Orthodpedic Disorders
QUICK LOOK AT THE CHAPTER AHEAD
Developmental milestones can be affected in children with musculoskeletal disorders.
Orthopedic injuries in children are often caused by sports or recreation related activities.
Immobilization related to an orthopedic injury can impact psych-social, intellectual, and physical development in a child.
Injury to epiphyseal growth plates can arrest further growth in bones.
Infections in the bone can be difficult to treat and eradicate.
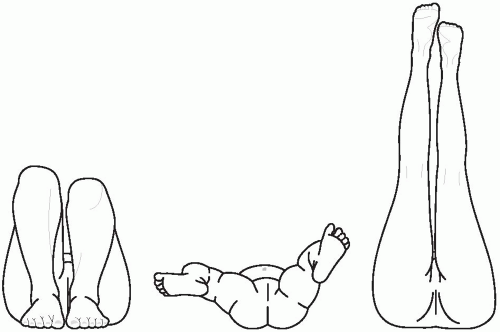
In the past the common term for a child born with a hip condition was congenital hip dysplasia. The current term of developmental dysplasia of the hip encompasses three conditions that may affect an infant at birth or shortly thereafter with dislocation, subluxation, or dysplasia of the hip (Figure 43-1). A dislocated hip occurs in 1 in 1,000 births, is usually unilateral, and occurs most often in females. The left hip is involved in 60% of cases.
Pathophysiology
Several factors influence the incidence of developmental dysplasia of the hip. Many hip dysplasias occur during the second or third trimester as a
result of fetal positioning. The left hip is involved more often because of intrauterine positioning of the fetus against the mother’s sacrum. Girls are more affected because it is thought that maternal levels of estrogen influence ligamentous laxity that females respond to differently. Developmental dysplasia of the hip is also more common in infants born in the breech position.
result of fetal positioning. The left hip is involved more often because of intrauterine positioning of the fetus against the mother’s sacrum. Girls are more affected because it is thought that maternal levels of estrogen influence ligamentous laxity that females respond to differently. Developmental dysplasia of the hip is also more common in infants born in the breech position.
A dislocated hip is one that is characterized by a complete loss of contact of the femoral head with the acetabulum, a dislocatable hip is one that can be manually displaced but returns to the acetabulum with release of pressure, and a subluxated hip is one where the femoral head remains in the acetabulum but comes partially out of the joint with manipulation.
In the infant two tests that may be done are the Barlow maneuver and the Ortolani test. These tests are most reliable within the first month of life. In the Barlow maneuver slight pressure is applied with the thumb on the medial side of the thigh as the thigh is adducted. A jerk is elicited as the hip dislocates. In the Ortolani test both hips are flexed and gently abducted and externally rotated. A click is heard as the dislocated head reduces into the acetabulum. There are several cardinal signs and symptoms that indicate an infant may have developmental dysplasia of the hip. They differ for the infant and older child (Table 43-1).
Treatment
Early detection and treatment are important to ensure that hip function is optimized. Treatment varies depending on age and extent of involvement. In the infant positional
casting, skin traction, or the Pavlik harness may be used. In the older child casting and traction may be tried initially to gently stretch the ligaments and tissue before a closed reduction being attempted. An open reduction may be necessary to correct the deformity, with a hip spica cast applied postoperatively.
casting, skin traction, or the Pavlik harness may be used. In the older child casting and traction may be tried initially to gently stretch the ligaments and tissue before a closed reduction being attempted. An open reduction may be necessary to correct the deformity, with a hip spica cast applied postoperatively.
Table 43-1 Differences in Clinical Manifestations of Developmental Dysplasia of the Hip | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
The three common pediatric curvatures of the spine are kyphosis, which is an increased convex curve, normally in the thoracic region; lordosis, which is an increased concave curve, normally in the lumbar region; and scoliosis, which is a lateral curvature of the spine. Each of these disorders may be classified as congenital, neuromuscular, or idiopathic. Many states now mandate school screening for curvatures of the spine in an effort to identify children early on and get treatment started. Idiopathic scoliosis occurs most often in girls and often presents during the preadolescent growth spurt. Young girls diagnosed with scoliosis are at an increased risk for osteopenia as they age. Curvatures of the spine may be associated with other pediatric chronic disorders such as spina bifida, cerebral palsy, and muscle diseases classified as neuromuscular.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree