Intrapleural Drug Administration
An intrapleural drug is injected through the chest wall into the pleural space or instilled through a chest tube placed intrapleurally for drainage. Doctors use intrapleural administration to promote analgesia, treat spontaneous pneumothorax, resolve pleural effusions, and administer chemotherapy.
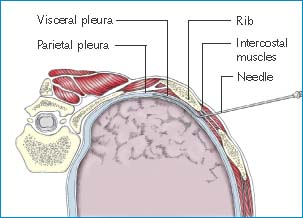
Intrapleurally administered drugs diffuse across the parietal pleura and innermost intercostal muscles to affect the intercostal nerves. During intrapleural injection of a drug, the needle passes through the intercostal muscles and parietal pleura on its way to the pleural space.
Drugs commonly given by intrapleural injection include tetracycline, streptokinase, anesthetics, and chemotherapeutic agents (to treat malignant pleural effusion or lung adenocarcinoma).
Contraindications for this route include pleural fibrosis or adhesions, which interfere with diffusion of the drug to the intended site; pleural inflammation; sepsis; and infection at the puncture site. Patients with bullous emphysema and those receiving respiratory therapy using positive end-expiratory pressure also shouldn’t have intrapleural injections because the injections may exacerbate an already compromised pulmonary condition.
Equipment
If a patient has emphysema, pleural effusion, or pneumothorax, an intrapleural drug is given through either a #16 to #20 or a #28 to #40 chest tube. Otherwise, it’s given through a 16G to 18G blunt-tipped intrapleural (epidural) needle and catheter. Accessory equipment depends on the type of access device the doctor uses. All equipment must be sterile.
For Intrapleural Catheter Insertion
Sterile gloves ▪ sterile cap ▪ sterile mask ▪ sterile gown ▪ sterile gauze ▪ antiseptic solution ▪ sterile drape ▪ local anesthetic, such as 1% lidocaine ▪ 3- to 5-mL syringe with 22G 1″ and 25G 5/8″ needles ▪ 18G needle or scalpel ▪ saline-lubricated glass syringe ▪ sterile dressings ▪ sutures ▪ tape ▪ blunt-tipped intrapleural needle ▪ intrapleural catheter.
For Chest Tube Insertion
Sterile towels ▪ sterile gloves ▪ sterile cap ▪ sterile mask ▪ sterile gown ▪ sterile gauze ▪ antiseptic solution ▪ 3- to 5-mL syringe ▪ local anesthetic, such as 1% lidocaine ▪ 18G needle or scalpel ▪ chest tube with or without trocar (#16 to #20 catheter for air or serous fluid; #28 to #40 for blood, pus, or thick fluid) ▪ two rubber-tipped clamps, if necessary ▪ sutures ▪ sterile drain dressings ▪ tape ▪ thoracic drainage system and tubing.
For Drug Administration
Sterile gloves ▪ sterile gauze pads ▪ antiseptic solution ▪ prescribed medication ▪ appropriate-sized needles and syringes ▪ 1% lidocaine, if necessary ▪ infusion pump ▪ sterile dressings ▪ tape ▪ two rubber-tipped clamps, if necessary.
For Chemotherapy Administration
Nonlinting, nonabsorbent disposable gown ▪ sterile powder-free chemotherapy gloves ▪ face shield ▪ National Institute for Occupational Safety and Health–approved respirator mask (if aerosolization is likely) ▪ antiseptic solution ▪ prescribed chemotherapeutic medication ▪ sterile gauze pads ▪ infusion pump with programmable dosing limits ▪ syringe with a luer-lock connector ▪ administration set ▪ spill kit ▪ hazardous waste receptacle.
Preparation of Equipment
When administering chemotherapy, make sure a spill kit is readily available to clean up spills immediately should they occur.
Implementation
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.4
Explain the procedure to the patient to allay his fears. Encourage him to follow instructions.
Perform hand hygiene and put on sterile gloves and other protective equipment as appropriate.1,2,3,7
Make sure that the insertion site is marked to prevent inserting the catheter in the incorrect location.
Conduct a time-out immediately before starting the procedure to perform a final assessment that the correct patient, site, positioning, and procedure are identified and, as applicable, all relevant information and necessary equipment are available.8
Inserting an Intrapleural Catheter
The doctor inserts the intrapleural catheter at the patient’s bedside with the nurse assisting.
Position the patient on his side with the affected side up. The doctor will insert the catheter into the fourth to eighth intercostal space, 3″ to 4″ (7.5 to 10 cm) from the posterior midline. (See Inserting an intrapleural catheter.)
The doctor puts on a sterile cap, gown, and mask and sterile gloves, cleans around the puncture site with an antiseptic-soaked gauze pad and allows it to dry, and then covers the area with a sterile drape. Next, he fills the 3- to 5-mL syringe with local anesthetic and injects it into the skin and deep tissues.
The doctor punctures the skin with the 18G needle or scalpel, which helps the blunt-tipped intrapleural needle penetrate the skin over the superior edge of the lower rib in the chosen interspace. Keeping the bevel tilted upward, he directs the needle medially at a 30- to 40-degree angle to the skin. When the needle tip punctures the posterior intercostal membrane, he removes the stylet and attaches a saline-lubricated glass syringe containing 2 to 4 mL of air to the needle hub.
During puncture, tell the patient to hold his breath (or momentarily disconnect him from mechanical ventilation) until the needle is removed. Doing so helps prevent the needle from injuring lung tissue.
The doctor advances the needle slowly. When the needle punctures the parietal pleura, negative intrapleural pressure moves the plunger outward. He then removes the syringe from the needle and threads the intrapleural catheter through the needle until he has advanced it about 2″ (5 cm) into the pleural space. Without removing the catheter, he carefully withdraws the needle.
Tell the patient that he can breathe again (or reconnect mechanical ventilation).
Blood in the needle means that the catheter probably is misplaced in a blood vessel, and aspirated air means that it’s probably in a lung. The doctor will then order a chest X-ray to verify placement and to detect such complications as pneumothorax.
Apply a sterile occlusive dressing over the insertion site to prevent catheter dislodgment. Label the dressing with the date, the time, and your initials. Obtain the patient’s vital signs every 15 minutes for the first hour after the procedure and then as needed.
Perform a comprehensive pain assessment using techniques appropriate for the patient’s age, condition, and ability to understand and respond appropriately.9
Inserting an Intrapleural Catheter
In intrapleural administration, the doctor injects a drug into the pleural space using a catheter.
Help the patient lie on one side with the affected side up. The doctor inserts a needle into the fourth to eighth intercostal space, 3” to 4” (7.5 to 10 cm) from the posterior midline. He then advances the needle medially over the superior edge of the patient’s rib through the intercostal muscles until it tangentially penetrates the parietal pleura (as shown). The catheter is advanced into the pleural space through the needle, which is then removed.
 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
