Inflammatory Heart Disease
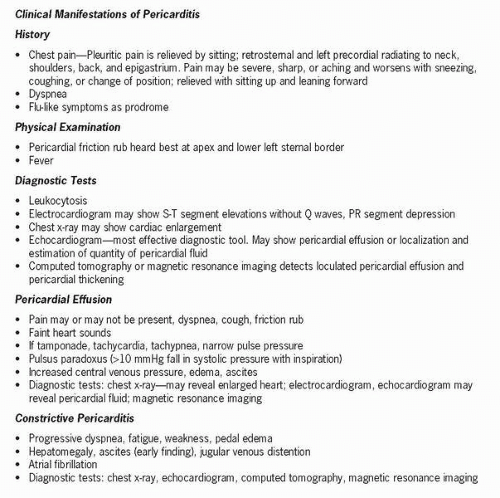
Pericarditis, or inflammation of the pericardium, may be a primary condition or result from secondary disease. It can be caused by viral, bacterial, or fungal infections or by neoplasm or uremia. Males under 50 years old are most commonly affected. Other causes include systemic disease such as autoimmune and connective tissues diseases, such as rheumatoid arthritis, systemic lupus erythematosus, or rheumatic fever, and trauma due to radiation, chest injury, open heart surgery, or pacemaker insertion. It may also be the result of diseases of adjacent structures, myocardial infarction, and pulmonary disease. Pericarditis may spread from or to the myocardium.
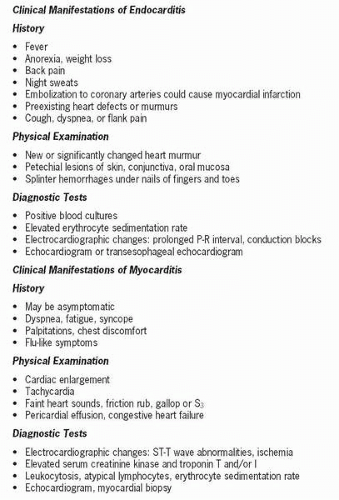
Infective endocarditis, formerly known as bacterial endocarditis, is an infection of the endocardium, or inner lining of the heart, and most often involves the valves. Before the era of antibiotics, it was a lethal disease. It is now relatively rare, although there are approximately 5,000 to 8,000 new cases in the United States each year. Two forms of endocarditis are described: subacute and acute. The subacute form has a longer course, a more insidious onset, less toxicity, and causative organism of low virulence, commonly Streptococcus viridans. It responds well to treatment. The acute form has a shorter course, more rapid onset, more toxicity, and more virulent organism, commonly caused by Staphylococcus aureus. It can cause death within days or weeks if untreated.
Infective endocarditis occurs when turbulent blood flow in the heart allows causative organisms to grow on damaged valves or other endothelial surfaces. Conditions predisposing individuals to endocarditis have changed with the decreasing incidence of rheumatic heart disease and recognition
and treatment of mitral valve prolapse. Risk factors include congenital and degenerative heart diseases that damage valves and endothelial surfaces. Individuals with artificial valve replacement may develop endocarditis. Organisms may gain entry to the bloodstream during intrusive procedures such as dental procedures, gynecological examinations, and placement of urinary catheters. Intravenous drug abusers are at high risk. Organisms other than bacteria can be involved, such as gram-negative bacilli, fungi, and yeast, particularly in the immunocompromised individual.
and treatment of mitral valve prolapse. Risk factors include congenital and degenerative heart diseases that damage valves and endothelial surfaces. Individuals with artificial valve replacement may develop endocarditis. Organisms may gain entry to the bloodstream during intrusive procedures such as dental procedures, gynecological examinations, and placement of urinary catheters. Intravenous drug abusers are at high risk. Organisms other than bacteria can be involved, such as gram-negative bacilli, fungi, and yeast, particularly in the immunocompromised individual.
 Infective endocarditis, formerly known as bacterial endocarditis, is an infection of the endocardium, or inner lining of the heart, and most often involves the valves.
Infective endocarditis, formerly known as bacterial endocarditis, is an infection of the endocardium, or inner lining of the heart, and most often involves the valves.Myocarditis is a focal or diffuse inflammatory process involving the myocardium and resulting from a variety of etiological agents, including pathological organisms (mainly viruses but also fungi, parasites, and rickettsiae), radiation, toxins, systemic diseases such as systemic lupus erythematosus or rheumatic fever, and immune reactions. It often follows an upper respiratory infection but may also occur from chemotherapy drugs, radiation, or cocaine abuse. It is frequently associated with pericarditis and endocarditis. The most common causative organism is Coxsackievirus A and B. It is also thought to be caused by exposure to chemical or physical agents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree