Peptic Ulcer Disease
Despite a decreasing incidence since the 1950s, peptic ulcer disease (PUD) remains a serious health concern. In developing countries it is common among children, but in the United States it is rarely seen until after age 15. About 500,000 new cases are diagnosed each year in the United States; another 4 million individuals experience recurrence of the disease. Fifteen percent of the United States population is thought to be diagnosed with it at some point in their lives. PUD has a slightly higher frequency in males and peaks at age 50 and then again at about age 75.
Ulcers are a disruption in the gastric mucosa (stomach and/or duodenum) greater than 5 mm, causing chronic inflammation. Chronic ulcers can be found anywhere in the gastrointestinal tract and are named according to their location or etiology (gastric or stress ulcers). Peptic ulcer disease, however, refers to those occurring in the stomach or duodenum.
An ulcer begins as a superficial erosion of the mucosa that is then subjected to the presence of pepsin and hydrochloric acid. The acid erodes the tissue as it attempts to heal itself and forms scar tissue at the base of what is now a developing ulcer. There is a decreased incidence of duodenal ulcers due to the eradication of Helicobacter pylori.
An ulcer begins as a superficial erosion of the mucosa that is then subjected to the presence of pepsin and hydrochloric acid. The acid erodes the tissue as it attempts to heal itself and forms scar tissue at the base of what is now a developing ulcer. There is a decreased incidence of duodenal ulcers due to the eradication of Helicobacter pylori.
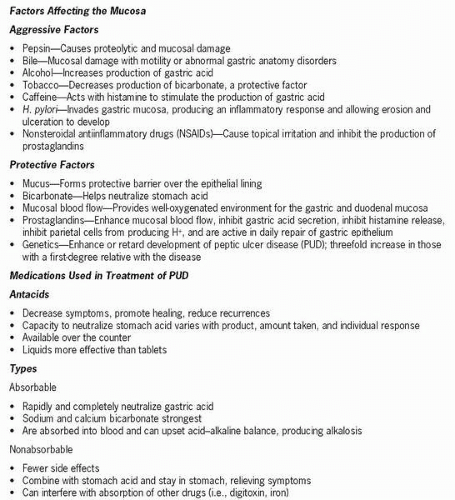
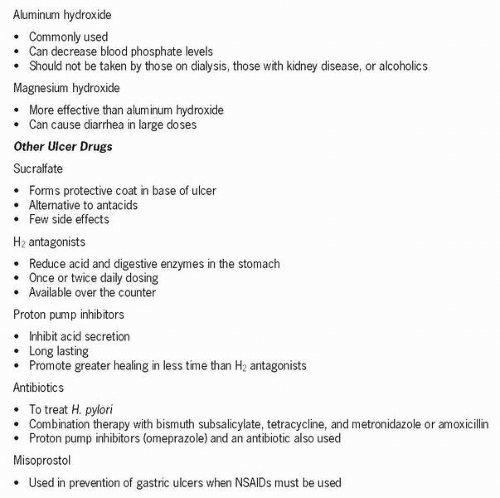
There are aggressive and defensive factors within the stomach and duodenum that balance each other to maintain a state of homeostasis. Aggressive forces are acid producers, whereas defensive forces are mucosal protectors. All people produce acid that is needed for digestion, but they can be separated into high, medium, or low acid producers. However, people who are high acid producers do not develop PUD at any greater rate than low acid producers. An imbalance between the aggressive and protective factors causes formation of an ulcer. Once considered a chronic disease, PUD is now thought to be caused by three major factors: H. pylori, nonsteroidal antiinflammatory drugs (NSAIDs), and Zollinger-Ellison syndrome. Other contributory risk factors include corticosteroid use, anticoagulants, cigarette smoking and alcohol abuse.
H. pylori
This microorganism is a small, curved, gram-negative rod with flagella found in 95% of patients with duodenal ulcers and in 75% with gastric ulcers. It is transmitted by an oral-oral or fecal-oral route. There are various strains of the organism, with some more virulent than others. Those acquiring a less virulent strain tend to develop gastritis rather than actual PUD. Infection with H. pylori does not always cause PUD to develop.
What triggers the organism’s attack on the mucosal lining is not known. It gains access to the gastric mucosa through the epithelial cells protecting it. In the mucosa the bacteria release toxins, stimulating an inflammatory response that causes tissue injury and the release of antibodies that can be detected in the blood or stool. The organism mainly invades the gastric mucosa, but it is unclear how it causes duodenal ulcers to form. It is presumed that the duodenum has patches of gastric
cells, which allows bacteria to colonize, or that excessive production of gastric acid in the stomach causes erosions, allowing the organism to take hold. Most people infected with H. pylori are asymptomatic, but their risk of developing gastric cancer is three to six times higher than noninfected people.
cells, which allows bacteria to colonize, or that excessive production of gastric acid in the stomach causes erosions, allowing the organism to take hold. Most people infected with H. pylori are asymptomatic, but their risk of developing gastric cancer is three to six times higher than noninfected people.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree