Intracranial Pressure Monitoring
Intracranial pressure (ICP) monitoring measures pressure exerted by the brain, blood, and cerebrospinal fluid (CSF) against the inside of the skull. Indications for monitoring ICP include head trauma with bleeding or edema, overproduction or insufficient absorption of CSF, cerebral hemorrhage, and space-occupying brain lesions. ICP monitoring can detect elevated ICP early, before clinical danger signs develop.1 Prompt intervention can then help avert or diminish neurologic damage caused by cerebral hypoxia and shifts of brain mass.
The four basic ICP monitoring systems are intraventricular catheter, subarachnoid bolt, epidural or subdural sensor, and intraparenchymal pressure monitoring. (See Understanding ICP monitoring, pages 404 and 405.) Regardless of which system is used, the procedure is typically performed by a neurosurgeon in the operating room, emergency department, or intensive care unit. Insertion of an ICP monitoring device requires sterile technique to reduce the risk of central nervous system (CNS) infection. Setting up equipment for the monitoring systems also requires strict asepsis.1
Equipment
Monitoring unit and transducers as ordered ▪ sterile 4″ × 4″ gauze pads ▪ linen-saver pads ▪ electric clippers ▪ sterile drapes ▪ povidone-iodine solution ▪ sterile gown ▪ surgical mask ▪ gloves ▪ sterile gloves ▪ sterile marker ▪ sterile labels ▪ head dressing supplies (two rolls of 4″ elastic gauze dressing, one roll of 4″ roller gauze, adhesive tape) ▪ Optional: suction apparatus, IV pole.
You may need to gather other equipment as instructed by the doctor, such as the drill and bits, scalp retractor, and a scalp staple.
Preparation of Equipment
Various types of preassembled ICP monitoring units are available, each with its own setup protocols. These units are designed to reduce the risk of infection by eliminating the need for multiple stopcocks, manometers, and transducer dome assemblies. When preparing the equipment, label all medications, medication containers, and other solutions on and off the sterile field.2 Some facilities use units that have miniaturized transducers rather than transducer domes.
Monitoring units and setup protocols are varied and complex and differ among health care facilities. Check your facility’s guidelines for your particular unit.
Implementation
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.6
Explain the procedure to the patient or his family.
Make sure that an informed consent has been obtained and documented in the medical record.7
Provide privacy if the procedure is being done in an open emergency department or intensive care unit.
Conduct a preprocedure verification process to make sure that all relevant documentation, related information, and equipment are available and correctly identified to the patient identifiers.8
Verify that the laboratory and imaging studies have been completed as ordered and that the results are in the patient’s medical record. Notify the doctor of any unexpected results.8
Obtain baseline routine and neurologic vital signs to aid in prompt detection of decompensation during the procedure.1
Understanding ICP Monitoring
Intracranial pressure (ICP) can be monitored using one of four systems.
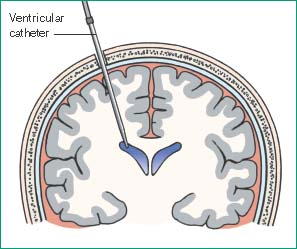
Intraventricular Catheter Monitoring
In this procedure, which monitors ICP directly, the doctor inserts a small polyethylene or silicone rubber catheter into the lateral ventricle through a burr hole.
Although this method measures ICP most accurately, it carries the greatest risk of infection. This is the only type of ICP monitoring that allows evaluation of brain compliance and drainage of significant amounts of cerebrospinal fluid (CSF).
Contraindications usually include stenotic cerebral ventricles, cerebral aneurysms in the path of catheter placement, and suspected vascular lesions.
 |
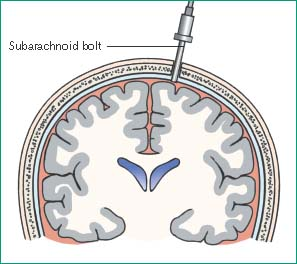
Subarachnoid Bolt Monitoring
This procedure involves insertion of a special bolt into the subarachnoid space through a twist-drill burr hole that’s positioned in the front of the skull behind the hairline.
Placing the bolt is easier than placing an intraventricular catheter, especially if a computed tomography scan reveals that the cerebrum has shifted or the ventricles have collapsed. This type of ICP monitoring also carries less risk of infection and parenchymal damage because the bolt doesn’t penetrate the cerebrum.
 |
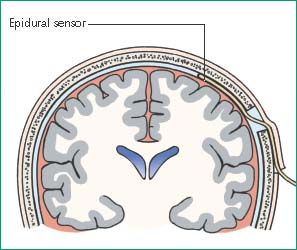
Epidural or Subdural Sensor Monitoring
ICP can also be monitored from the epidural or subdural space. For epidural monitoring, a fiber-optic sensor is inserted into the epidural space through a burr hole. This system’s main drawback is its questionable accuracy because ICP isn’t being measured directly from a CSF-filled space.
For subdural monitoring, a fiber-optic transducer-tipped catheter is tunneled through a burr hole, and its tip is placed on brain tissue under the dura mater. The main drawback to this method is its inability to drain CSF.
 |
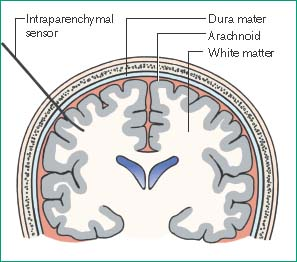
Intraparenchymal Pressure Monitoring
In this procedure, the doctor inserts a catheter through a small subarachnoid bolt and, after puncturing the dura mater, advances the catheter a few centimeters into the brain’s white matter. There’s no need to balance or calibrate the equipment after insertion.
Although this method doesn’t provide direct access to CSF, measurements are accurate because brain tissue pressures correlate well with ventricular pressures. Intraparenchymal monitoring may be used to obtain ICP measurements in patients with compressed or dislocated ventricles.
 |
Place the patient in the supine position, and elevate the head of the bed 30 degrees (or as ordered).1
Place linen-saver pads under the patient’s head. Clip his hair at the insertion site, as indicated by the doctor, to decrease the risk of infection. Carefully fold and remove the linen-saver pads to avoid spilling loose hair onto the bed.
Drape the patient with sterile drapes.
Verify that the insertion site has been identified before preparing the site. Doing so will minimize the risk of preparing the wrong area.9 Then scrub the insertion site for 2 minutes with antiseptic solution.
The doctor puts on the sterile gown, mask, and sterile gloves.
Make sure a time-out is conducted immediately before the doctor starts the procedure to identify the correct patient, site, positioning, and procedure and to ensure that all relevant information and necessary equipment is available.10
The doctor opens the interior wrap of the sterile supply tray and proceeds with insertion of the catheter or bolt.
To facilitate placement of the device, hold the patient’s head in your hands or attach a long strip of 4″ roller gauze to one side rail, and bring it across the patient’s forehead to the opposite rail. Reassure the conscious patient to help ease his anxiety. Talk to him frequently to assess his level of consciousness (LOC) and detect signs of deterioration. Watch for cardiac arrhythmias and abnormal respiratory patterns.
After insertion, remove and discard your gloves. Perform hand hygiene,3,4,5 put on sterile gloves, clean around the insertion site with antiseptic solution, and apply a sterile dressing to the site.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
