Peritoneal Dialysis
Like hemodialysis, peritoneal dialysis removes toxins from the blood of a patient with acute or chronic renal failure. But unlike hemodialysis, it uses the patient’s peritoneal membrane as a semipermeable dialyzing membrane. In this technique, a hypertonic dialyzing solution is instilled through a catheter inserted into the peritoneal cavity. (See Catheters for peritoneal dialysis.) Diffusion allows excessive concentrations of electrolytes and uremic toxins in the blood to move across the peritoneal membrane and into the dialysis solution. Excessive water in the blood moves across the peritoneal membrane by osmosis. After an appropriate dwelling time, the dialysis solution is drained, taking toxins and wastes with it.
Peritoneal dialysis may be performed by an automatic cycler machine or as continuous ambulatory peritoneal dialysis (CAPD). The cycler machine requires sterile set-up and connection technique.
Catheters for peritoneal dialysis
The first step in any type of peritoneal dialysis is insertion of a catheter to allow instillation of dialysate. The surgeon may insert one of three different catheters, as described below.
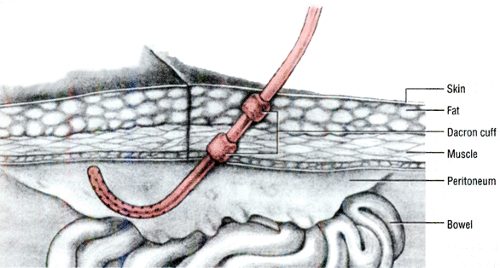
Tenckhoff catheter
To implant a Tenckhoff catheter, the surgeon inserts the first 6¾″(17.1 cm) of the catheter into the patient’s abdomen. The next 2¾″(7-cm) segment, which has a Dacron cuff at each end, is imbedded subcutaneously. Within a few days after insertion, the patient’s tissues grow around these Dacron cuffs, forming a tight barrier against bacterial infiltration. The remaining 37/8″(10 cm) of the catheter extends outside of the abdomen and is equipped with a metal adapter at the tip to allow connection to dialyzer tubing.
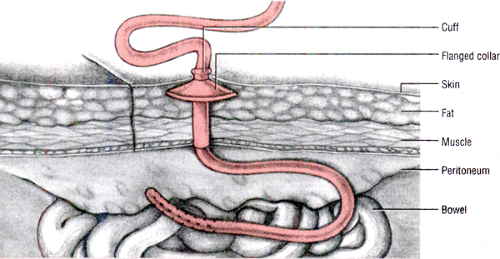
Flanged-collar catheter
To insert this kind of catheter, the surgeon positions its flanged collar just below the dermis so that the device extends through the abdominal wall. He keeps the distal end of the cuff from extending into the peritoneum, where it could cause adhesions.
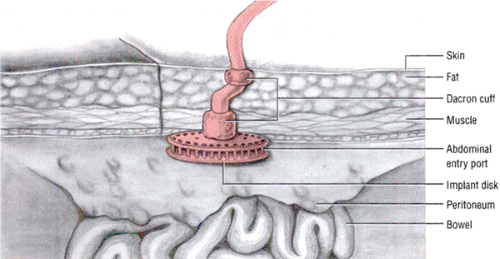
Column-disk peritoneal catheter
To insert a column-disk peritoneal catheter (CDPC), the surgeon rolls up the flexible disk section of the implant, inserts it into the peritoneal cavity, and retracts it against the abdominal wall. The implant’s first cuff rests just outside the peritoneal membrane, whereas the second cuff rests just beneath the skin. Because the CDPC doesn’t float freely in the peritoneal cavity, it keeps inflowing dialyzing solution from being directed at sensitive organs; this increases patient comfort during dialysis.
Because the patient himself performs CAPD, the method causes minimal disruption to the patient’s life by allowing him to remain active during dialysis. In CAPD, the patient uses a peritoneal catheter to instill dialysis solution into his peritoneal cavity. After the solution is instilled, the patient can attach a sterile cap to the catheter end and proceed with his normal activities as the solution remains in the peritoneal cavity. After 4 to 6 hours of dwelling time, the patient reconnects the peritoneal catheter to sterile tubing, allows the fluid to drain via gravity, and instills fresh dialysis solution. He repeats the process to ensure continuous dialysis 24 hours per day, 7 days per week.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree