Pharmacology
Michelle S. Turner PharmD, BCPS
Susan K. Poole MS, BSN, RN, CRNI®, CNSN, CIC
 I. Considerations for Intravenous Drug Administration
I. Considerations for Intravenous Drug AdministrationA. Nursing Responsibilities
1. Review the order for the appropriateness of prescribed therapy for the patient’s age and condition, access device, dose, rate, and route of administration, and follow the rights of medication administration
2. Review facility policy for the list of approved parenteral medications and solutions for each type of administration method and route
3. Be knowledgeable of indications for therapy, side effects, potential adverse reactions, and appropriate interventions
4. Evaluate and monitor the effectiveness of prescribed therapy; document patient response, adverse events, and interventions; communicate laboratory tests results
B. Legal Considerations
1. State Nurse Practice Act determines the scope of practice for professional nursing within a given geographical area
2. Personal liability: each individual is responsible for his/her actions
3. Medication errors
a. Definition
1) Is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient, or consumer
2) May be related to professional practice, healthcare products, procedures, and systems, including prescribing; order communication; product labeling, packaging, and nomenclature; compounding; dispensing; distribution; administration; education; monitoring; and use
b. Prevention—proactively looking at problem-prone areas of medication administration leads to reducing risks and preventing errors
c. Classification/reporting—understanding the type of error and reporting of near misses assist in the education process and identify common issues that lead to prevention
d. Safety factors—advocate for the use of engineering controls, protocols, and technology that is intended and has been shown to reduce medication errors
1) Electronic order entry
2) Smart pumps with drug libraries
3) Bar coding
4) Procedures for distraction-free medication administration
5) Establishment of protocols for high-risk intravenous drugs
6) Standardized drug concentrations or standard order sets
4. Documentation
a. A record in written or printed form, containing original, official, or legal information
1) Drug
2) Dosage
3) Rate of administration as given
4) Time of actual administration
5) Route of administration
6) Patient’s response to treatment
7) Nurse’s signature
b. Investigational drugs
1) Know federal and state laws
2) Review research protocol
3) Obtain signed, informed consent
4) Investigation protocols may be continued in alternative care settings if requirements met
C. Nursing Process
1. Patient assessment
a. Nursing history
1) Sequence and length are modified consistent with the type of therapy ordered, acuity level of patient, and clinical setting in which care is delivered
2) Health status: question patient concerning current health and health history, including disease-specific conditions, such as diabetes, cardiac disease, cirrhosis, and surgeries
3) Allergies: specific to foods and drugs; other allergies and type of reaction and severity
4) Medication history: for specific illness (e.g., diuretics, insulin, anticoagulants, aspirin, over-the-counter drugs, herbal products)
5) Patient care plan: develops an individualized plan of care relative to medication administration
6) Clinical assessment parameters
a) Age
b) Weight: such as percent loss in comparison with usual body weight and time span involved (30 days, 90 days)
c) Height
d) Body temperature
e) Skin
Tissue turgor
Appearance: skin should be dry and intact
Presence of rash or lesions
Presence of petechiae; absorption may be impeded with subcutaneous administration
f) Edema
g) Other sources of fluid loss, such as fistulas, vomiting, diarrhea, and drains
h) Sensorium
i) Related therapies may affect the ability to maintain patency of the infusion line; for example, hydrotherapy may limit the use of hand veins for infusion purposes, and hyperbaric medicine may necessitate removal of a flush solution from an intermittent infusion device before treatment
2. Laboratory data
a. Hematology
1) Prothrombin time (PT)
2) Partial thromboplastin time (PTT)
3) Antithrombin III (heparin cofactor activity)
4) Complete blood count (CBC)
b. Chemistry panel
1) Comprehensive measurement of the body’s chemical constituents found in the blood, including electrolytes, enzymes, hepatic and renal function, and blood sugar
2) Blood urea nitrogen (BUN)
c. Urine
1) Determines various properties of urine
2) Analysis of drug excretion is often measured
d. Therapeutic drug monitoring
1) Ensures appropriate dosing regimens so that the concentration of the drug is between the minimum level and the toxic level
2) Required for patients
a) Receiving combination therapies
b) With renal dysfunction
c) With third spacing in whom therapeutic failure would prove catastrophic
d) Who fail to have anticipated response to therapy, despite appropriate dosing
3) Blood levels
a) Peak: maximum drug concentration is achieved after administration of single dose
b) Trough: minimum drug concentration after administration of single dose
c) Sensitivities: a screen used in determining sensitivity or resistance of bacteria to specific drugs
d) Toxicology screens
3. Interventions
a. Administer solutions and medications prepared and dispensed from the pharmacy or as commercially prepared solutions and medications whenever feasible
b. Medications admixed outside of the pharmacy, pharmacy-labeled solutions, and medications labeled for emergent use should be started within 1 hour of preparation
c. Trace the administration set from the patient to the point of origin before making connections and on admission or transfer of a patient to a new setting
d. Aspirate for a positive blood return from the vascular access device (VAD) to confirm device patency prior to administration of parenteral medications and solutions
4. Evaluation of response to treatment
a. Evaluate and monitor the effectiveness of prescribed therapy; documenting patient response, adverse events, and interventions
1) Adverse reaction: an unwanted, unexpected, noxious, or potentially harmful reaction to a medication
b. Communicate to the licensed independent practitioner (LIP) and the patient care team the results of laboratory tests
c. Discontinue therapy when the nursing assessment determines that intervention is necessary (e.g., in the event of an adverse reaction, complication such as phlebitis or infiltration, suspected VAD malposition, or loss of VAD patency)
d. The LIP should be notified of the assessment and intervention immediately
5. Document discontinued therapy in the patient’s permanent medical record therapy, including amount infused, time, date, condition of the site, integrity of the catheter if removed, and reason for discontinuation
6. Provide instruction to the patient and caregiver about the observations and care of the infusion and catheter site and potential postinfusion complications, such as postinfusion phlebitis or infiltration, and document such instructions in the patient’s permanent medical record
 II. Drug Administration
II. Drug AdministrationA. Drug Preparation
1. Parenteral solutions: know the tonicity (hypertonic, hypotonic, or isotonic) of the parenteral solution and whether it is appropriate for the prescribed route
2. Syringes
a. Use the appropriate size syringe for the volume of drug/solution to be withdrawn
b. Syringe-to-syringe transfer is not recommended due to the risk of serious medication errors
3. Needles
a. Select the appropriate size needle for withdrawing solution from a vial or ampoule
b. If available and appropriate for the medication, needleless vial adapters may be used
c. Multidose vial use should be avoided
d. Blunted filter needles or filter straws should be used when withdrawing medications from glass ampoules
4. Inspect solutions and medications
a. Appropriate labeling
b. Integrity (no leakage/discoloration/open packaging)
c. Accuracy (right drug or solution and right dose)
d. Sterility (within beyond-use or expiration date)
e. In the home care setting, verify appropriate storage/refrigeration
B. Drug Forms
1. Powders: require reconstitution
2. Liquids: in the appropriate liquid form
3. Premixed: drugs may be premixed with intravenous additives
C. Drug Containers
1. Vials include double-compartment, pump-action, and additive piggyback
a. Single-use vial: hermetically sealed with rubber stopper and intended for one-time use
b. Multiple-dose vial: hermetically sealed with rubber stopper and designed to be entered more than once
2. Ampoules: a hermetically sealed glass medication container in which the neck of the container must be broken to access the medication
3. Prefilled syringes: minimize errors in calculation and ensure drug preparation in the correct volume of diluent
D. Drug Compatibility and Stability
1. Compatibility
a. Capability of being mixed and administered without undergoing undesirable chemical or physical changes or loss of therapeutic action
b. Factors affecting compatibility
1) Concentration of drug
2) Length of time drugs are in contact with other additives or diluent
3) pH of admixture
a) pH: symbol for degree of concentration of hydrogen ions or acidity of solution
4) Presence of buffers
a) Addition of buffers may minimize the potential for the development of phlebitis
2. Incompatibilities
a. Chemical: a change, which may or may not be visually observed, in the molecular structure or pharmacologic properties of a substance (e.g., penicillin and ascorbic acid, lowering the pH)
b. Physical: an undesirable change that is physically observed (e.g., sodium bicarbonate and calcium chloride, forming an insoluble precipitate)
c. Therapeutic: an undesirable reaction resulting from the overlapping effects of two drugs given together or closely together (e.g., penicillin and tetracycline, inhibiting the bactericidal effect of penicillin)
3. Drug stability
a. The length of time the drug retains its original properties and characteristics
b. Factors affecting drug stability
1) Parenteral solutions: tonicity may affect stability
2) Additive drugs: presence may affect pH
3) Buffers: used to stabilize the drug in solution
4) Preservatives: to prolong shelf-life
5) Time in solution: some drugs require admixing immediately before administration
6) Order of mixing: end product may be affected
7) Amount of diluent
8) Light
9) Temperature
E. Methods of IV Drug Administration
1. Bolus injection
2. IV drip (gravity) with or without flow control device
3. Infusion via mechanical (e.g., syringe pump, elastomeric) or electronic device
F. Drug Calculations
1. Drug dosage determination
a. Body surface area (BSA)
1) Frequently used to calculate dosage
2) Nomogram method: to calculate BSA, draw a straight line between the point representing patient’s height on left vertical scale and the point representing patient’s weight on right vertical scale. The point at which this line intersects the middle vertical scale represents the patient’s surface area in square meters
b. Ratio-proportion method
1) A ratio is a comparison between two related items, and a proportion is the equality of two ratios
2) When setting up a proportion, start with what you know about the drug from the label; the strength of the drug on hand (H) and the volume of the drug on hand (V). Place this information in the form of a ratio (H:V) on the left of the equal sign (=). The ratio for the dose desired is the relationship of the dose ordered (D) and the amount to give (G), and this is placed on the right side of the equal sign (H:V = D:G)
3) Thus, the strength on hand (H) is related (:) to the volume (V) as (=) the dose ordered (D) is related (:) to the amount to give (G)
4) For an answer to be correct, the product of the means must equal the product of the extremes. The extremes are always the two outside numbers
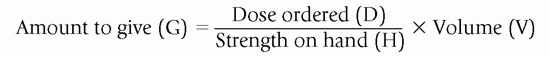
c. Formula method
2. Flow rate determination
a. Milliliter per hour: total volume (mL) ÷ administration time (hour) = milliliters per hour (mL/hour)
1) Milliliters per minute: milliliters per hour (mL/hour) ÷ minutes per hour (60) = milliliters per minutes (mL/minute)
2) Macrodrop infusion formula:
a) 10, 15, or 20 drops (drops) per 1 mL
b) Milliliters per minute (mL/minute) × drops per milliliter (drops/mL) = drops per minute (drops/minute)
3) Microdrop infusion formula:
a) 60 drops (drops) per 1 mL
b) Milliliters per minute (mL/minute) × drops per milliliter (drops/mL) = drops per minute (drops/minute)
b. Intermittent medication or solution calculation
1. Volume to be infused (mL) ÷ mL/hour = number of hours
3. Medication conversions
a. Microgram/kilogram (mcg/kg)
1) Kilogram × 1,000 = 1,000 grams
2) 1 gram × 1,000 = 1,000 milligrams (mg)
3) 1 milligram × 1,000 = 1,000 micrograms (mcg)
b. Milligrams per minute (mg/minute)
1) Determine the total amount of the drug in the solution
2) Divide the drug amount (in milligrams) by the total volume in solution (mL) = concentration of the solution (mg/mL)
3) Divide the desired amount of drug (in mg/minute) by the concentration of the solution (in mg/mL) = infusion rate (mL/minute)
4) To convert to mL/hour: mL/minute × 60 minutes/hour = mL/hour
4. Percentage solutions
a. Percent solution is a measure of parts per hundred
b. 1% solution = 1 g of drug in 100 mL of solution
 III. Drug Classifications
III. Drug ClassificationsA. Anti-infective Agents
1. Natural penicillins
a. Prototype: penicillin G potassium/sodium (Pfizerpen)
b. Indications: used to treat infections with penicillin-sensitive organisms such as meningitis or endocarditis
c. Usual dosage: 2,000,000 to 5,000,000 units every 4 hours
d. Mode of administration: intermittent, continuous
e. Major side effects: fever, chills, edema, urticaria, rash
f. Nursing considerations: monitor electrolyte balance because of sodium or potassium base
g. Patient/caregiver education: instruct patient to report venous pain
2. Aminopenicillin
a. Prototype: ampicillin sodium (Omnipen-N)
b. Indications: respiratory, ear, gastrointestinal, genitourinary, and skin infections
c. Usual dosage: 1 to 2 g every 4 to 6 hours
d. Mode of administration: push, intermittent
e. Major side effects: dermatitis, rash, urticaria, anemia
f. Nursing considerations: stability is concentration-dependent and decreases as the concentration of the drug increases; the drug is especially susceptible to inactivation in dextrose solutions
g. Patient/caregiver education: instruct patient to report skin rash, previous sensitivities
h. Related drug: ampicillin sodium/sulbactam sodium (Unasyn)
3. Penicillinase-resistant penicillin
a. Prototype: nafcillin sodium (Unipen)
b. Indication: infection caused by penicillinase-producing staphylococci
c. Usual dosage: 1 to 2 g every 4 hours
d. Mode of administration: push, intermittent
e. Major side effects: rash, fever, and pruritus
f. Nursing considerations: monitor renal, hepatic, and hematopoietic functions; local reactions can occur such as pain, phlebitis, thrombophlebitis, and occasionally skin sloughing with extravasation
g. Patient/caregiver education: instruct patient to recognize and report adverse effects
h. Related drug: oxacillin sodium (Bactocil)
4. Extended-spectrum penicillin
a. Prototype: piperacillin sodium and tazobactam sodium (Zosyn)
b. Indications: respiratory, urinary, skin, bone, and joint infections
c. Usual dosage: 2.25 to 4.5 g every 6 hours
d. Mode of administration: intermittent
e. Major side effects: rash, fever, nausea, neutropenia, and pruritus
f. Nursing considerations: evaluate renal and hematopoietic systems
g. Patient/caregiver education: instruct patient to report skin rash
h. Related drug: ticarcillin disodium/clavulanate potassium (Timentin)
5. Cephalosporins
a. First-generation agent
1) Prototype: cefazolin sodium (Kefzol, Ancef)
2) Indications: perioperative prophylaxis; bone, joint, respiratory, genitourinary, or gastrointestinal infections
3) Usual dosage: 500 mg to 2 g every 6 to 8 hours
4) Mode of administration: push, intermittent
5) Major side effects: urticaria, rash, nephrotoxicity, leukopenia, nausea, pain, and induration at site
6) Nursing considerations: in a patient with a penicillin allergy, cefazolin may cause cross-sensitivity (similarity in chemical structure); monitor infusion site for pain and induration
7) Patient/caregiver education: instruct patient in recognizing and reporting change at infusion site and flank pain
b. Second-generation agent
1) Prototype: cefuroxime sodium (Zinacef)
2) Indications: respiratory, urinary tract, and skin infections; sinusitis, bronchitis, pharyngitis, tonsillitis, otitis media
3) Usual dosage: 750 mg to 1.5 g every 8 hours
4) Mode of administration: push, intermittent
5) Major side effects: leukopenia, neutropenia, vomiting, oral thrush, rash, and diarrhea
6) Nursing considerations: may cause phlebitis; provide oral care
7) Patient/caregiver education: instruct patient to report changes in bowel habits
8) Related drugs: cefoxitin sodium (Mefoxin) and cefotetan disodium (Cefotan)
c. Third-generation agent
1) Prototype: ceftriaxone sodium (Rocephin)
2) Indications: meningitis, endocarditis; bone, joint, respiratory, intra-abdominal, genitourinary, and skin infections
3) Usual dosage: 1 to 2 g every 12 to 24 hours
4) Mode of administration: intermittent
5) Major side effects: diarrhea, rash, and eosinophilia
6) Nursing considerations: precipitation can occur when combined with solutions containing calcium (Ringer’s lactate, parenteral nutrition)
7) Patient/caregiver education: instruct patient to report any adverse effects
8) Related drugs: cefotaxime sodium (Claforan) and ceftazidime (Fortaz)
d. Fourth-generation agent
1) Prototype: cefepime hydrochloride (Maxipime)
2) Indications: serious bacterial infections such as pneumonia or febrile neutropenia
3) Usual dosage: 0.5 to 2 g every 8 to 12 hours
4) Mode of administration: intermittent
5) Major side effects: rash, diarrhea, seizures, and pain at infusion site
6) Nursing considerations: monitor renal function
7) Patient/caregiver education: teach signs and symptoms of allergic reaction
e. Fifth-generation agent
1) Prototype: ceftaroline fosamil (Teflaro)
2) Indications: pneumonia; skin and skin structure infections; treatment of infections due to methicillin-resistant Staphylococcus aureus
3) Usual dosage: 600 mg every 12 hours
4) Mode of administration: intermittent
5) Major side effects: diarrhea, nausea, rash, colitis, infusion site reactions
6) Nursing considerations: administer as a slow infusion over 60 minutes
7) Patient/caregiver education: instruct patient to report adverse effects
6. Carbapenems
a. Prototype: imipenem and cilastatin (Primaxin)
b. Indications: respiratory, skin, bone, joint, intra-abdominal, and gynecologic infections
c. Usual dosage: 250 to 500 mg every 6 hours
d. Mode of administration: intermittent
e. Major side effects: nausea, diarrhea, colitis, seizures, rash, pruritis
f. Nursing considerations: monitor intake and output; reduce the rate of infusion if nausea develops; monitor infusion site
g. Patient/caregiver education: instruct patient to report decreased urine output
h. Related drugs: meropenem (Merrem), doripenem (Doribax), ertapenem sodium (Invanz)
7. Aminoglycosides
a. Prototype: gentamicin sulfate (Garamycin)
b. Indications: specific gram-negative infections; a combination treatment for gram-positive infections
c. Usual dosage: 1 to 1.5 mg/kg every 8 hours or 7 mg/kg every 24 hours
d. Mode of administration: intermittent
e. Major side effects: ototoxicity, nephrotoxicity, neuromuscular blockade, and rash
f. Nursing considerations: monitor BUN, serum creatinine, and peak/trough levels
g. Patient/caregiver education: instruct patient to report hearing difficulties, tinnitus, dizziness, and changes in urine output
h. Related drugs: tobramycin sulfate (Nebcin), amikacin sulfate (Amikin)
8. Tetracyclines
a. Prototype: doxycycline hyclate (Vibramycin IV)
b. Indications: broad-spectrum against gram-negative and gram-positive organisms; treatment of uncommon infectious diseases
c. Usual dosage: 200 mg loading dose, and then 100 mg every 12 hours
d. Mode of administration: intermittent
e. Major side effects: anorexia, diarrhea, skin rashes, blood dyscrasias, photosensitivity, and thrombophlebitis
f. Nursing considerations: phlebitis may occur because doxycycline is inhibited by alkalinizing agents, infuse slowly over 1 to 4 hours
g. Patient/caregiver education: instruct patient to avoid exposure to sun when taking this medication and to recognize and report induration at the infusion site
h. Related drugs: minocycline (Minocin) and tigecycline (Tygacil)
9. Macrolides
a. Prototype: erythromycin lactobionate (Erythrocin IV)
b. Indications: staphylococcal, pneumococcal, streptococcal infections; infections due to atypical organisms such as chlamydia, mycoplasma, and mycobacteria
c. Usual dosage: 15 to 20 mg/kg over 24 hours or 4 mg/kg every 6 hours
d. Mode of administration: intermittent, continuous
e. Major side effects: abdominal pain, nausea, diarrhea, urticaria, and pain along the vein
f. Nursing considerations: monitor the infusion site for signs of phlebitis; reduce rate of infusion for pain at the infusion site
g. Patient/caregiver education: instruct patient to report pain or induration at infusion site
h. Related drug: azithromycin (Zithromax)
10. Quinolones
a. Prototype: ciprofloxacin lactate (Cipro)
b. Indications: genitourinary, sinus, prostate, skin, bone, and joint infections
c. Usual dosage: 200 to 400 mg every 12 hours
d. Mode of administration: intermittent
e. Major side effects: nausea, diarrhea, phlebitis, photosensitivity
f. Nursing considerations: infuse slowly over at least 60 minutes
g. Patient/caregiver education: instruct patient to avoid prolonged exposure to sunlight
h. Related drugs: levofloxacin (Levaquin) and moxifloxacin hydrochloride (Avelox)
11. Miscellaneous antibiotics
a. Aztreonam (Azactam)
1) Indications: serious infections due to gram-negative organisms
2) Usual dosage: 500 to 2,000 mg every 8 to 12 hours
3) Mode of administration: push, intermittent
4) Major side effects: diarrhea, rash, and phlebitis
5) Nursing considerations: monitor for infusion site reactions
6) Patient/caregiver education: instruct patient to report pain at infusion site
b. Chloramphenicol sodium succinate
1) Indications: treatment of uncommon infections, such as Rocky Mountain Spotted Fever, typhoid fever, and anthrax
2) Usual dosage: 12.5 mg/kg every 6 hours
3) Mode of administration: intermittent
4) Major side effects: aplastic anemia, optic neuritis, granulocytopenia, bone marrow depression, and gray syndrome
5) Nursing considerations: monitor CBC at baseline and every 2 to 3 days, monitor serum concentrations with a goal of 5 to 20 mcg/mL
6) Patient/caregiver education: instruct patient to report abnormal bruising or bleeding
c. Clindamycin phosphate (Cleocin)
1) Indications: treatment of gram-positive and anaerobic infections
2) Usual dosage: 600 to 900 mg every 8 hours
3) Mode of administration: intermittent
4) Major side effects: colitis, nausea, diarrhea, and phlebitis
5) Nursing considerations: monitor for infusion site reactions
6) Patient/caregiver education: instruct patient to report any changes in bowel habits
d. Colistimethate sodium (Coly-Mycin M)
1) Indications: treatment of multidrug-resistant gram-negative infections
2) Usual dosage: 1.25 mg/kg every 6 hours
3) Mode of administration: push, intermittent
4) Major side effects: nephrotoxicity, paresthesias, and neuromuscular blockade
5) Nursing considerations: monitor urine output, BUN, and serum creatinine
6) Patient/caregiver education: instruct patient to report decreased urine output or paresthesias
e. Daptomycin (Cubicin)
1) Indications: treatment of gram-positive infections such as endocarditis or bone and joint infections
2) Usual dosage: 4 to 6 mg/kg every 24 hours
3) Mode of administration: push, intermittent
4) Major side effects: rhabdomyolysis and eosinophilic pneumonia
5) Nursing considerations: monitor creatine kinase levels weekly
6) Patient/caregiver education: instruct patient to report muscle pain
f. Linezolid (Zyvox)
1) Indications: treatment of infections due to methicillin-resistant Staphylococcus aureus or vancomycin-resistant Enterococcus
2) Usual dosage: 600 mg every 12 hours
3) Major side effects: myelosuppression, neuropathy, lactic acidosis, and serotonin syndrome
4) Nursing considerations: monitor CBC weekly
5) Patient/caregiver education: instruct patient to report any new fevers
g. Quinupristin/dalfopristin (Synercid)
1) Indications: infections due to methicillin-resistant Staphylococcus aureus or vancomycin-resistant Enterococcus faecium
2) Usual dosage: 7.5 mg/kg every 8 hours
3) Mode of administration: intermittent
4) Major side effects: phlebitis, arthralgias, and QT prolongation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


