Oxygen Administration
A patient will need oxygen therapy when hypoxemia results from a respiratory or cardiac emergency or an increase in metabolic function.
In a respiratory emergency, oxygen administration enables the patient to reduce his ventilatory effort. When conditions such as atelectasis or acute respiratory distress syndrome impair diffusion, or when lung volumes are decreased from alveolar hypoventilation, this procedure boosts alveolar oxygen levels.
In a cardiac emergency, oxygen therapy helps meet the increased myocardial workload as the heart tries to compensate for hypoxemia. Oxygen administration is particularly important for a patient whose myocardium is already compromised—for instance, from a myocardial infarction or cardiac arrhythmia.
When metabolic demand is high (in cases of massive trauma, burns, or high fever, for instance) oxygen administration supplies the body with enough oxygen to meet its cellular needs. This procedure also increases oxygenation in the patient with a reduced blood oxygen-carrying capacity, perhaps from carbon monoxide poisoning or sickle cell crisis.
The adequacy of oxygen therapy is determined by arterial blood gas (ABG) analysis, oximetry monitoring, and clinical examinations. The patient’s disease, physical condition, and age help determine the most appropriate method of administration.
Equipment
The equipment needed depends on the type of delivery system ordered. (See Guide to oxygen delivery systems, pages 538 to 541.) Equipment includes selections from the following list: Oxygen source (wall unit, cylinder, liquid tank, or concentrator) ▪ flowmeter ▪ adapter, if using a wall unit, or a pressure-reduction gauge, if using a cylinder ▪ sterile humidity bottle and adapters ▪ sterile distilled water ▪ oxygen precaution sign ▪ appropriate oxygen delivery system (a nasal cannula, simple mask, or nonrebreather mask for low-flow and variable oxygen concentrations; a Venturi mask, aerosol mask, T tube, tracheostomy collar, tent, or oxygen hood for high-flow and specific oxygen concentrations) ▪ small-diameter or large-diameter connection tubing ▪ gauze pads and tape ▪ jet adapter for Venturi mask (if adding humidity) ▪ gloves ▪ stethoscope ▪ sphygmomanometer ▪ Optional: oxygen analyzer.
Preparation of Equipment
Although a respiratory therapist typically is responsible for setting up, maintaining, and managing the equipment, you’ll need a working knowledge of the oxygen system being used.
Guide to Oxygen Delivery Systems
Patients may receive oxygen through one of several administration systems. Each has its own benefits, drawbacks, and indications for use. The advantages and disadvantages of each system are compared below.
Nasal Cannula
Oxygen is delivered through plastic cannulas in the patient’s nostrils.
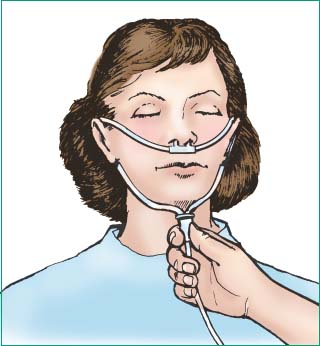 |
Advantages: Safe and simple; comfortable and easily tolerated; nasal prongs can be shaped to fit any face; effective for low oxygen concentrations; allows movement, eating, and talking; inexpensive and disposable.
Disadvantages: Can’t deliver concentrations higher than 40%7; can’t be used in complete nasal obstruction; may cause headaches or dry mucous membranes if flow rate exceeds 6 L/minute7; can dislodge easily.
Administration guidelines: Hook the cannula tubing behind the patient’s ears and under the chin. Slide the adjuster upward under the chin to secure the tubing. If using an elastic strap to secure the cannula, position it over the ears and around the back of the head. Avoid applying it too tightly, which can result in excess pressure on facial structures and cannula occlusion as well. With a nasal cannula, oral breathers achieve the same oxygen delivery as nasal breathers.
Simple Mask
Oxygen flows through an entry port at the bottom of the mask and exits through large holes on the sides of the mask.
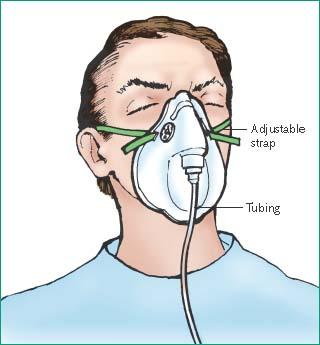 |
Advantages: Can deliver concentrations of 35% to 50%.7
Disadvantages: Hot and confining; may irritate patient’s skin; tight seal, which may cause discomfort, is required for higher oxygen concentration; interferes with talking and eating; impractical for long-term therapy because of imprecision.
Administration guidelines: Select the mask size that offers the best fit. Place the mask over the patient’s nose, mouth, and chin, and mold the flexible metal edge to the bridge of the nose. Adjust the elastic band around the head to hold the mask firmly but comfortably over the cheeks, chin, and bridge of the nose. For elderly or cachectic patients with sunken cheeks, tape gauze pads to the mask over the cheek area to try to create an airtight seal. Without this seal, room air dilutes the oxygen, preventing delivery of the prescribed concentration. A minimum of 5 L/minute is required in all masks to flush expired carbon dioxide from the mask so that the patient doesn’t rebreathe it.
Nonrebreather Mask
On inhalation, the one-way valve opens, directing oxygen from a reservoir bag into the mask. On exhalation, gas exits the mask through the one-way expiratory valve and enters the atmosphere. The patient only breathes gas from the bag.
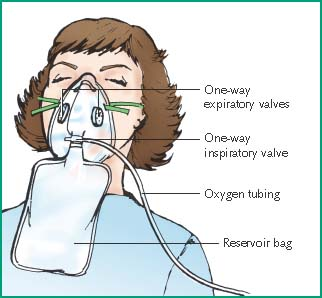 |
Advantages: Delivers the highest possible oxygen concentration (60% to 90%) short of intubation and mechanical ventilation; effective for short-term therapy; can be converted to a partial rebreather mask, if necessary, by removing the one-way valve.
Disadvantages: Requires a tight seal, which may be difficult to maintain and may cause discomfort; may irritate the patient’s skin; interferes with talking and eating; impractical for long-term therapy.
Administration guidelines: Follow procedures listed for the simple mask. Make sure that the mask fits very snugly and that the one-way valves are secure and functioning. Because the mask excludes room air, valve malfunction can cause carbon dioxide buildup and suffocate an unconscious patient. If the reservoir bag collapses more than slightly during inspiration, raise the flow rate until you see only a slight deflation. Marked or complete deflation indicates an insufficient flow rate. Keep the reservoir bag from twisting or kinking. Ensure free expansion by making sure the bag lies outside the patient’s gown and bedcovers.
CPAP Mask
This system allows the spontaneously breathing patient to receive continuous positive airway pressure (CPAP) with or without an artificial airway.
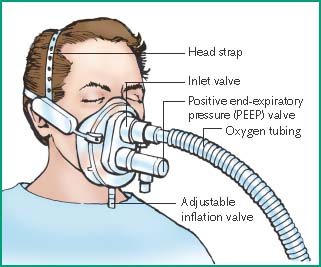 |
Advantages: Noninvasively improves arterial oxygenation by increasing functional residual capacity; allows the patient to avoid intubation; allows the patient to talk and cough without interrupting positive pressure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
