Nasogastric Tube Insertion and Removal
Usually inserted to decompress the stomach, a nasogastric (NG) tube can prevent vomiting after major surgery. An NG tube is typically in place for 48 to 72 hours after surgery, by which time peristalsis usually resumes. It may remain in place for shorter or longer periods, however, depending on its use.
The NG tube has other diagnostic and therapeutic applications, especially in assessing and treating upper GI bleeding, collecting gastric contents for analysis, performing gastric lavage, aspirating gastric secretions, and administering medications and nutrients.
Inserting an NG tube requires close observation of the patient and verification of proper placement. The tube must be inserted with extra care in pregnant patients and in those with an increased risk of complications. For example, the doctor will order an NG tube for a patient with aortic aneurysm, myocardial infarction, gastric hemorrhage, or esophageal varices only if he believes that the benefits outweigh the risks of intubation.
Most NG tubes have a radiopaque marker or strip at the distal end so that the tube’s position can be verified by X-ray. If the position can’t be confirmed, the doctor may order fluoroscopy to verify placement.
The most common NG tubes are the Levin tube, which has one lumen, and the Salem sump tube, which has two lumens—one for suction and drainage and a smaller one for ventilation. Air flows through the vent lumen continuously, which protects the delicate gastric mucosa by preventing a vacuum from forming should the tube adhere to the stomach lining. (See Types of NG tubes.)
Equipment
For Insertion
Tube (usually #12, #14, #16, or #18 French for a normal adult) ▪ towel or linen-saver pad ▪ facial tissues ▪ emesis basin ▪ penlight ▪ 1″ hypoallergenic tape ▪ alcohol pad ▪ gloves ▪ water-soluble lubricant ▪ cup or glass of water with straw (if appropriate) ▪ pH test strip or carbon dioxide detector ▪ tongue blade ▪ catheter-tip or bulb syringe or irrigation set ▪ safety pin ▪ ordered suction equipment ▪ Optional: rubber band and safety pin, basin of ice or warm water.
For Removal
Stethoscope ▪ catheter-tip syringe ▪ normal saline solution ▪ towel or linen-saver pad ▪ adhesive remover ▪ gloves.
Preparation of Equipment
Inspect the NG tube for defects, such as rough edges or partially closed lumens. Then check the tube’s patency by flushing it with water. If you need to increase the tube’s flexibility to ease insertion, coil it around your gloved fingers for a few seconds or dip it in
warm water. If the tube is too flaccid, stiffen it by filling the tube with water and then freezing it1 or dipping the tube in ice water.
warm water. If the tube is too flaccid, stiffen it by filling the tube with water and then freezing it1 or dipping the tube in ice water.
Types of NG tubes
The doctor will choose the type and diameter of nasogastric (NG) tube that best suits the patient’s needs, including lavage, aspiration, enteral therapy, and stomach decompression. Choices may include the Levin and Salem sump tubes.
Levin Tube
The Levin tube is a rubber or plastic tube that has a single lumen, a length of 42″ to 50″ (106.5 to 127 cm), and holes at the tip and along the side.
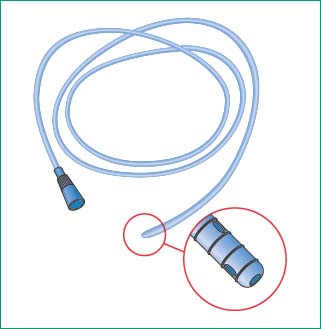 |
Salem Sump Tube
A Salem sump tube is a double-lumen tube that’s made of clear plastic and has a blue sump port (pigtail) that allows atmospheric air to enter the patient’s stomach. Thus, the tube floats freely and doesn’t adhere to or damage gastric mucosa. The larger port of this 48″ (122-cm) tube serves as the main suction conduit. The tube has openings at 45, 55, 65, and 75 cm as well as a radiopaque line to verify placement.
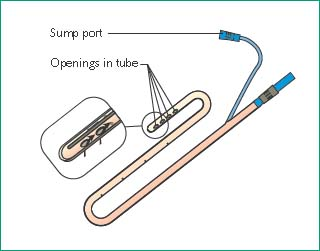 |
Implementation
Verify the doctor’s order.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.5
Explain the procedure to the patient to ease anxiety and promote cooperation. Inform her that she may experience some nasal discomfort, that she may gag, and that her eyes may water.
Agree on a signal that the patient can use if she wants you to stop briefly during the procedure.
Provide privacy and help the patient into high Fowler’s position unless contraindicated.
Drape the towel or linen-saver pad over the patient’s chest to protect her gown and bed linens from spills.
Inserting an NG tube
Place the facial tissues and emesis basin well within the patient’s reach.
Help the patient face forward with her neck in a neutral position.
Determine the length of the tube to be inserted to reach the stomach: hold the end of the tube at the tip of the patient’s nose (as shown below) and extend the tube to the patient’s earlobe and then down to the xiphoid process.

Mark this distance on the tubing with the tape. (Average measurements for an adult range from 22″ to 26″ [56 to 66 cm].) It may be necessary to add 2″ (5 cm) to this measurement in tall individuals to ensure entry into the stomach.
Determine which nostril will allow easier access; use a penlight and inspect for a deviated septum or other abnormalities. Ask the patient if she ever had nasal surgery or a nasal injury. Assess airflow in both nostrils by occluding one nostril at a time while the patient breathes through her nose. Choose the nostril with the better airflow. If the patient is able to respond, ask whether she has had an NG tube placed previously. If she has, then ask which nostril is better for insertion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
