L
LANGUAGE DIFFICULTIES
Entering a health care facility or using a health care service can be a daunting experience for a person who doesn’t speak English. Nurses and other health care workers face similar obstacles to communication. A patient may be unable to communicate his questions, concerns, needs, and fears, and the nurse may be unable to perform a health history, ask about symptoms, or provide education. In fact, every part of the nurse-patient relationship may be compromised.
When a patient doesn’t speak English, you’ll need to find an interpreter. Interpreters may be found among staff members or family members. Telephone interpretation services are also available. Make sure that the patient trusts and approves of the family member. Be aware that the patient may not want to discuss his problems in front of family members and that family translators may be protective of the patient and may not relay all information. In some cultures, it may not be appropriate for a translator to discuss certain matters with members of the opposite sex. Failure to have a reliable translator can result in lack of informed consent and subsequent claims of false imprisonment, battery, or assault.
Essential documentation
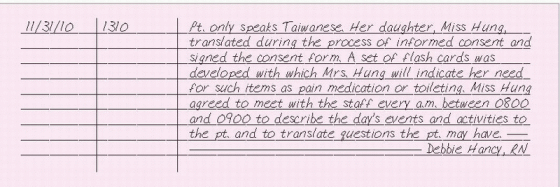
Document the primary language spoken by the patient. Include the names, addresses, and telephone numbers of family interpreters approved by the patient. Place in the patient’s chart a list of staff members approved by your facility to act as interpreters. When a translator is used for an
event, such as patient education, discharge instructions, or informed consent, record the name of the translator on the appropriate form or in your note. If a telephone interpretation service is used, record the call number assigned by the service for future reference. Describe alternative forms of communication used, such as a picture board or flash cards.
event, such as patient education, discharge instructions, or informed consent, record the name of the translator on the appropriate form or in your note. If a telephone interpretation service is used, record the call number assigned by the service for future reference. Describe alternative forms of communication used, such as a picture board or flash cards.
|
LAST WILL AND TESTAMENT, PATIENT REQUEST FOR WITNESS OF
A patient, especially one who believes he’s dying, may ask you to witness a last will and testament. In many states, a nurse can witness a patient’s signature on a will. However, you don’t have a legal or ethical responsibility to act as a witness. Check your facility’s policy or ask your facility’s legal consultant before you witness a will. (See Witnessing a will, page 236.)
If a patient asks you to be a witness when he draws his will, notify the doctor and your supervisor before you act as a witness. Don’t give any legal advice or offer assistance in wording the document. Don’t comment on the nature of the patient’s choices. Document your actions in your nurse’s note.
Essential documentation
When you witness a written will, document that it was signed and witnessed, who signed and witnessed it, who was present, what was done with it after signing, and what the patient’s condition was at the time. Document the name of the doctor, facility attorney, or any other person (such as the nursing supervisor) who was notified, and note the time of notification. Record instructions that were given and your actions. Record that
you heard the maker of the will declare it to be his will and that all witnesses and the maker of the will were actually present during the signing.
you heard the maker of the will declare it to be his will and that all witnesses and the maker of the will were actually present during the signing.
 WITNESSING A WILL
WITNESSING A WILLIn many states,your signature on a will certifies that:
you witnessed the signing of the will
you heard the maker of the will declare it to be his will
all witnesses and the maker of the will were actually present during the signing.
By attesting to the last two facts, you help ensure the authenticity of the will and the signatures. However, your signature doesn’t certify that the maker of the will is competent.
Before you sign any document, read at least enough of it to make sure it’s the type of document the maker represents it to be. Usually you won’t have to read all the text and, legally, that isn’t necessary for your signature to be valid. You should, however, always examine the document’s title and first page and give careful attention to what’s written immediately above the place for your signature.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access