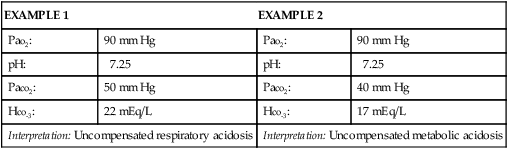
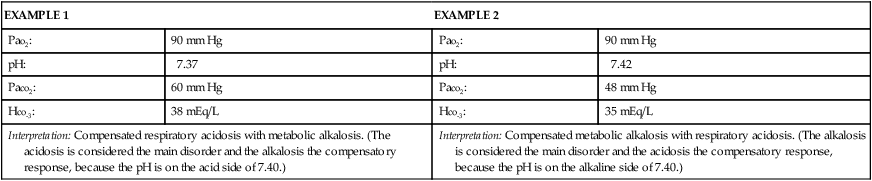
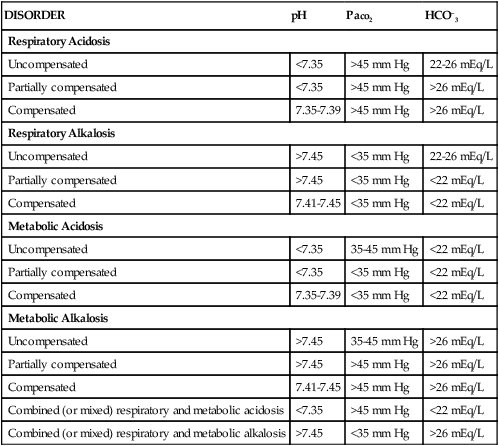
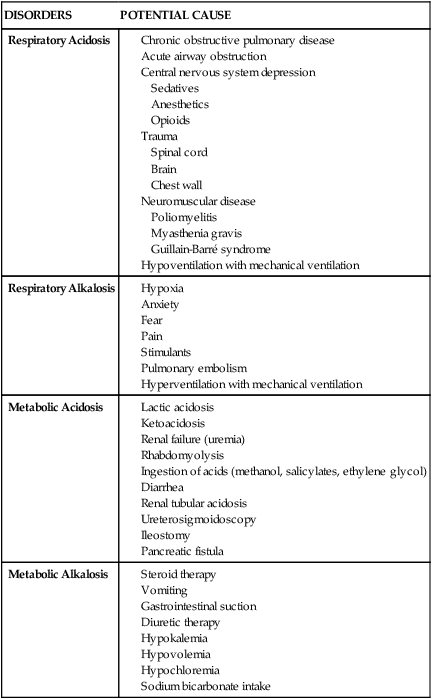
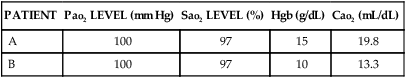
Interpretation of arterial blood gas (ABG) levels can be difficult, especially if the nurse is under pressure to do it quickly and accurately. One method that can help ensure accuracy when analyzing ABG levels is to follow the same steps of interpretation each time. A specific method to be used each time that blood gas values must be interpreted is presented here (Box 19-1). Look at the Pao2 level, and answer this question: Does the Pao2 show hypoxemia? The Pao2 is a measure of the partial pressure (P) of oxygen dissolved in arterial (a) blood plasma. Sometimes, Pao2 is shortened to Po2. It is reported in millimeters of mercury (mm Hg). Pao2 reflects 3% of total oxygen in the blood.1 The normal range of Pao2 values for persons breathing room air at sea level is 80 to 100 mm Hg. However, the normal range is age dependent for infants and for persons 60 years old or older. The normal level for infants breathing room air is between 50 and 70 mm Hg.2 The normal level for persons 60 years old or older decreases with age as changes occur in the ventilation/perfusion (V/Q) matching in the aging lung.1,3 The correct Pao2 for older persons can be ascertained as follows: 80 mm Hg (the lowest normal value) minus 1 mm Hg for every year of age above 60 years. Using this formula, a 65-year-old individual can have a Pao2 as low as 75 mm Hg (80 mm Hg − 5 mm Hg = 75 mm Hg) and still be within the normal range. An acceptable range for an 80-year-old person (20 years older than 60 years) is 60 mm Hg (80 mm Hg − 20 mm Hg = 60 mm Hg). At any age, a Pao2 lower than 40 mm Hg represents a life-threatening situation that necessitates immediate action.1 A Pao2 value less than the predicted lowest value indicates hypoxemia, which means that a lower-than-normal amount of oxygen is dissolved in plasma.1 Look at the pH level, and answer this question: Is the pH on the acid or alkaline side of 7.40? The pH is the hydrogen ion (H+) concentration of plasma. Calculation of pH is accomplished by using the partial pressure of carbon dioxide (Paco2) and the plasma bicarbonate level (HCO3−). The formula used is the Henderson-Hasselbalch equation (see Appendix B).4 The normal pH of arterial blood is 7.35 to 7.45, and the mean is 7.40. If the pH level is less than 7.40, it is on the acid side of the mean. A pH level less than 7.35 is known as acidemia, and the overall condition is called acidosis. If the pH level is greater than 7.40, it is on the alkaline side of the mean. A pH level greater than 7.45 is known as alkalemia, and the overall condition is called alkalosis.1,4,5 Look at the Paco2 level, and answer this question: Does the Paco2 show respiratory acidosis, alkalosis, or normalcy? The Paco2 is a measure of the partial pressure of carbon dioxide dissolved in arterial blood plasma, and it is reported in millimeters of mercury (mm Hg). It is the acid–base component that reflects the effectiveness of ventilation in relation to the metabolic rate.4 In other words, the Paco2 value indicates whether the patient can ventilate well enough to rid the body of the carbon dioxide produced as a consequence of metabolism. The normal range for Paco2 is 35 to 45 mm Hg. This range does not change as a person ages. A Paco2 value greater than 45 mm Hg defines respiratory acidosis, which is caused by alveolar hypoventilation. Hypoventilation can result from chronic obstructive pulmonary disease (COPD), oversedation, head trauma, anesthesia, drug overdose, neuromuscular disease, or hypoventilation with mechanical ventilation.6 Ventilatory failure results when the Paco2 level exceeds 50 mm Hg. Acute ventilatory failure occurs when the Paco2 level is greater than 50 mm Hg and the pH level is less than 7.30. It is referred to as acute because the pH is abnormal, not allowing enough time for the body to compensate by returning the pH to the normal range. Chronic ventilatory failure is defined as a Paco2 value greater than 50 mm Hg and a pH level greater than 7.30.1,7 A Paco2 value that is less than 35 mm Hg defines respiratory alkalosis, which is caused by alveolar hyperventilation. Hyperventilation can result from hypoxia, anxiety, pulmonary embolism, pregnancy, and hyperventilation with mechanical ventilation or as a compensatory mechanism for metabolic acidosis.4 Look at the HCO3− level, and answer this question: Does the HCO3− show metabolic acidosis, alkalosis, or normalcy? Bicarbonate (HCO3−) is the acid–base component that reflects kidney function. The bicarbonate level is reduced or increased in the plasma by renal mechanisms. The normal range is 22 to 26 mEq/L.4,5 A bicarbonate level of less than 22 mEq/L defines metabolic acidosis, which can result from ketoacidosis, lactic acidosis, renal failure, or diarrhea. The cumulative effect is a gain of acids or a loss of base. A bicarbonate level that is greater than 26 mEq/L defines metabolic alkalosis, which can result from fluid loss from the upper gastrointestinal tract (vomiting or nasogastric suction), diuretic therapy, severe hypokalemia, alkali administration, or steroid therapy.4,5,6 Look again at the pH level, and answer this question: Does the pH show a compensated or an uncompensated condition? If the pH level is abnormal (less than 7.35 or greater than 7.45), the Paco2 value or the HCO3− level, or both, will also be abnormal. This is an uncompensated condition because the body has not had enough time to return the pH to its normal range.4,5,6,8 Box 19-2 provides two examples of uncompensated ABGs. If the pH level is within normal limits and the Paco2 value and the HCO3− level are abnormal, the condition is compensated because the body has had enough time to restore the pH to within its normal range.4,5,6,8 Differentiating the primary disorder from the compensatory response can be difficult. The primary disorder is the abnormality that caused the pH level to shift initially. It is determined according to the pH level; the primary disorder is considered to be the one on whichever side of 7.40 the pH level occurs.4,8 Box 19-3 provides two examples of compensated ABGs. Partial compensation may be present and is evidenced by abnormal pH, Paco2, and HCO3− levels, indications that the body is attempting to return the pH to its normal range.4,8 Table 19-1 summarizes the changes in the acid–base components that accompany various acid–base disorders.4,5,8 In addition to the parameters previously discussed, other factors must be considered when reviewing a patient’s ABGs, including oxygen saturation, oxygen content, base excess and deficit, and anion gap analysis. Table 19-2 summarizes conditions that may potentiate acid–base abnormalities.4,5,8 TABLE 19-1 TABLE 19-2 Oxygen saturation is a measure of the amount of oxygen bound to hemoglobin, compared with hemoglobin’s maximal capability for binding oxygen. It can be assessed as a component of the ABG (Sao2) or can be measured noninvasively using a pulse oximeter (Spo2).9,10 Oxygen saturation is reported as a percentage or as a decimal; normal values are greater than 95% when the patient is on room air. Normally, the saturation level cannot reach 100% (on room air) because of physiologic shunting.1 However, when supplemental oxygen is administered, oxygen saturation may approach 100% so closely that it is reported as 100%. Proper evaluation of the oxygen saturation level is vital. For example, an Sao2 of 97% means that 97% of the available hemoglobin is bound with oxygen. The word available is essential to evaluating the Sao2 level, because the hemoglobin level is not always within normal limits and oxygen can bind only with what is available. A 97% saturation level associated with 10 g/dL of hemoglobin does not deliver as much oxygen to the tissues as does a 97% saturation level associated with 15 g/dL of hemoglobin. Assessing only the Sao2 level and finding it within normal limits does not ensure that the patient’s oxygenation status is normal. The hemoglobin level must also be evaluated before a decision on oxygenation status can be made.1,9,10 Oxygen content (Cao2) is a measure of the total amount of oxygen carried in the blood, including the amount dissolved in plasma (measured by the Pao2) and the amount bound to the hemoglobin molecule (measured by the Sao2). Cao2 is reported in milliliters of oxygen carried per 100 mL of blood. The normal value is 20 mL of oxygen per 100 mL of blood. To calculate the oxygen content, the Pao2, the Sao2, and the hemoglobin level are used (see Appendix B). A change in any one of these parameters will affect the Cao2.1 The value of assessing the Cao2 is best illustrated by the examples in Table 19-3. The ABG parameters that are used most commonly to evaluate oxygenation status (Pao2 and Sao2) are both normal. Assessing only the Pao2 and the Sao2 would lead to the invalid conclusion that Patient B’s oxygenation status is normal. However, consideration of the hemoglobin level and the Cao2 reveals that the oxygenation of Patient B’s blood is significantly abnormal. TABLE 19-3 Base excess and base deficit reflect the nonrespiratory contribution to acid–base balance and are reported in milliequivalents per liter (mEq/L) above or below the normal range of −2 mEq/L to +2 mEq/L. A negative base level is reported as a base deficit, which correlates with metabolic acidosis, whereas a positive base level is reported as a base excess, which correlates with metabolic alkalosis.1,4,8
Pulmonary Diagnostic Procedures
Laboratory Studies
Arterial Blood Gases
Steps for Interpretation of Blood Gas Levels
Step 1.
Step 2.
Step 3.
Step 4.
Step 5.
DISORDER
pH
Paco2
HCO–3
Respiratory Acidosis
Uncompensated
<7.35
>45 mm Hg
22-26 mEq/L
Partially compensated
<7.35
>45 mm Hg
>26 mEq/L
Compensated
7.35-7.39
>45 mm Hg
>26 mEq/L
Respiratory Alkalosis
Uncompensated
>7.45
<35 mm Hg
22-26 mEq/L
Partially compensated
>7.45
<35 mm Hg
<22 mEq/L
Compensated
7.41-7.45
<35 mm Hg
<22 mEq/L
Metabolic Acidosis
Uncompensated
<7.35
35-45 mm Hg
<22 mEq/L
Partially compensated
<7.35
<35 mm Hg
<22 mEq/L
Compensated
7.35-7.39
<35 mm Hg
<22 mEq/L
Metabolic Alkalosis
Uncompensated
>7.45
35-45 mm Hg
>26 mEq/L
Partially compensated
>7.45
>45 mm Hg
>26 mEq/L
Compensated
7.41-7.45
>45 mm Hg
>26 mEq/L
Combined (or mixed) respiratory and metabolic acidosis
<7.35
>45 mm Hg
<22 mEq/L
Combined (or mixed) respiratory and metabolic alkalosis
>7.45
<35 mm Hg
>26 mEq/L
DISORDERS
POTENTIAL CAUSE
Respiratory Acidosis
Respiratory Alkalosis
Metabolic Acidosis
Metabolic Alkalosis
Oxygen Saturation
Oxygen Content
PATIENT
Pao2 LEVEL (mm Hg)
Sao2 LEVEL (%)
Hgb (g/dL)
Cao2 (mL/dL)
A
100
97
15
19.8
B
100
97
10
13.3
Base Excess and Base Deficit
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine