has long been the most common cause of cancer death in men and is an increasing cause of cancer death in women. Lung cancer usually develops within the wall or epithelium of the bronchial tree. The most common type is non-small-cell cancer, which includes epidermoid (squamous cell) carcinoma, adenocarcinoma, and large cell (anaplastic) carcinoma. Less common is small-cell lung cancer. prognosis varies with the extent of metastasis at the time of diagnosis and the cell type growth rate.
Signs and symptoms
Cough, hoarseness, wheezing, dyspnea, hemoptysis, and chest pain
Bone and joint pain
Clubbing of fingers
Cushing’s syndrome
Fever, weight loss, weakness, and anorexia
Hemoptysis, atelectasis, pneumonitis, and dyspnea
Hypercalcemia
Jugular vein distention and facial, neck, and chest edema
Piercing chest pain, increasing dyspnea, and severe arm pain
Pleural friction rub
Rust-colored or purulent sputum
Shoulder pain and unilateral paralysis of diaphragm
Wheezing
Treatment
Lobectomy, wedge resection, or pneumonectomy
Video-assisted chest surgery
Laser surgery
Radiation
Chemotherapy
Cisplastin and p53 gene therapy
Staging lung cancer
Using the TNM (tumor, node, metastasis) classification system, the American Joint Committee on Cancer stages lung cancer as follows.
Primary tumor
TX—primary tumor can’t be assessed, or malignant tumor cells are detected in sputum or bronchial washings but undetected by X-ray or bronchoscopy
T0—no evidence of primary tumor
Tis—carcinoma in situ
T1—tumor 3 cm or less in greatest dimension, surrounded by normal lung or visceral pleura; no bronchoscopic evidence of cancer closer to the center of the body than the lobar bronchus
T1a—tumor 2 cm or less
T1b—tumor greater than 2 cm but less than or equal to 3 cm
T2—tumor larger than 3 cm but less than or equal to 7 cm; one that involves the main bronchus and is 2 cm or more from the carina; one that invades the visceral pleura; or one that’s accompanied by atelectasis or obstructive pneumonitis that extends to the hilar region but doesn’t involve the entire lung
T2a—tumor greater than 3 cm but less than or equal to 5 cm
T2b—tumor greater than 5 cm but less than or equal to 7 cm
T3—tumor greater than 7 cm or of any size that extends into neighboring structures, such as the chest wall, diaphragm, or mediastinal pleura; tumor in the main bronchus that doesn’t involve but is less than 2 cm from the carina; or tumor that’s accompanied by atelectasis or obstructive pneumonitis of the entire lung
T4—tumor of any size that invades the mediastinum, heart, great vessels, trachea, esophagus, vertebral body, or carina; or tumor with malignant pleural effusion
Regional lymph nodes
NX—regional lymph nodes can’t be assessed
N0—no detectable metastasis to lymph nodes
N1—metastasis to the ipsilateral peribronchial or hilar lymph nodes or both
N2—metastasis to the ipsilateral mediastinal or subcarinal lymph nodes or both
N3—metastasis to the contralateral mediastinal or hilar lymph nodes, the ipsilateral or contralateral scalene lymph nodes, or the supraclavicular lymph nodes
Distant metastasis
M0—no evidence of distant metastasis
M1—distant metastasis
M1a—tumor with malignant pleural or pericardial effusion or pleural nodules; separate tumor nodules in contralateral lobe
M1b—metastasis in extrathoracic organs
Staging categories
Lung cancer progresses from mild to severe as follows:
Occult carcinoma—TX, N0, M0
Stage 0—Tis, N0, M0
Stage Ia—T1, N0, M0
Stage Ib—T2, N0, M0
Stage IIa—T1, N, M0
Stage IIb—T2, N1, M0; T3, N0, M0
Stage IIIa—T1, N2, M0; T2, N2, M0; T3, N1, M0; T3, N2, M0
Stage IIIb—any T, N3, M0; T4, any N, M0
Stage IV—any T, any N, M1
Nursing considerations
Give comprehensive, supportive care and provide patient teaching to minimize complications and speed the patient’s recovery from surgery,
radiation, and chemotherapy.
Urge the patient to voice his concerns and schedule time to answer his questions. Be sure to explain procedures before performing them.
After thoracic surgery
Maintain a patent airway and monitor chest tubes.
Check vital signs and watch for and report abnormal respirations and other changes.
Suction the patient as needed and encourage him to begin deep breathing and coughing as soon as possible. Check secretions often. Initially sputum will appear thick and dark with blood, but it should become thinner and grayish-yellow within 1 day.
Monitor and document amount and color of closed chest drainage. Keep chest tubes patent and draining effectively. Watch for fluctuation in the water seal chamber on inspiration and expiration, indicating that the chest tube remains patent. Watch for air leaks and report them immediately. Position the patient on the surgical side to promote drainage and lung reexpansion.
Monitor intake and output and maintain hydration.
Encourage early ambulation.
 Teaching about lung cancer
Teaching about lung cancer
Preoperatively, teach the patient about postoperative procedures and equipment. Teach him how to cough and breathe deeply from the diaphragm and how to perform range-of-motion exercises. Reassure him that analgesics and proper positioning will help to control postoperative pain.
If the patient will have chemotherapy or radiation therapy, make sure he understands the adverse effects that occur and measures to prevent or reduce their severity.
To help prevent lung cancer, teach high-risk patients to stop smoking. Refer smokers who want to quit to
the local branch of the American Cancer Society or American Lung Association. Explain that nicotine gum or a nicotine patch and an antidepressant may be prescribed in combination with educational and support groups.
Pneumonia
Pneumonia is an acute infection of the lung parenchyma that commonly impairs gas exchange. The prognosis is generally good for people who have normal lungs and adequate host defenses before the onset of pneumonia; however, pneumonia is the sixth leading cause of death in the United States.
Pneumonia can be classified by microbiologic etiology, location, or type.
Microbiologic etiology—Pneumonia can be viral, bacterial, fungal, protozoan, mycobacterial, mycoplasmal, or rickettsial in origin.
Location—Bronchopneumonia involves distal airways and alveoli; lobular pneumonia, part of a lobe; and lobar pneumonia, an entire lobe.
Type—Pneumonia may be described by the setting in which it was acquired. Community-acquired pneumonia is the most common type and occurs outside the health care setting. Hospital-acquired pneumonia (HAC) occurs in the health care setting. Ventilator-associated pneumonia is a type of HAC occurring in ventilator patients. Health care–associated pneumonia occurs in other health care settings, such as nursing homes. Aspiration pneumonia refers to pneumonia that results from a foreign substance, such as emesis, entering the lungs.
Predisposing factors for bacterial and viral pneumonia include:
abdominal and thoracic surgery
aspiration
atelectasis
cancer (particularly lung cancer)
chronic illness and debilitation
common colds or other viral respiratory infections
exposure to noxious gases
immunosuppressive therapy
influenza
malnutrition
smoking
tracheostomy.
Predisposing factors for aspiration pneumonia include:
artificial airway use
debilitation
decreased level of consciousness
impaired gag reflex
nasogastric (NG) tube feedings
advanced age
poor oral hygiene
positioning during and after eating or feeding.
Signs and symptoms
Coughing
Crackles and decreased breath sounds
Dyspnea
Fatigue
Fever
Headache
Pleuritic chest pain
Rapid, shallow breathing
Shaking chills
Shortness of breath
Sputum production
Sweating
Decreased pulse oximetry reading
Distinguishing sources of pneumonia
The characteristics and prognosis of different types of pneumonia vary.
| Type | Characteristics |
|---|---|
| Viral | |
| Influenza |
|
| Adenovirus |
|
| Respiratory syncytial virus |
|
| Measles (rubeola) |
|
| Chickenpox (varicella pneumonia) |
|
| Cytomegalo-virus |
|
| Bacterial | |
| Strepto-coccus | |
| |
| Klebsiella |
|
| Staphylo-coccus |
|
| Aspiration | |
| Aspiration of gastric or oropharyn-geal contents into trachea and lungs |
|
Treatment
Antimicrobial therapy that varies with the causative agent (should be reevaluated early in the course of treatment)
Humidified oxygen therapy for hypoxemia
Mechanical ventilation for respiratory failure
High-calorie diet and adequate fluid intake
Bed rest
Analgesics to relieve pleuritic chest pain
Positive end-expiratory pressure to facilitate adequate oxygenation for patients with severe pneumonia who are on mechanical ventilation
Administration of bronchodilators
Administration of corticosteroids
Nursing considerations
Maintain a patent airway and adequate oxygenation. Monitor pulse oximetry. Measure arterial blood gas levels and administer supplemental oxygen as indicated.
Teach the patient how to cough and perform deep-breathing exercises.
If the patient requires endotracheal intubation or tracheostomy, provide thorough respiratory care. Suction the patient as needed, using sterile technique.
Obtain sputum specimens as ordered.
Administer antibiotics as ordered and pain medication as needed; record the patient’s response to medications.
Administer I.V. fluids and electrolyte replacement therapy as ordered.
Maintain adequate nutrition and ask the dietary department to provide a high-calorie, high-protein diet consisting of soft, easy-to-eat foods.
Provide a quiet, calm environment for the patient, with frequent rest periods.
Provide emotional support, especially if respiratory failure occurs.
 Teaching about pneumonia
Teaching about pneumonia
Explain the disease process and the treatment plan.
Teach the patient how to cough and perform deep-breathing exercises to clear secretions; encourage him to do so often.
Give emotional support by explaining all procedures (especially intubation and suctioning) to the patient and his family.
To control the spread of infection, tell the patient to sneeze and cough into a disposable tissue; tape a lined bag to the side of the bed for used tissues.
Teach the patient strategies to prevent pneumonia:
Advise against using antibiotics indiscriminately during minor viral infections because doing so may encourage upper airway colonization by antibiotic-resistant bacteria.
Encourage pneumonia and annual flu vaccination for high-risk patients, such as those with chronic obstructive pulmonary disease, chronic heart disease, or sickle cell disease.
Urge all bedridden and postoperative patients to perform deep-breathing and coughing exercises often. Tell caregivers to reposition such patients frequently to promote full aeration and drainage of secretions. Encourage early ambulation in postoperative patients.
Urge patients to avoid irritants that stimulate secretions, such as cigarette smoke, dust, and environmental pollution.
Pulmonary edema
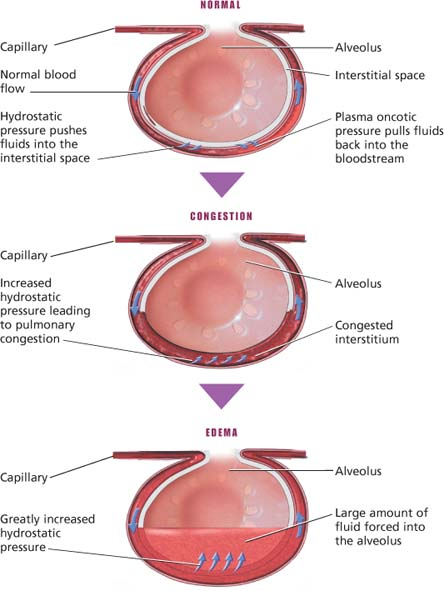
Pulmonary edema is the accumulation of fluid in the extravascular spaces of the lung. With cardiogenic pulmonary edema, fluid accumulation results from elevations in pulmonary venous and capillary hydrostatic pressures. A common complication of cardiac disorders, pulmonary edema can occur as a chronic condition or it can develop quickly and cause death.
Pulmonary edema usually results from left-sided heart failure due to arteriosclerotic, hypertensive, cardiomyopathic, or valvular heart disease. With such disorders, the compromised left ventricle can’t maintain adequate cardiac output; increased pressures are transmitted to the left atrium, pulmonary veins, and pulmonary capillary bed. This increased pulmonary capillary hydrostatic force promotes transudation of intravascular fluids into the pulmonary interstitium, decreasing lung compliance and interfering with gas exchange.
Signs and symptoms
Cold, clammy, and sweaty skin
Cough
Decreased level of consciousness
Dependent crackles or wheezing
Diastolic (S3) gallop
Dyspnea on exertion
Frothy, bloody sputum
Hypoxemia
Jugular vein distention
Orthopnea
Paroxysmal nocturnal dyspnea
Restlessness and anxiety
Tachycardia
Tachypnea
Thready pulse
Treatment
High concentrations of oxygen by cannula, face mask and, if necessary, assisted ventilation
Angiotensin-converting enzyme inhibitors, diuretics, inotropic drugs such as digoxin (Lanoxin), antiarrhythmic agents, beta-adrenergic blockers, and human B-type natriuretic peptide to treat heart failure
Vasodilator drugs, such as nitroprusside (Nipride) to reduce preload and afterload in acute episodes of pulmonary edema
Morphine to reduce anxiety and dyspnea as well as to dilate the systemic venous bed, promoting blood flow from pulmonary circulation to the periphery
Nursing considerations
Administer oxygen, as ordered, and monitor pulse oximetry.
Monitor vital signs every 15 to 30 minutes while giving nitroprusside in dextrose 5% in water by I.V. drip.
Watch for arrhythmias in patients receiving cardiac glycosides and diuretics and for marked respiratory depression in those receiving morphine.
Assess the patient’s condition frequently, and record response to treatment. Monitor arterial blood gas levels, electrolytes, oral and I.V. fluid intake, urine output and, in the patient with a pulmonary artery catheter, pulmonary end-diastolic and wedge pressures. Check cardiac monitor often. Report changes immediately.
Reassure the patient, who will have anxiety due to hypoxia and respiratory distress. Explain all procedures. Provide emotional support to his family as well.
Place the patient in high Fowler’s position to enhance lung expansion.
 Teaching about pulmonary edema
Teaching about pulmonary edema
Explain all procedures to the patient and his family.
Review all prescribed drugs with the patient. If he takes digoxin (Lanoxin), show him how to monitor his own pulse rate and warn him to report signs of toxicity.
Encourage the patient to eat potassium-rich foods to lower the risk of cardiac arrhythmias.
If the patient takes a vasodilator, teach him the signs of hypotension and emphasize the need to avoid alcohol.
Urge the patient to comply with the prescribed drug regimen to avoid future episodes of pulmonary edema.
Emphasize the need to report early signs of fluid overload.
Discuss ways to conserve physical energy.
Pulmonary embolism
Pulmonary embolism is an obstruction of the pulmonary arterial bed that occurs when a mass—such as a dislodged thrombus—lodges in a pulmonary artery branch, partially or completely obstructing it. This causes a ventilation-perfusion mismatch, resulting in hypoxemia, as well as intrapulmonary shunting.
The prognosis varies. Although the pulmonary infarction that results from embolism may be so mild that the patient is asymptomatic, massive embolism (more than 50% obstruction of pulmonary arterial circulation) and infarction can cause rapid death.
In most patients, pulmonary embolism results from a dislodged thrombus (blood clot) that originates in the leg veins. More than one-half of such thrombi arise in the deep veins of the legs; usually multiple thrombi arise. Other, less common sources of thrombi include the pelvic, renal, and hepatic veins, the right side of the heart, and the upper extremities.
Signs and symptoms
Cyanosis
Dyspnea or unexplained shortness of breath
Hypotension
Jugular vein distention
Low-grade fever
Pleuritic pain or chest pain
Productive cough (sputum may be blood tinged)
Tachycardia or arrhythmia
Treatment
Oxygen therapy
Fibrinolytic therapy
Anticoagulation with heparin
Embolectomy
Vasopressors and antibiotics
Vena caval ligation, plication, or insertion of a device to filter blood returning to the heart and lungs to prevent future pulmonary emboli
Understanding thrombus formation
Thrombus formation results from vascular wall damage, venous stasis, and hypercoagulability of the blood. Trauma, clot dissolution, intravascular pressure changes, or a change in peripheral blood flow can cause the thrombus to loosen or become fragmented. Then, the thrombus—now called an embolus—floats to the heart’s right side and enters the lung through the pulmonary artery. There, the embolus may dissolve, become more fragmented, or grow.
By occluding the pulmonary artery, the embolus prevents alveoli from producing enough surfactant to maintain alveolar integrity. As a result, alveoli collapse and atelectasis develops. If the embolus enlarges, it may clog most or all pulmonary vessels and cause right-sided heart failure and death.
Who’s at risk for pulmonary embolism?
Many disorders and treatments increase the risk of pulmonary embolism. Risk is particularly high for patients who have had recent surgery. The anesthetic used during surgery can injure lung vessels, and surgery or prolonged immobility can promote venous stasis, further compounding the risk.
Predisposing disorders
Lung disorders, especially chronic types
Cardiac disorders
Infection
Cancer
History of thromboembolism, thrombophlebitis, or venous insufficiency
Sickle cell disease
Autoimmune hemolytic anemia
Polycythemia
Osteomyelitis
Long-bone fracture
Manipulation or disconnection of central lines
Coagulation disorders
Venous stasis
Prolonged immobilization
Obesity
Age older than 40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

 Asthmatic bronchus
Asthmatic bronchus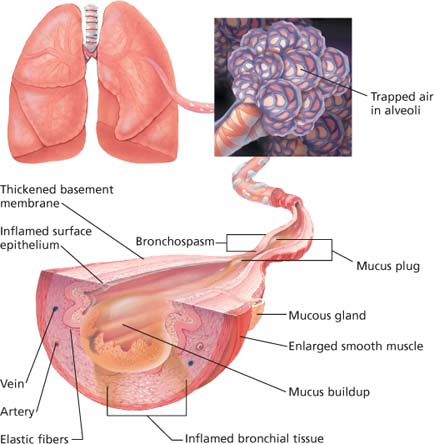
 Lung changes in emphysema
Lung changes in emphysema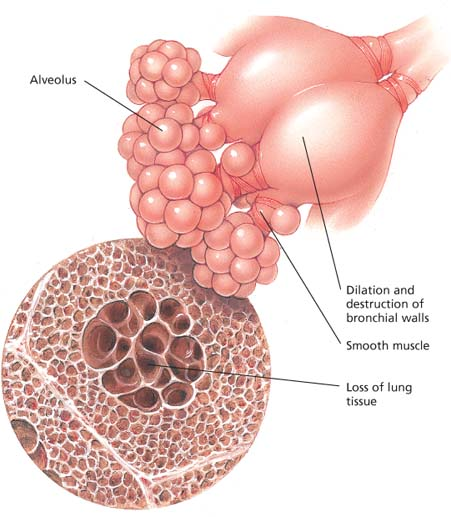
 Tumor infiltration in lung cancer
Tumor infiltration in lung cancer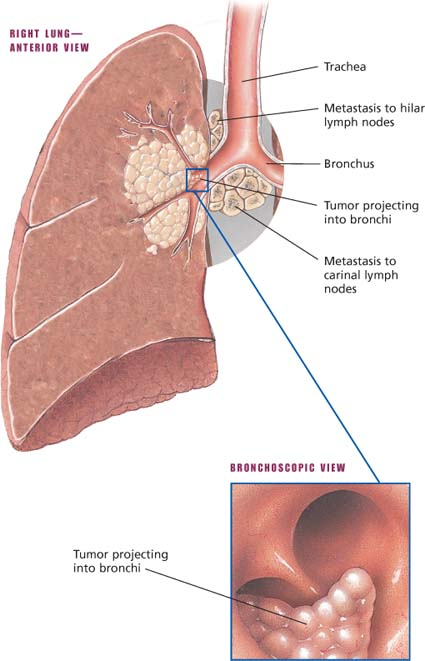
 Locations of pneumonia
Locations of pneumonia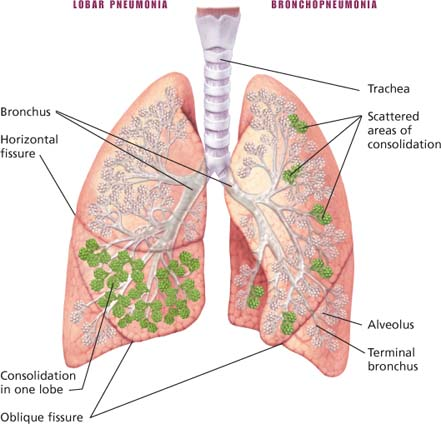
 How pulmonary edema develops
How pulmonary edema develops