Renal Failure
Renal failure is classified as acute or chronic. Acute renal failure (ARF) (now frequently called “acute kidney injury”) has a mortality rate of 10% to 60%, begins abruptly, and is characterized as a sudden decline in renal function resulting in the inability to maintain fluid and electrolyte balance and excretion of waste products. ARF is generally reversible, whereas chronic renal failure (CRF) has an eventual mortality rate of 100% (without dialysis and/or renal transplantation), is irreversible, and results in a slow, steady decline of renal function. This chapter discusses the pathophysiology and treatment for acute and chronic renal failure.
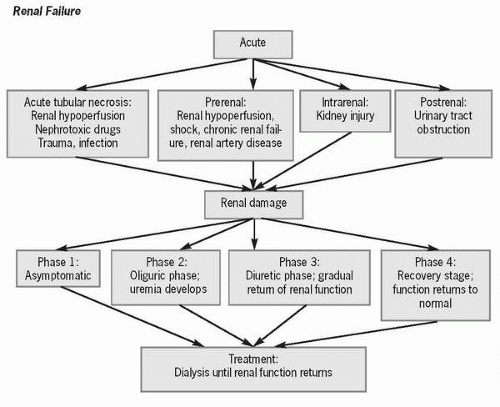 Figure 63-1 Renal failure. |
Prevention of ARF depends in part on limiting one’s exposure to nephrotoxic agents and prevention and prompt treatment of shock, especially in the elderly and people with renal insufficiency. CRF can be avoided with tight control of hypertension and diabetes; genetic counseling for persons with polycystic renal disease, which is an inheritable cause of renal failure; and prompt treatment of ARF.
Pathophysiology
Approximately 10,000 people develop ARF each year. It has been estimated that 5% of hospital admissions, 30% of clients in critical care units, and 25% of all hospitalized patients develop ARF.
 It has been estimated that 5% of hospital admissions, 30% of clients in critical care units, and 25% of all hospitalized patients develop ARF.
It has been estimated that 5% of hospital admissions, 30% of clients in critical care units, and 25% of all hospitalized patients develop ARF.Acute tubular necrosis (ATN), one cause of ARF, occurs because of renal hypoperfusion or in response to nephrotoxic drugs, such as aminoglycosides, and chemicals, such as radiological dyes, which set up an inflammatory process leading to tubular edema, obstruction, and ischemia. Up to 12% of patients exposed to radiocontrast agents develop ATN. Other causes of ATN are major trauma, systemic infections, and muscle breakdown, which produces myoglobin, a substance that clogs renal tubules. Damaged tubules result in a decreased ability to maintain homeostasis. ATN usually resolves in about 8 weeks.
 Up to 12% of patients exposed to radiocontrast agents develop ATN.
Up to 12% of patients exposed to radiocontrast agents develop ATN.The factors that instigate prerenal ARF (i.e., factors that occur before blood being filtered by the kidneys) are caused by renal hypoperfusion and account for approximately 40-80% of ARF cases per year. Prerenal factors include those that cause decreased cardiac output such as shock and congestive heart failure, volume depletion from vomiting, or increased renal vascular resistance as occurs in renal artery stenosis. If perfusion can be restored in a short amount of time, permanent renal damage can be averted. In prerenal ARF, urine osmolality is high and urine sodium is low, because although renal perfusion is greatly decreased, renal tubular function is normal.
Intrarenal ARF results from injury to the kidney itself from emboli or ATN. Sodium cannot be conserved and urine cannot be concentrated because of glomerular damage. Postrenal or obstructive ARF results from urinary tract obstruction by renal calculi or prostatic enlargement; thus urine osmolarity and sodium levels are usually unaffected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



