patient attempts to look upward for a period of time. Pupillary response to light and accommodation remains normal.
TABLE 33-1 MYASTHENIA GRAVIS FOUNDATION OF AMERICA CLASSIFICATION5 | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||
deep tendon reflexes, coordination, or sensory perception. Confirmation of MG is based on results of the following tests: anticholinesterase test; ice-test; antibody titer for AChR, and MuSK; repetitive nerve stimulation; and single-fiber electromyography (EMG).6
Anticholinesterase testing: the drug commonly used is edrophonium chloride (Tensilon) because it has a rapid onset of 30 seconds and a short duration of about 5 to 10 minutes. The test is performed by drawing 10 mg of Tensilon into a syringe and administering 2 mg intravenously as a test dose. If no adverse symptoms appear, a subsequent dose of 3 to 8 mg is injected. If there is improvement in the muscle strength of a previously weak muscle that lasts 5 to 10 minutes, the test result is considered positive.
Ice-test: an ice-test is a bedside test with high sensitivity that is useful to differentiate MG from other similarly presenting conditions. The test is conducted by holding ice packs over the patient closed eyes for one minute and observing for resolution of ptosis. After application of the ice packs, the ptosis is markedly improved with a sustained effect of several minutes.7 An added advantage of this simple test is that treatment can be promptly initiated in response to a positive test.
Antibody titer for AChR: this is conducted by assay of blood. In 80% to 90% of patients with generalized myasthenia, the level of AChR antibody titer is elevated and in only in 55% of purely ocular myasthenia.8
Antibody titer for MuSK: this is conducted by assay of blood. In 40% of patients with AChR antibody negative generalized MG, this test is positive.9
Repetitive nerve stimulation: while electrical shocks are delivered to a nerve at the rate of 3 per second, surface electrodes over the muscle record electrical potentials. A rapid reduction of the amplitude of the muscle potential is considered positive.
Single-fiber EMG: this test can detect delay or failure of neuromuscular transmission in pairs of muscle fibers supplied by branches of a single nerve fiber. It is about 99% sensitive in confirming MG.
TABLE 33-2 IMMUNOSUPPRESSION IN MYASTHENIA GRAVIS
DRUG
DESCRIPTION
SIDE EFFECTS
Immediate Response
Intravenous immunoglobulin (IVIg)
2 g/kg administered over 5 days
Headache
Fluid overload
Rarely, renal failure
Intermediate: 1-3 Mos
Glucocorticoids (prednisone)
Begin low (15-25 mg/day) and increase stepwise up to maximum improvement or 50 mg/day
Optimal dose is maintained for 1-3 mos
Next, an alternate-day schedule is begun
Most patients need some form of chronic therapy
Peptic ulcer
Hyperglycemia
Fluid retention
Cyclophosphamide (Cytoxan) may be used with glucocorticoids
Rarely used except if unresponsive to other drugs
4-5 mg/kg/day in two divided doses
Hypertension
Nephrotoxicity
Response: Long-Term (Months to 1 Yr)
Azathioprine (Imuran) may be used with glucocorticoids
Used frequently after prednisone
Range: 2-3 mg/kg total body weight
Monitor white and red blood count
Works in 3-6 mos
Flu-like symptoms (fever, malaise)
Bone marrow depression
Hepatotoxicity
Anorexia, nausea, vomiting
Mycophenolate mofetil
1 g b.i.d.
Inhibits purine synthesis
Side effects rare
Diarrhea and leucopenia
Mediastinal CT or MRI: a CT or MRI of the mediastinal cavity may be ordered to determine whether the thymus gland is enlarged because many people with MG have a thymoma.
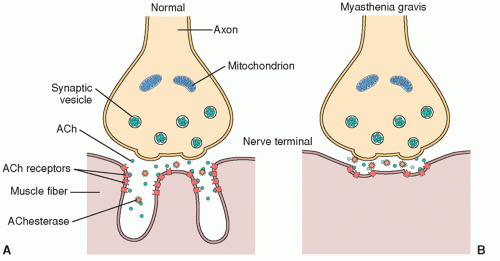
neuromuscular transmission of an impulse by preventing the degradation of ACh by the enzyme cholinesterase (ChE).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree