Nasal Packing, Assisting
In the highly vascular nasal mucosa, even seemingly minor injuries can cause major bleeding and blood loss. When routine therapeutic measures, such as direct pressure, cautery, and vasoconstrictive drugs, fail to control epistaxis (nosebleed), the patient’s nose may have to be packed to stop anterior bleeding (which runs out of the nose) or posterior bleeding (which runs down the throat). If blood drains into the nasopharyngeal area or lacrimal ducts, the patient may also appear to bleed from the mouth and eyes.
Most nasal bleeding originates at a plexus of arterioles and venules in the anteroinferior septum. Only about 1 in 10 nosebleeds occurs in the posterior nose, which usually bleeds more heavily than the anterior location.
A nurse typically assists a doctor with anterior or posterior nasal packing. She may also assist with nasal balloon catheterization—a procedure that applies pressure to a posteior bleeding site.
Whichever procedure the patient undergoes, you should provide ongoing encouragement and support to reduce his discomfort and anxiety. You should also perform ongoing assessment to determine the procedure’s success and to detect possible complications.
Equipment
Gowns ▪ goggles ▪ masks ▪ sterile gloves ▪ sedative, as ordered ▪ clamp ▪ patient drape (towels, incontinence pads, or gown) ▪ nasal speculum and tongue depressors (may be in preassembled head and neck examination kit) ▪ directed illumination source (such as headlamp or strong flashlight) or fiber-optic nasal endoscope, light cables, and light source ▪ suction apparatus with sterile suction-connecting tubing and sterile nasal aspirator tip ▪ sterile bowl and sterile saline solution for flushing out suction apparatus ▪ sterile tray or sterile towels ▪ local anesthetic spray (topical 4% lidocaine) or vial of local anesthetic solution (such as 2% lidocaine or 1% to 2% lidocaine with epinephrine 1:100,000) ▪ 10-mL syringe with 22G 1½″ needle ▪ silver nitrate sticks ▪ topical nasal vasoconstrictor decongestant (such as 0.5% phenylephrine) ▪ sterile normal saline solution (1-g container and 60-mL syringe with luer-lock tip, or 5-mL bullets for moistening nasal tampons) ▪ equipment for measuring vital signs ▪ packages of 1½″ petroleum strip gauze ▪ two #14 or #16 French catheters with 30-mL balloon ▪ alcohol pad ▪ cotton-tipped applicators ▪ petroleum jelly ▪ additional medications, as ordered.
Preparation of Equipment
Gather all equipment at the patient’s bedside. Make sure the headlamp works. Plug in the suction apparatus if necessary or turn on the suction regulator. Connect the tubing from the collection
container to the suction source. Test the suction equipment to make sure it works properly.
container to the suction source. Test the suction equipment to make sure it works properly.
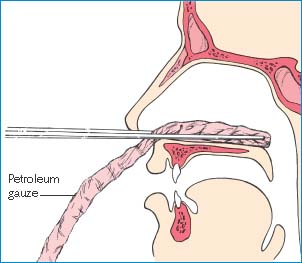
Inserting Anterior Nasal Packing
The doctor may treat an anterior nosebleed by packing the anterior nasal cavity with a 3″ to 4″ (7.5- to 10-cm) strip of antibiotic-impregnated petroleum gauze (as shown) or with a nasal tampon.
 |
A nasal tampon is made of tightly compressed absorbent material with or without a central breathing tube. The doctor inserts a lubricated tampon along the floor of the nose and, with the patient’s head tilted backward, instills 5 to 10 mL of antibiotic or normal saline solution, which causes the tampon to expand, stopping the bleeding. The tampon should be moistened periodically, and the central breathing tube should be suctioned regularly.
In a child or a patient with blood dyscrasias, the doctor may fashion an absorbable pack by moistening a gauzelike, regenerated cellulose material with a vasoconstrictor. Applied to a visible bleeding point, this substance will swell to form a clot. The packing is absorbable and doesn’t need removal.
Perform hand hygiene. At the bedside, create a sterile field. (Use the sterile towels or the sterile tray.) Using sterile technique, label all medications and solutions and place all sterile equipment on the sterile field.1
If the doctor will inject a local anesthetic rather than spray it into the nose, place the 22G 1½″ needle attached to the 10-mL syringe on the sterile field. When the doctor readies the syringe, clean the stopper on the anesthetic vial with an alcohol pad, and hold the vial so he can withdraw the anesthetic. This practice allows the doctor to avoid touching his sterile gloves to the nonsterile vial.
Open the packages containing the sterile suction-connecting tubing and aspirating tip, and place them on the sterile field. Fill the sterile bowl with normal saline solution so that the suction tubing can be flushed, as necessary. Thoroughly lubricate the posterior packing with antibiotic ointment.
Implementation
Verify the doctor’s order.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.2
Explain the procedure to the patient, answer questions, and offer reassurance to reduce his anxiety and promote cooperation.
Perform hand hygiene, put on sterile gloves and other personal protective equipment, and ensure that all people caring for the patient wear gowns, sterile gloves, and goggles during insertion of packing to prevent possible contamination from splattered blood.3,4,5
Check the patient’s vital signs, and observe for hypotension with postural changes. Hypotension suggests significant blood loss. Also monitor airway patency because the patient will be at risk for aspirating or vomiting swallowed blood.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
