Pressure Ulcer Care
As the name implies, pressure ulcers result when pressure—applied with great force for a short period or with less force over a long period—impairs circulation, depriving tissues of oxygen and other life-sustaining nutrients. This process damages skin and underlying structures. Untreated, resulting ischemic lesions can lead to serious infection.
Most pressure ulcers develop over bony prominences, where friction and shearing force combine with pressure to break down skin and underlying tissues. Persistent pressure on bony prominences obstructs capillary blood flow, leading to tissue necrosis. Common sites include the sacrum, coccyx, ischial tuberosities, and greater trochanters. Other common sites include the skin over the vertebrae, scapulae, elbows, knees, and heels in bedridden and relatively immobile patients.
Successful pressure ulcer treatment involves relieving pressure, restoring circulation, promoting adequate nutrition and, if possible, resolving or managing related disorders. Typically, the effectiveness and duration of treatment depend on the pressure ulcer’s characteristics.1 (See Staging pressure ulcers.)
Ideally, prevention is the key to avoiding extensive therapy. Preventive measures include off-loading pressure, maintaining adequate nourishment, and ensuring mobility to relieve pressure and promote circulation.2 Performing a risk assessment is necessary to implement effective prevention strategies.2 (See Braden scale: Predicting pressure ulcer risk, pages 602 and 603.)
When a pressure ulcer develops despite preventive efforts, treatment includes methods to decrease pressure, such as frequent repositioning to shorten pressure duration and the use of special equipment to reduce pressure intensity. Treatment also may involve pressure-reducing devices, such as special beds, mattresses, mattress overlays, and chair cushions.
Equipment
Pressure-redistribution device ▪ pillows ▪ lotion ▪ protective moisture barrier ▪ gloves.
Staging Pressure Ulcers1
Pressure ulcer staging reflects the depth and extent of tissue involvement. The classification system developed by the National Pressure Ulcer Advisory Panel is the most widely used system and categorizes pressure ulcers into four stages and two additional categories—suspected deep tissue injury and unstageable pressure ulcers.
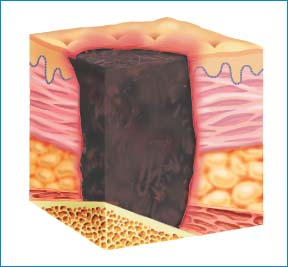
Suspected Deep Tissue Injury
Deep tissue injury is characterized by a purple or maroon localized area of intact skin or blood-filled blister caused by damage of underlying soft tissue from pressure or shear. It may be preceded by tissue that’s painful, firm, mushy, boggy, or warm or cool compared with adjacent tissue. The depth of the suspected deep tissue injury is unknown. It may be difficult to detect in individuals with dark skin tones. It may initially appear as a thin blister over a dark wound bed.
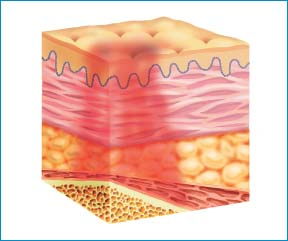 |
Stage I
Stage I ulcers are characterized by intact skin with nonblanchable redness of a localized area, usually over a bony prominence. The area may be warmer or cooler than adjacent tissue or painful and firm or soft. Darkly pigmented skin may not have visible blanching, but its color and temperature may differ from the surrounding area.
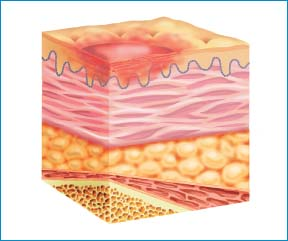 |
Stage II
A stage II pressure ulcer is characterized by partial-thickness loss of the dermis, presenting as a shallow, open ulcer with a red-pink wound bed without slough. It may also present as an intact or open serum-filled blister. This stage shouldn’t be used to describe skin tears, tape burns, excoriation, perineal dermatitis, or maceration.
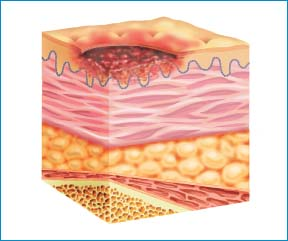 |
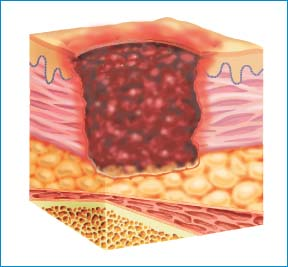
Stage III
A stage III pressure ulcer is characterized by full-thickness tissue loss. Subcutaneous fat may be visible, but bone, tendon, and muscle aren’t exposed. Slough may be present, but it doesn’t obscure the depth of tissue loss. Undermining and tunneling may be present. The depth of a stage III ulcer varies by anatomical location.
 |
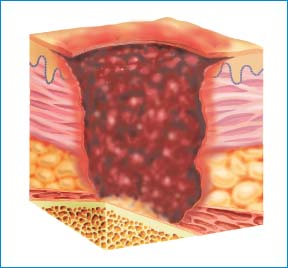
Stage IV
A stage IV pressure ulcer involves full-thickness tissue loss with exposed bone, tendon, or muscle. Slough or eschar may be present on some parts of the wound bed. Undermining and tunneling are also common. The depth of a stage IV ulcer varies by anatomic location.
 |
Implementation
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access