Kidney Transplantation
Ranking among the most commonly performed and most successful of all organ transplantations, kidney transplantation represents an alternative to dialysis for many patients with otherwise unmanageable end-stage renal disease. It also may be necessary to sustain life in a patient who has suffered traumatic loss of kidney function or in whom dialysis is contraindicated. Kidney transplantation, however, isn’t performed on all patients who seemingly could benefit from it. For instance, severely debilitated, diabetic, or elderly patients or those with human immunodeficiency virus infection or psychiatric disorders aren’t considered good candidates.
In this transplantation procedure, a healthy kidney harvested from a living donor or cadaver donor is implanted in the recipient’s iliac fossa and anastomosed in place. The recipient’s own kidneys usually aren’t removed unless they’re chronically infected, greatly enlarged, cancerous, or causing intractable hypertension. Because the recipient’s own kidneys often secrete the hormone erythropoietin, they’re left in place to increase circulating hematocrit levels, relieve anemia, and reduce blood transfusion requirements in case of transplant rejection.
Procedure
With the patient under general anesthesia, the surgeon makes a curvilinear incision in the right or left lower quadrant, extending from the symphysis pubis to the anterior superior iliac spine and up to just below the thoracic cage. He exposes the iliac fossa with a self-retaining retractor, then performs segmental separation, ligature, and division of perivascular tissue. Next, he clamps the iliac vein and artery in preparation for anastomosis to the donor kidney’s renal vein and artery.
Meanwhile, the donor kidney is prepared for transplantation. If a cadaver kidney is being used, it’s removed from cold storage or a perfusion preparation machine. Kidneys can be stored for 72 hours, although most transplantations are done within 48 hours.
If the kidney is from a living donor, it’s harvested in an adjacent operating room via nephrectomy and placed in cold lactated Ringer’s solution. Before transplantation, the donor kidney’s renal artery is flushed with cold heparinized lactated Ringer’s solution to prevent clogging. Then, the surgeon positions the kidney in a sling over the implantation site.
The surgeon then implants the kidney in the retroperitoneal area of the iliac fossa, where it’s protected by the hip bone. If a donor’s left kidney is being used, the surgeon implants it in the recipient’s right side; conversely, he implants a donor’s right kidney in the recipient’s left side. Doing so permits the renal pelvis to rest anteriorly and allows the new kidney’s ureter to rest in front of the iliac artery, where the ureter is more accessible.
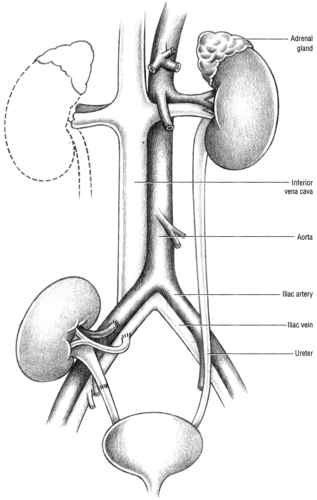
When the kidney is in place, the surgeon anastomoses its renal vein to the recipient’s iliac vein and the renal artery to the recipient’s internal iliac artery. (See Understanding kidney transplant.) He then removes the venous and arterial clamps and checks for patency of the anastomoses. Next, he attaches the donor kidney’s ureter to the recipient’s bladder, taking care to ensure a watertight closure. When the transplantation is complete, the surgeon sutures the incision and sends the patient to the recovery room.
Complications
The major impediment to transplantation is rejection of the donated organ. However, careful tissue matching between donor and recipient decreases this risk. (See Managing transplant rejection, page 508.)
Kidney transplantation may also be associated with vascular complications—such as stenosis of the renal artery, vascular
leakage, and thrombosis at the surgical site—or genitourinary tract complications—such as ureteral leakage, ureteral fistula, ureteral obstruction, calculus formation, bladder neck contracture, scrotal swelling, and graft rupture. Cardiovascular complications include hypertension, arrhythmias, heart failure, and increased plasma erythropoietin level. Respiratory complications include pneumonia, pulmonary edema, pulmonary emboli, and reactivated tuberculosis. Hepatitis B, cirrhosis (associated with azathioprine therapy), peptic ulcers, and increased histamine levels can occur. Other potential complications include infection, hematomas, abscesses, lymphoceles, steroid-induced diabetes mellitus, osteoporosis, myopathy, aseptic bone necrosis, cataracts, glaucoma, and retinitis.
leakage, and thrombosis at the surgical site—or genitourinary tract complications—such as ureteral leakage, ureteral fistula, ureteral obstruction, calculus formation, bladder neck contracture, scrotal swelling, and graft rupture. Cardiovascular complications include hypertension, arrhythmias, heart failure, and increased plasma erythropoietin level. Respiratory complications include pneumonia, pulmonary edema, pulmonary emboli, and reactivated tuberculosis. Hepatitis B, cirrhosis (associated with azathioprine therapy), peptic ulcers, and increased histamine levels can occur. Other potential complications include infection, hematomas, abscesses, lymphoceles, steroid-induced diabetes mellitus, osteoporosis, myopathy, aseptic bone necrosis, cataracts, glaucoma, and retinitis.
Understanding kidney transplant
In kidney transplant, the donated organ is implanted in the iliac fossa. The organ’s vessels are then connected to the internal iliac vein and internal iliac artery, as shown in the illustration. Typically, the patient’s own kidneys are left in place.
 Nursing priority
Nursing priorityManaging transplant rejection
Transplant rejection can occur immediately after surgery or years later. If rejection occurs, it demands prompt intervention.
Hyperacute rejection
In hyperacute rejection, the patient’s circulating antibodies attack the donor kidney several minutes to hours after transplantation. Renal perfusion plummets, and the organ rapidly becomes ischemic and dies.
If the patient experiences hyperacute rejection, prepare him for removal of the rejected kidney. Provide emotional support to help lessen his disappointment. If possible, provide support for the donor, who may also be distressed.
Get Clinical Tree app for offline access