Renal Failure
QUICK LOOK AT THE CHAPTER AHEAD
This chapter discusses the etiology of renal failure defined as the inability to concentrate water, balance electrolytes, and remove waste products. Renal failure is classified as either acute or chronic. Acute renal failure begins abruptly and is generally reversible. Chronic renal failure has an eventual mortality rate of 100% (without dialysis and/or renal transplantation), is irreversible, and results in a slow steady decline of renal function.
The most common causes of acute renal failure (ARF) in children are hemolytic-uremic syndrome and dehydration. Prevention of ARF depends in part on limiting the child’s exposure to nephrotoxic agents, eliminating exposure to unpasteurized products and undercooked meat, and prevention and prompt treatment of dehydration and shock.
In ARF the glomerular filtration rate (GFR) is greatly reduced, the blood urea nitrogen level rises, and sodium is not efficiently reabsorbed from the proximal tubule. Because the distal tubule has a high amount of sodium the renin-angiotensin system is activated, which causes constriction of the afferent arteriole, thereby further reducing the GFR and continuing the cycle (Figure 47-1).
Pathophysiology
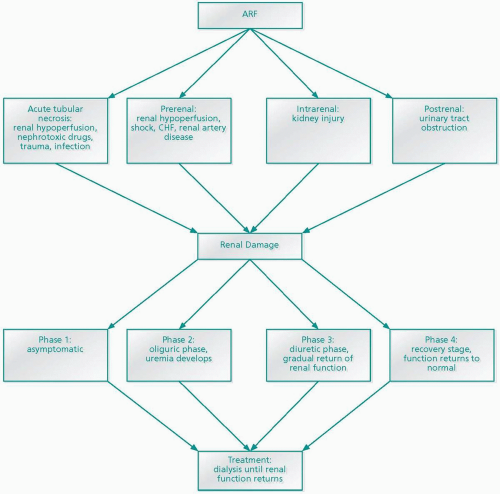
Prerenal, intrarenal, and postrenal factors may cause ARF. Prerenal factors (factors that occur before blood being filtered by the kidneys) may be caused by anything that promotes renal hypoperfusion. Prerenal factors include shock, congestive heart failure, volume depletion from vomiting/diarrhea, or diabetic acidosis. The most common cause of decreased renal perfusion in children is dehydration. In prerenal ARF urine osmolality is high (50 mOsm/kg higher than plasma osmolality), urine sodium is low (below 10 mEq/1), and specific gravity is less than 1.020. Although renal perfusion is greatly decreased, renal tubular function is normal. Children may exhibit nonspecific symptoms such as fever, dehydration, and tachycardia.
Intrarenal ARF (intrinsic) results from injury to the kidney itself. This type of ARF may be caused by hemolytic-uremic syndrome, nephrotoxins such as contrast dye, ingestion of poison, glomerulonephritis, acute tubular necrosis, severe infection, liver failure, and chemotherapy, resulting in large amounts of calcium and uric acid excretion. Because of glomerular damage sodium cannot be conserved and urine cannot be concentrated. The child may present with nausea/vomiting, hypertension, and oliguria.
Postrenal or obstructive ARF results from urinary tract outflow obstruction by renal calculi, tumors, trauma resulting in hematoma, neurogenic bladder, or structural abnormalities such as ureterovesical junction stricture. Newborn delayed voiding after birth, electrolyte imbalance, a poor urinary stream, and/or abdominal mass suggests a structural
abnormality and should be investigated promptly. Urine osmolality and sodium levels are usually unaffected.
abnormality and should be investigated promptly. Urine osmolality and sodium levels are usually unaffected.
ARF has four phases. In the initial phase, although renal damage is occurring, the child may be asymptomatic. During the second, or oliguric, phase less than 1 mL/kg/hr of urine is produced. This stage usually lasts from 10 days to several weeks. Impaired glomerular filtration causes solute and water reabsorption, urine output declines, and serum waste products cannot be removed. As the child becomes symptomatic, a condition known as uremia (urine in the blood) develops. Neurotoxicity from uremia causes an altered mental status and altered peripheral sensation. Electrolyte imbalance causes dysrhythmias, water retention may lead to congestive heart failure and hypertension, and metabolic acidosis may develop because of the kidney’s inability to excrete hydrogen ions. In addition to anemia caused by decreased erythropoietin production, blood loss may be caused by gastrointestinal bleeding secondary to platelet and protein anticoagulant dysfunction.
During the third phase, or the diuretic phase, which lasts days to weeks, there is a gradual return of renal function due to cellular regeneration and healing. Excessive urine output leading to dehydration and electrolyte imbalance may occur during this stage as a result of incompetent tubular transport of water and solutes. The fourth and final phase is the recovery stage during which glomerular function gradually returns to normal. The recovery stage may take several months. If left untreated ARF can result in fluid overload, electrolyte imbalance, metabolic acidosis, uremia, and coma. ARF is treated by supportive care, including volume restoration, diuretic administration, and/or dialysis.
Chronic renal failure (CRF) in children is rare and most commonly develops because of abnormal renal and urinary tract structure. CRF in children younger than 5 years of age may develop because of uncorrected urinary tract structural abnormalities. Children ages 5 to 15 may develop CRF because of chronic renal infections and heredity disorders such as polycystic kidney disease (Figure 47-2). Long-term uncontrolled hypertension and/or diabetes mellitus can lead to CRF in young adults.
In some children the kidneys do not develop (agenesis), whereas in others development is poor (dysgenesis). Untreated severe vesicoureteral reflux, chronic glomerulonephritis, diabetes, lupus, and polycystic disease may also lead to CRF. Renal function steadily declines as nephrons are replaced with scar tissue. Renal
insufficiency denotes a 20% to 50% reduction in the GFR. When renal function in each kidney is reduced by 50%, signs and symptoms of mild azotemia (buildup of nitrogenous waste products in the blood), polyuria, nocturia, hypertension, and anemia become apparent. As the GFR drops to 20-25% of normal, the term renal failure is used.
insufficiency denotes a 20% to 50% reduction in the GFR. When renal function in each kidney is reduced by 50%, signs and symptoms of mild azotemia (buildup of nitrogenous waste products in the blood), polyuria, nocturia, hypertension, and anemia become apparent. As the GFR drops to 20-25% of normal, the term renal failure is used.