Peripheral Nerve Stimulation
Peripheral nerve stimulation assesses and monitors the depth of neuromuscular blockade in patients receiving neuromuscular-blocking drugs, which are administered to produce paralysis. Neuromuscular-blocking drugs may be given to help synchronize breathing and mechanical ventilation in patients with severe lung injury; assist with the treatment of severe muscle spasms in patients with seizures, tetanus, or drug overdose; and help in the management of increased intracranial pressure in patients with head injury.
A peripheral nerve stimulator (PNS) is used to evaluate the level of neuromuscular blockade and determine the lowest therapeutic dose of the neuromuscular-blocking drug needed to produce paralysis. The PNS works by stimulating a peripheral nerve with a series of brief electrical pulses to produce a muscle response or twitch.
The train of four (TOF) is the most commonly used method for monitoring neuromuscular blockade. Using this method, a series of four electrical impulses are delivered to a particular peripheral
nerve. If four twitches occur, then 75% or less of the receptors are blocked. Three twitches occur when 80% of the receptors are blocked. One or two twitches correspond to 85% to 90% neuromuscular blockade. After the neuromuscular blockade drug is administered, it’s titrated so that each set of four electrical impulses produces one or two muscle twitches.
nerve. If four twitches occur, then 75% or less of the receptors are blocked. Three twitches occur when 80% of the receptors are blocked. One or two twitches correspond to 85% to 90% neuromuscular blockade. After the neuromuscular blockade drug is administered, it’s titrated so that each set of four electrical impulses produces one or two muscle twitches.
Equipment
Peripheral nerve stimulator ▪ two electrode gel patches ▪ two leadwires ▪ alcohol pads ▪ Optional: clippers.
Implementation
Verify the doctor’s order for peripheral nerve stimulation.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.4
Explain the reasons for neuromuscular blockade and peripheral nerve stimulation to the patient and family to increase their understanding and reduce anxiety.
Select a site for electrode placement that’s accessible and is without edema, wounds, catheters, or dressings to ensure optimum placement. The preferred monitoring site is the ulnar nerve, but if it isn’t accessible, other sites may be used.
If the patient has excessive hair where an electrode is to be placed, remove the hair with clippers to improve contact of the pad with the skin.
Ulnar Nerve Stimulation
Clean the site on the patient’s arm where the electrodes are to be placed with an alcohol pad and allow it to dry to reduce skin resistance.
Place the patient’s arm in a relaxed position with the palm up so that the ulnar nerve is easily accessible.
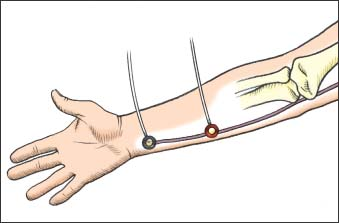
Place one electrode over the ulnar nerve at the crease of the wrist and the other electrode 1 to 2 cm away, parallel to the carpi ulnaris tendon (as shown below) to ensure stimulation of the ulnar nerve.
Attach the leadwires to the PNS.
Connect the black lead (negative) to the electrode nearest the wrist and the red lead (positive) to the electrode on the forearm.
Switch the PNS on and choose a low milliampere (mA)—commonly 10 mA to 20 mA—because higher current can cause overstimulation of the nerve and rhythmic nerve firing.
Press the TOF button to initiate the four impulses and count the number of twitches the stimulation produces. Visually count the number of thumb adductions or twitches while lightly feeling for twitches. Don’t count finger movement that’s caused by muscle stimulation.
Turn off the PNS.
Facial Nerve Stimulation
Clean the site on the patient’s face where the electrodes are to be placed with an alcohol pad and allow it to dry to reduce skin resistance.
Place one electrode near the outer canthus of the eye and a second electrode 2 cm below and at the level of the tragus of the ear (as shown below).
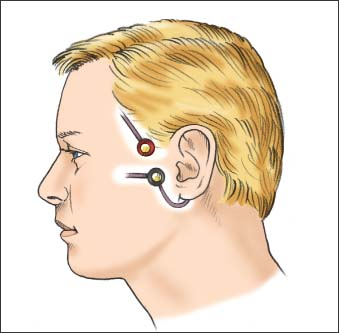
Attach the leadwires to the PNS and connect the black lead (negative) to the electrode nearest the tragus and the red lead (positive) to the electrode near the outer canthus of the eye.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
