Osteoporosis
Osteoporosis is a disease of decreased bone mass and occurs when the rate of bone resorption exceeds the rate of bone formation. Approximately 10 million people have osteoporosis, but it is more common among the older adult female population, affecting one in three women and one in eight men. Osteopenia is a condition of bone thinning that leads to osteoporosis if not diagnosed.
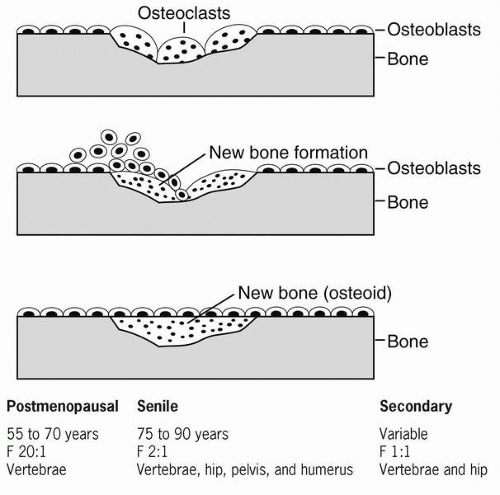 Figure 66-1 Bone remodeling and types of osteoporosis. |
There are two types of osteoporosis: Type I or primary osteoporosis is associated with postmenopausal estrogen loss but can also be contributed to as a result of not building necessary bone mass during the formative years. Secondary, or Type II, osteoporosis is due to some underlying disease or pathology or from certain medications. Osteoporosis can be due to either a decrease in activity of the osteoblasts, which are responsible for bone
formation, or an increase in activity of the osteoclasts, which are responsible for bone breakdown. It can be either regional or generalized. Early osteoporosis is asymptomatic, and considerable bone loss (30-50%) can occur before it is detectable on x-ray.
formation, or an increase in activity of the osteoclasts, which are responsible for bone breakdown. It can be either regional or generalized. Early osteoporosis is asymptomatic, and considerable bone loss (30-50%) can occur before it is detectable on x-ray.
 Osteoporosis can be due to either a decrease in activity of the osteoblasts, which are responsible for bone formation, or an increase in activity of the osteoclasts, which are responsible for bone breakdown.
Osteoporosis can be due to either a decrease in activity of the osteoblasts, which are responsible for bone formation, or an increase in activity of the osteoclasts, which are responsible for bone breakdown.Osteoporosis is more common in women than in men, with the peak incidence
in women beginning within 5 years of menopause. Estrogen influences bone density. When that source is decreased, cytokinins increase and stimulate osteoclast (bone breakdown) activity. In men, demineralization begins around the age of 65 to 70 due to a decrease in testosterone and other factors. Osteoporosis in males has less clinical significance because their bones are larger and denser than those of women. Men also do not have the influence of estrogen on their bones. The bone loss during menopause is due to an increase in osteoclastic activity, whereas that occurring with aging is mediated by a decrease in osteoblastic activity.
in women beginning within 5 years of menopause. Estrogen influences bone density. When that source is decreased, cytokinins increase and stimulate osteoclast (bone breakdown) activity. In men, demineralization begins around the age of 65 to 70 due to a decrease in testosterone and other factors. Osteoporosis in males has less clinical significance because their bones are larger and denser than those of women. Men also do not have the influence of estrogen on their bones. The bone loss during menopause is due to an increase in osteoclastic activity, whereas that occurring with aging is mediated by a decrease in osteoblastic activity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree