Intra-Aortic Balloon Counterpulsation
Providing temporary support for the heart’s left ventricle, intra-aortic balloon counterpulsation (IABC) mechanically displaces blood within the aorta by means of an intra-aortic balloon attached to an external pump console. The balloon is usually inserted through the common femoral artery and positioned with its tip just distal to the left subclavian artery. When used correctly, IABC improves two key aspects of myocardial physiology: it increases the supply of oxygen-rich blood to the myocardium, and it decreases myocardial oxygen demand and consumption.
IABC is recommended for patients with a wide range of low-cardiac-output disorders or cardiac instability, including refractory anginas, ventricular arrhythmias associated with ischemia, pump failure caused by cardiogenic shock, intraoperative myocardial infarction (MI), or low cardiac output after bypass surgery. IABC is also indicated for patients with low cardiac output secondary to acute mechanical defects after MI (such as ventricular septal defect, papillary muscle rupture, or left ventricular aneurysm).
Perioperatively, the technique is used to support and stabilize patients with a suspected high-grade lesion who are undergoing such procedures as angioplasty, thrombolytic therapy, cardiac surgery, and cardiac catheterization.
IABC is contraindicated in patients with end-stage renal disease, irreversible brain damage, severe aortic regurgitation, aortic aneurysm, or severe peripheral vascular disease.
The doctor removes the balloon when the patient’s hemodynamic status remains stable after the frequency of balloon augmentation is decreased.
Equipment
For assisting with insertion
IABC console and balloon catheters ▪ insertion kit ▪ Dacron graft (for a surgically inserted balloon) ▪ electrocardiogram (ECG) monitor and electrodes ▪ IV solution and infusion set ▪ sedative ▪ arterial line catheter ▪ temporary pacemaker setup ▪ 18G angiography needle ▪ sterile drape ▪ sterile gloves ▪ gown ▪ mask ▪ sutures ▪ suction setup ▪ oxygen setup and ventilator, if necessary ▪ defibrillator and emergency medications ▪ fluoroscope ▪ indwelling urinary catheter ▪ urinometer ▪ arterial blood gas (ABG) kits and tubes for laboratory studies ▪ antiseptic solution ▪ clippers.
For Maintaining the IABC
IABC console and balloon catheters ▪ ECG monitor and electrodes ▪ IV solution ▪ arterial line tubing, transducer, and pressure bag or device ▪ suction setup ▪ oxygen ▪ thermometer ▪ stethoscope ▪ emergency equipment and medications ▪ ABG kits and tubes for laboratory studies ▪ dressing materials ▪ gloves.
For Assisting with Removal
Dressing materials ▪ gloves ▪ suture removal kit.
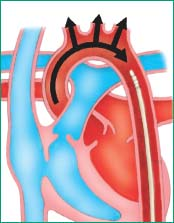
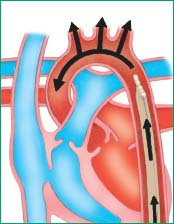
How the Intra-Aortic Balloon Pump Works
Made of polyurethane, the intra-aortic balloon is attached to an external pump console by means of a large-lumen catheter. These illustrations show the direction of blood flow when the pump inflates and deflates the balloon.
Balloon Inflation
The balloon inflates as the aortic valve closes and diastole begins. The balloon inflation displaces blood superiorly, which, in turn, augments coronary artery blood flow.
 |
Preparation of Equipment
When assisting with insertion, you or a perfusionist must zero and balance the pressure transducer in the external pump console and calibrate the oscilloscope monitor to ensure accuracy depending on your facility’s policy.
When maintaining IABC, have the defibrillator, the suction setup, the temporary pacemaker setup, and emergency medications readily available in case the patient develops severe complications.
Implementation
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.4
For Assisting with Insertion
Reinforce the doctor’s explanation of the procedure, explaining that the doctor will place a special balloon catheter in the patient’s aorta to help his heart pump more easily. Briefly explain the insertion procedure, and mention that the catheter will be connected to a large console next to his bed. Tell him that the balloon will temporarily reduce his heart’s workload to promote rapid healing of the ventricular muscle. Let him know that it will be removed after his heart can resume an adequate workload. (See How the intra-aortic balloon pump works.)
Confirm that a written consent is obtained and that the consent is in the patient’s medical record.5,6
Conduct a pre-procedure verification process to make sure that all relevant documentation, related information, or equipment is available and correctly identified to the patient’s identifiers.7
Make sure the patient has an arterial line for withdrawing blood samples, monitoring blood pressure, and assessing the timing and effectiveness of therapy; a pulmonary artery catheter to allow measurement of pulmonary artery pressure (PAP), aspiration of blood samples, and cardiac output studies (increased PAP indicates increased myocardial workload and ineffective balloon pumping); and a peripheral IV catheter or central venous access device in place for administering fluids and medications.
Obtain the patient’s baseline vital signs. Attach the patient to an ECG machine for continuous monitoring. Be sure to apply chest electrodes in a standard lead II position—or in whatever position produces the largest R wave—because the R wave triggers balloon inflation and deflation. Obtain a baseline ECG.
Attach another set of ECG electrodes to the patient unless the ECG pattern is being transmitted from the patient’s bedside monitor to the balloon pump monitor through another cable.
Administer oxygen, as ordered and as necessary.
Insert an indwelling catheter so you can measure the patient’s urine output and assess his fluid balance and renal function.
To reduce the risk of infection, clip hair bilaterally from the lower abdomen to the lower thigh, including the pubic area.
Observe and record the patient’s peripheral leg pulse and document sensation, movement, color, and temperature of the legs.
Administer a sedative, as ordered, following safe medication administration practices.9
Have the defibrillator, suction setup, temporary pacemaker setup, and emergency medications readily available in case the patient develops complications (such as arrhythmia) during insertion.
Perform hand hygiene and then put on a cap, mask, gown, and sterile gloves to comply with maximal barrier precautions during insertion.1,2,3,8
Before the doctor inserts the balloon, he puts on a surgical cap, sterile gloves, a gown, and a mask following maximal barrier precautions. He cleans the site with antiseptic solution and drapes
the patient using a sterile drape and observing maximal barrier precautions.
Conduct a time-out immediately before starting the procedure to determine that the correct patient, site, positioning, and procedure are identified and to confirm, as applicable, that relevant information and necessary equipment are available.10
Inserting the Intra-Aortic Balloon Percutaneously
The doctor may insert the balloon percutaneously through the femoral artery into the descending thoracic aorta using a modified Seldinger technique. First, he accesses the vessel with an 18G angiography needle and removes the inner stylet.
Then he passes the guide wire through the needle and removes the needle.
After passing a #8 French vessel dilator over the guide wire into the vessel, he removes the vessel dilator, leaving the guide wire in place.
Next, the doctor passes an introducer (dilator and sheath assembly) over the guide wire into the vessel until about 1″ (2.5 cm) remains above the insertion site. He then removes the inner dilator, leaving the introducer sheath and guide wire in place.
After passing the balloon over the guide wire into the introducer sheath, the doctor advances the catheter into position, 3/8″ to ¾″ (1 to 2 cm) distal to the left subclavian artery under fluoroscopic guidance.
The doctor attaches the balloon to the control system to initiate counterpulsation. The balloon catheter then unfurls.
Inserting the Intra-Aortic Balloon Surgically
If the doctor chooses not to insert the catheter percutaneously, he usually inserts it by femoral arteriotomy.
After making an incision and isolating the femoral artery, the doctor attaches a Dacron graft to a small opening in the arterial wall.
He then passes the catheter through this graft. Using fluoroscopic guidance as necessary, he advances the catheter up the descending thoracic aorta and places the catheter tip between the left subclavian artery and the renal arteries.
The doctor sews the Dacron graft around the catheter at the insertion point and connects the other end of the catheter to the pump console. (See Surgical insertion sites for the intra-aortic balloon.)
Completing the Procedure
Discard used supplies, remove and discard your personal protective equipment, and perform hand hygiene.1,2,3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access