Ommaya Reservoir Drug Infusion
Also known as a subcutaneous cerebrospinal fluid (CSF) reservoir, the Ommaya reservoir allows delivery of long-term drug therapy to the CSF by way of the brain’s ventricles. The reservoir spares the patient repeated lumbar punctures to administer chemotherapeutic drugs, analgesics, antibiotics, and antifungals. It’s most commonly used for chemotherapy and pain management, specifically for treating central nervous system (CNS) leukemia, malignant CNS disease, and meningeal carcinomatosis.
The reservoir is a mushroom-shaped silicone apparatus with an attached catheter. It’s surgically implanted beneath the patient’s scalp in the nondominant lobe, and the catheter is threaded into the ventricle through a burr hole in the skull. (See How the Ommaya reservoir works, page 522.) Besides providing convenient, comparatively painless access to CSF, the Ommaya reservoir permits consistent and predictable drug distribution throughout the subarachnoid space and CNS. It also allows for measurement of intracranial pressure (ICP).
Before reservoir insertion, the patient may receive a local or general anesthetic, depending on his condition and the doctor’s preference. After an X-ray confirms placement of the reservoir, a pressure dressing is applied for 24 hours, followed by a gauze dressing for another day or two. The sutures may be removed in about 10 days. However, the reservoir can be used within 48 hours to deliver drugs, obtain CSF pressure measurements, drain CSF, and withdraw CSF specimens.
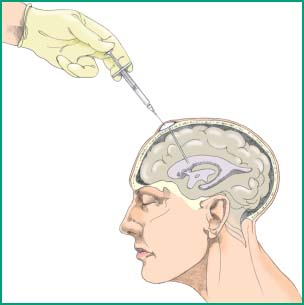
How the Ommaya Reservoir Works
To insert an Ommaya reservoir, the doctor drills a burr hole and inserts the device’s catheter through the patient’s nondominant frontal lobe into the lateral ventricle. The reservoir, which has a self-sealing silicone injection dome, rests over the burr hole under a scalp flap. This creates a slight, soft bulge on the scalp about the size of a quarter. Usually, drugs are injected into the dome with a syringe.
 |
The doctor usually injects drugs into the Ommaya reservoir, but a specially trained nurse may perform this procedure if allowed by facility policy and the state’s nurse practice act. This sterile procedure usually takes 15 to 30 minutes.
Equipment
Equipment varies but may include the following: Preservative-free prescribed drug ▪ personal protective equipment (sterile gloves, gown, mask, face shield, goggles) ▪ antiseptic solution (antiseptics containing alcohol or acetone should be avoided) ▪ sterile drape ▪ two 3-mL syringes ▪ 25G needle ▪ sterile gauze pad ▪ syringe containing preservative-free normal saline solution ▪ sterile label ▪ sterile marker ▪ CSF collection tubes.
For Chemotherapy
Powder-free chemotherapy gloves ▪ nonlinting, nonabsorbent disposable gown ▪ face shield ▪ National Institute for Occupational Safety and Health–approved respirator mask (if aerosolization is likely) ▪ syringes with luer-lock connector ▪ chemotherapy sharps container ▪ hazardous waste container approved for cytotoxic waste ▪ chemotherapy spill kit.
Preparation of Equipment
Make sure that a chemotherapy spill kit and emergency equipment are readily available if chemotherapy is being administered. Also ensure that the emergency equipment is functioning properly.
Implementation
Verify the doctor’s order in the patient’s medical record and medication administration record.1
Make sure that the doctor has obtained an informed consent and that the consent form is in the patient’s medical record.2,3
If administering a chemotherapeutic agent, become familiar with the information contained in the material safety data sheet specific to the prescribed drug.
In collaboration with the patient’s multidisciplinary team, review the patient’s test results, specifically the complete blood count, blood urea nitrogen level, platelet count, and liver function studies.
Check the patient’s medication history for drugs that might interact with the prescribed medication.
Determine whether the patient has received chemotherapy before and note the severity of any adverse effects.2
Determine if the doctor has ordered any premedications to combat adverse effects of the medication and administer them as prescribed, following safe medication administration practices.
Avoid distractions and interruptions when preparing and administering medication to prevent medication administration errors.4
Verify that the drug is properly labeled when you receive it from the pharmacy and that this information includes the patient’s full name and second identifier, full generic drug name, drug administration route, total dose to be given, total volume required to administer the dosage, date of administration, and the date and time of preparation and expiration. If the drug is a chemotherapeutic agent, make sure it also contains a label that clearly identifies the drug as hazardous. If you must prepare the drug yourself, make sure you label it properly.2,5
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
