Inflammatory Bowel Disease: Part II
Crohn’s disease, a disease that is characterized by periods of exacerbations and remissions, can involve any segment of the bowel. The etiology of this disease is largely unknown. Exacerbations are painful and sometimes require surgery or hospitalization. Management is aimed at providing symptomatic relief.
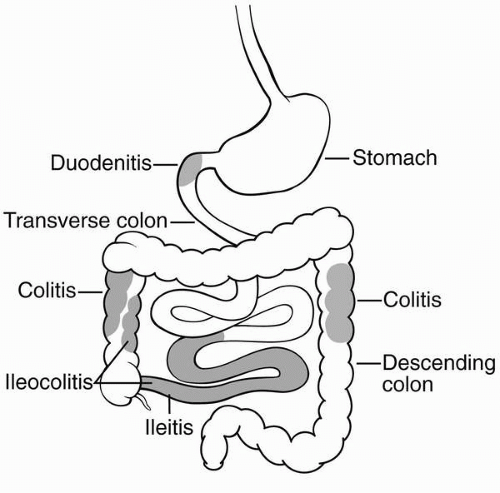 Figure 47-1 Areas (shaded) frequently affected by Crohn’s disease. |
Crohn’s disease is an insidious, slowdeveloping, chronic, progressive disorder that involves the full thickness of the bowel wall. The pattern of ulceration is linear and penetrating, skipping over regions of normal tissue. Typically occurring in the distal colon, 30% of cases involve the small intestine alone and 40% the proximal ascending colon alone. Ulceration and inflammation can, however, involve any segment of the
gastrointestinal tract from mouth to anus with a characteristic “skipping” pattern of sharply demarcated areas of diseased and normal bowel segments adjacent to each other.
gastrointestinal tract from mouth to anus with a characteristic “skipping” pattern of sharply demarcated areas of diseased and normal bowel segments adjacent to each other.
Crohn’s disease is a recurrent disease of the intestines that causes right lower quadrant or periumbilical pain, especially after eating. It is characterized by a colicky pain relieved with defecation. Patients present complaining of low-grade fever, abdominal pain, a number of liquid bowel movements per day, abdominal tenderness, malaise, weight loss, and fatigue. The diarrhea is nonbloody and intermittent. A palpable mass may be present in the lower abdomen because of inflamed and thickened loops of intestine. Recurrent bouts of diarrhea and progressive disease produce weight loss and malabsorption syndromes that include anemia from inadequate absorption of iron, folate, vitamin B12, and other vitamin deficiencies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



