Internal Fixation Management
In internal fixation, also known as surgical reduction or open reduction–internal fixation, the doctor implants fixation devices to stabilize the fracture. Internal fixation devices include nails, screws, pins, wires, and rods, all of which may be used in combination with metal plates. These devices remain in the body indefinitely unless the patient experiences adverse reactions after the healing process is complete. (See Reviewing internal fixation devices.)
Typically, internal fixation is used to treat fractures of the face and jaw, spine, and arms and legs as well as fractures involving a joint (most commonly, the hip). Internal fixation permits earlier mobilization and can shorten hospitalization, particularly in elderly patients with hip fractures.
Nursing management for a patient who undergoes internal fixation involves monitoring neurovascular status, administering
medications, managing the patient’s pain, preventing infection, and assisting with ambulation and exercises.
medications, managing the patient’s pain, preventing infection, and assisting with ambulation and exercises.
Reviewing Internal Fixation Devices
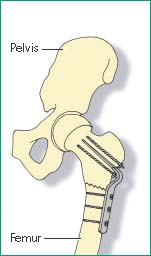
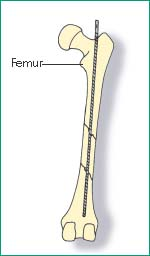
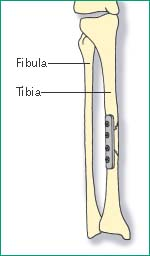
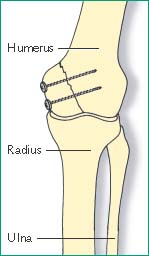
| In trochanteric or subtrochanteric fractures, the surgeon may use a hip pin or nail, with or without a screw plate. A pin or plate with extra nails stabilizes the fracture by impacting the bone ends at the fracture site. | In an uncomplicated fracture of the femoral shaft, the surgeon may use an intramedullary rod. This device permits early ambulation with partial weight bearing. | Another choice for fixation of a long-bone fracture is a screw plate, shown here on the tibia. | In an arm fracture, the surgeon may fix the involved bones with a plate, rod, or nail. Most radial and ulnar fractures may be fixed with plates, whereas humeral fractures are commonly fixed with rods. |
 |  |  |  |
Equipment
Ice bag ▪ pain medication ▪ incentive spirometer ▪ compression stockings ▪ sequential compression device.
For a patient with a leg fracture, you may also need an overhead frame with trapeze, pressure-relief mattress, crutches or walker, and pillow; hip fractures may require abductor pillows.
Implementation
Preoperative Care
Verify the doctor’s orders.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.4
Reinforce the doctor’s explanation of the procedure, and answer the patient’s questions. Ensure that the patient has signed a consent form, according to your facility’s policy.5
Perform a comprehensive pain assessment using techniques appropriate for the patient’s age, condition, and ability to understand.6
Assess the patient for pain and administer pain medication, as prescribed, using safe medication administration practices. Perform a follow-up pain assessment and notify the doctor if pain isn’t adequately controlled.6
Tell the patient what to expect during postoperative assessment and monitoring.
Teach the patient how to cough, deep breathe, and use an incentive spirometer to reduce the risk of postprocedure pneumonia.7
Prepare the patient for proposed exercise and progressive ambulation regimens, if necessary.
Conduct a preprocedure verification to make sure that all relevant documentation and related information or equipment is available and correctly identified to the patient’s identifiers.8
Verify that the laboratory and imaging studies have been completed, as ordered, and that the results are in the patient’s medical record. Notify the doctor of any unexpected results.8
Ensure that the patient has had nothing by mouth for 6 to 8 hours before the procedure, except in emergency situations.
Verify that the patient has patent IV access to administer prophylactic antibiotics (commonly administered 1 hour before the incision or 2 hours before if vancomycin or fluoroquinolones are prescribed), IV fluids, and blood products, as prescribed.9,10
Postoperative Care
Get Clinical Tree app for offline access



